To compare the double row technique versus the single row technique for arthroscopic rotator cuff repair, in order to assess whether there are clinical differences.
MethodsSystematic review of randomized clinical trials comparing the clinical results of the double-row technique versus the single-row technique in arthroscopic rotator cuff repair. Demographic, clinical, and surgical variables were analyzed, including functional scores, tendon healing rate, and re-tear rate.
ResultsThirteen randomized clinical trials were selected. 437 patients in the single row group (50.7%) and 424 patients in the double row group (49.3%) were analyzed. No significant differences were found between the two groups in terms of age (P = .84), sex (P=.23) and loss to follow-up (P=.52). Significant differences were found for the better results of the double row technique at the UCLA level (P=.01). No significant differences were found on the Constant-Murley scale (P=.87) or on the ASES scale (P=.56). Similarly, there was a higher healing rate (P=.006) and less risk of rotator cuff re-tears with the double row technique (P=.006).
ConclusionsIn rotator cuff repair, the double row technique was found to be superior to the single row technique in terms of better UCLA score, better tendon healing rate, and lower re-tear rate. No clinically significant differences were found on the Constant-Murley scale or on the ASES scale.
Comparar la técnica doble hilera versus la técnica de hilera simple para la reparación artroscópica del manguito rotador, con el fin de valorar si hay diferencias clínicas, funcionales y radiológicas.
MétodosRevisión sistemática de ensayos clínicos aleatorizados que comparen los resultados clínicos de la técnica doble hilera versus la técnica de hilera simple en la reparación artroscópica del manguito rotador. Se analizaron las variables demográficas, clínicas y quirúrgicas, incluyendo escalas funcionales, tasa de curación del tendón y tasa de re-rupturas.
ResultadosTrece ensayos clínicos aleatorizados fueron seleccionados. Se analizaron 437 pacientes en el grupo de hilera simple (50,7%) y 424 pacientes en el grupo de doble hilera (49,3%). No se encontraron diferencias significativas entre ambos grupos en lo referente a la edad (p=0,84), sexo (p=0,23) y pérdidas durante el seguimiento (p=0,52). La técnica de doble hilera obtuvo mejores resultados en la escala UCLA, siendo esta diferencia estadísticamente significativa (p=0,01). No se encontraron diferencias significativas en la escala Constant-Murley (p=0,87) ni en la escala ASES (p=0,56). Del mismo modo, hubo una mayor tasa de curación (p=0,006) y menor tasa de re-rupturas del manguito rotador con la técnica de doble hilera (p=0,006).
ConclusionesEn la reparación del manguito rotador se halló que la técnica doble hilera es superior a la técnica hilera simple en términos de una mejor puntuación en la escala UCLA, una mejor tasa de curación del tendón y una menor tasa de re-rupturas. No se encontraron diferencias significativas a nivel clínico en la escala Constant-Murley ni en la escala de ASES.
Arthroscopic repair of rotator cuff tears is a common procedure that offers advantages over open surgery which include: a minimally invasive approach, smaller skin incisions, absence of deltoid detachment, and less soft tissue dissection.1 Ideally, rotator cuff repair should provide stable fixation and minimise gap formation between the tendon and bone during the healing process.2 The single-row technique for rotator cuff tear repair has been the standard technique, although numerous studies have reported a higher rate of re-tears and incomplete tendon healing.3,4 The re-tear rate with the single-row technique ranges from 25.9% to 56%, whereas the re-tear rate with the double row technique ranges from 14.2% to 27%.4,5 One possible explanation for the high rate of repair site failure is that the single-row technique does not fully recreate the native tendon footprint insertion on the greater tuberosity, leading to incomplete anatomical healing.3,5 It is estimated that with the single-row technique, an average of 52.7% of the rotator cuff footprint remains uncovered.3
The double row technique has been advocated as a means of increasing the contact area between the rotator cuff and the bone bed. Theoretically, this technique incorporates medial and lateral anchors, which increases the initial coverage of the tendon–bone junction.6 Restoring the anatomical footprint may improve healing of the tendon–bone interface and the mechanical strength of repaired tendons.7 Good clinical outcomes have been published for arthroscopic rotator cuff repair using a double row technique.8,9 Several studies have also reported anatomical and biomechanical advantages of the technique compared with the single-row technique.7–9 The results of these studies indicate that the double row technique provides a better healing environment for the tendon and bone for rotator cuff repairs than the single-row technique.2,10–12 However, there are also studies indicating no clinical differences in postoperative outcomes between the two techniques.13,14 Currently, there is still controversy regarding which of the two techniques offers better results in rotator cuff repair. With the hypothesis that the double row technique presents better functional outcomes and a lower re-tear rate, the primary objective of this study was to compare the double row technique versus the single-row technique for rotator cuff repair through a systematic review of randomised clinical trials.
Materials and methodsSystematic reviewThis meta-analysis was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement,15 and the systematic review followed the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions.16 The electronic search was conducted between July and September 2022. Studies published up to September 15, 2022, that evaluated clinical and radiological outcomes in patients undergoing rotator cuff repair using the single-row or double row technique were sought. The search terms used in English were: 1. Rotator cuff repair, 2. Single-Row, 3. Double row, 4. Randomised Controlled Trials (RCT).
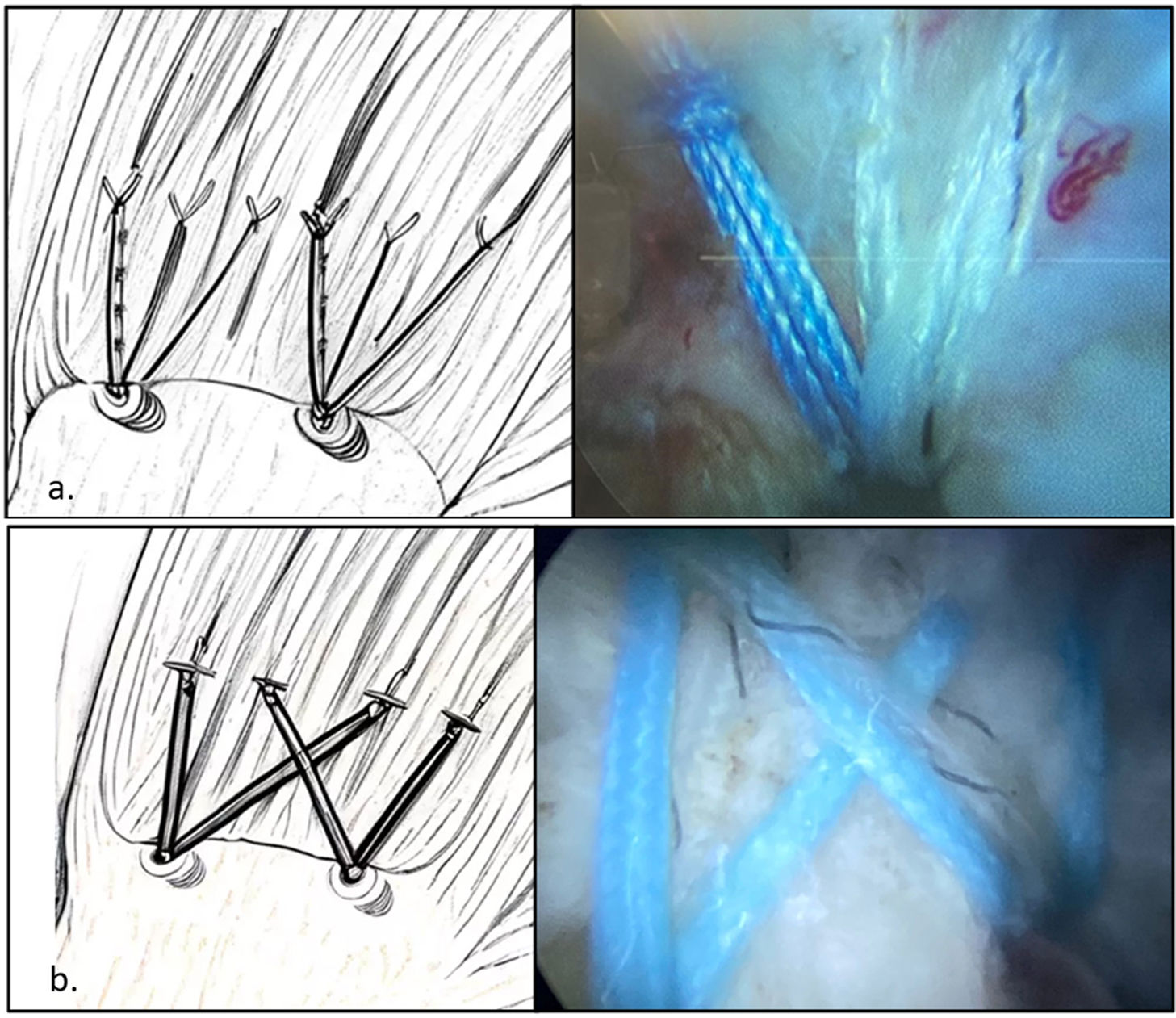
Inclusion and exclusion criteriaThe inclusion criteria for the studies were as follows: (1) studies published between 2000 and 2022; (2) randomised clinical trials (RCTs) comparing the two surgical procedures (single-row technique or double row technique) (Fig. 1); (3) studies with a minimum follow-up of 12 months, and (4) studies that report at least one outcome related to the variables studied. Studies with the following were excluded from the meta-analysis: (1) lack of comparative data; (2) biomechanical or in vitro studies; (3) papers that do not present their results through means with standard deviations; (4) studies with duplicate data, and (5) conference presentations, editorials, and abstracts.
Study selectionThe titles and abstracts of the articles found through the systematic search were evaluated, and relevant studies were selected for a full review. If the abstract did not provide sufficient data to determine the eligibility, the full article was reviewed. References were also cross-referenced to identify papers potentially missed by the electronic search. When analysing and organising the studies, the country and city of the hospital or institution where the surgical interventions were performed, the name of the surgeon in the studies, and the evaluation period were verified to identify duplicate patient cohorts. If the same patient cohort was evaluated in more than one study, the last study with the longest follow-up period was included, while the others were excluded.
Following PRISMA guidelines, two independent reviewers (J.D.M. and M.S.) evaluated titles, abstracts, and full-text articles. If there was a debate about the inclusion of an article, a third independent reviewer (J.H.N.) was consulted.
Data extraction: variables analysedData were extracted from the main texts and supplementary appendices. Two researchers independently extracted data from the studies included in the final analysis. A predefined data extraction form was used for data extraction. Any unresolved disagreements between the two researchers were reviewed by a third researcher (J.H.N.).
The data obtained were divided as follows: (I) General characteristics, including first author, year of publication, clinical trial number (NCT), included patients, age, sex, suture type (single-row or double row), follow-up time, and loss to follow-up. (II) Postoperative clinical variables collected included the American Shoulder and Elbow Surgeons (ASES) score, the Constant-Murley Shoulder Score, and the University of California, Los Angeles (UCLA) score. (III) Finally, tendon healing and re-rupture rates after surgery were recorded, which were measured by postoperative ultrasound or MRI at the end of follow-up.
Quality assessmentThe quality of the RCTs was assessed using Review Manager (RevMan) software version 5.3 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, 2014) to assess the risk of bias. The assessment methods consisted of the following steps: random sequence generation, concealed allocation, assessment of blinding, incomplete outcome data, and selective reporting of results. Scores in these domains are translated into an overall assessment of the overall risk of bias for a given RCT: (I) “low risk of bias”; (II) “unclear risk of bias”; or (III) “high risk of bias.”
Statistical analysisDescriptive statistics were mean and SD for continuous variables and count and percentage for categorical variables. The meta-analysis was performed using the Cochrane Community Review Manager software (version 5.3). For binary variables, the odds ratio (OR) was used for assessment, while for continuous variables, the standard mean difference (SMD) with a 95% confidence interval (CI) was applied. Study heterogeneity was estimated using the I2 test. The random-effects inverse variance model was applied. Statistical significance was defined as a p value <.05.
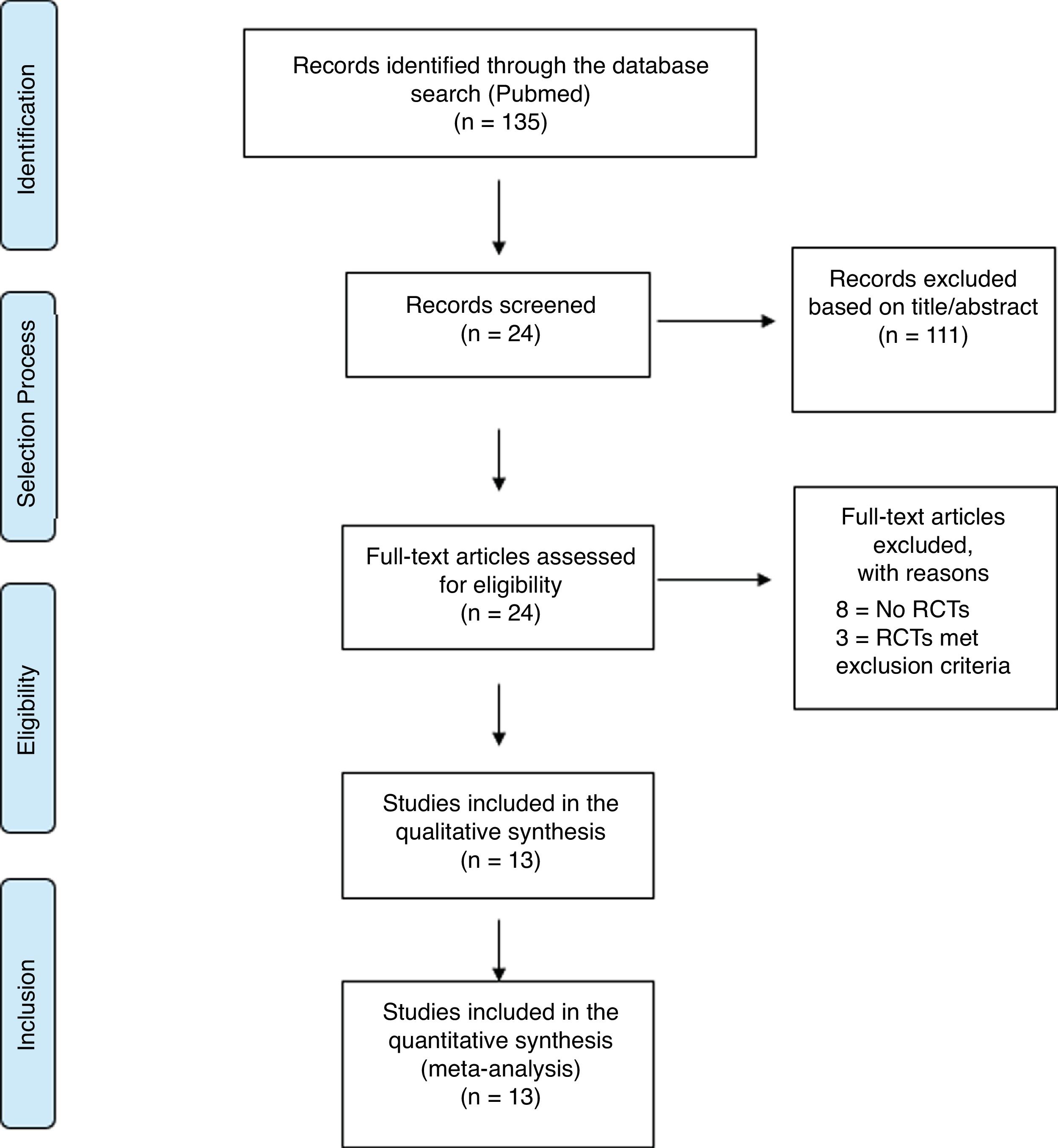
ResultsReview of the literatureThe initial search returned a total of 135 studies, of which 111 were excluded from the present systematic review after reading the title and/or abstract. Of the remaining 24 studies, and after reviewing the full text, 11 were excluded, leaving 13 RCTs for inclusion in the final analysis17–29 (Fig. 2). Fig. 3 provides a summary of the risk of bias.
The characteristics of each study are contained in Table 1. The meta-analysis included a total of 1139 patients. However, at the end of follow-up for the final analysis, 24.4% (278 patients) were lost. No statistically significant differences were found in patient loss to follow-up (OR: 1.16; 95% CI: .74–1.83; p=.52) with no heterogeneity (I=.0%; p=.94).17–29
Summary of the studies included in this systematic review.
| Study | Year | Number of patients | Type of DR | Age (mean) | Follow-up (months | Follow-up scales | ||
|---|---|---|---|---|---|---|---|---|
| SR | DR | SR | DR | |||||
| Imam et al. | 2020 | 40 | 40 | Transosseous equivalent | 61.6 | 60 | 36 | UCLA and Constant scale |
| Yamakado et al. | 2019 | 53 | 53 | Transosseous equivalent | 65.8 | 65.4 | 28.6 | UCLA scale |
| Barber et al. | 2016 | 20 | 20 | Transosseous equivalent | 57 | 55 | 27 | Constant and ASES |
| Franceschi et al. | 2016 | 30 | 28 | Double row suture | 61.8 | 58.9 | 26.8 | UCLA scale |
| Nicholas et al. | 2016 | 25 | 24 | Transosseous equivalent | 61 | 65 | 26 | ASES scale |
| Carbonel et al. | 2012 | 80 | 80 | Double row suture | 60.8 | 61.6 | 33.5 | UCLA, Constant and ASES scales |
| Lapner et al. | 2012 | 48 | 42 | Double row suture | 56 | 57.8 | 24 | Constant and ASES scales |
| Ma et al. | 2012 | 80 | 80 | Double row suture | 55.79 | 55.21 | 24 | UCLA and ASES scales |
| Khon et al. | 2011 | 31 | 31 | Double row suture | 61.6 | 61.1 | 32.8 | UCLA, Constant and ASES scales |
| Aydin et al. | 2010 | 34 | 34 | Transosseous equivalent | 59 | 57 | 36 | Constant scale |
| Burkus et al. | 2009 | 20 | 20 | Transosseous equivalent | 56 | 57 | 12 | UCLA, Constant and ASES scales |
| Grasso et al. | 2009 | 40 | 40 | Transosseous equivalent | 58.3 | 55.2 | 24.8 | Constant scale |
| Franceschi et al. | 2007 | 30 | 30 | Double row suture | 63.5 | 59.6 | 22.5 | UCLA scale |
ASES: American Shoulder and Elbow Surgeons; Constant: Constant-Murley scale; DR: double row; SR: single row; UCLA: Universidad of California in Los Angeles.
A total of 437 patients in the single-row group (50.7%) and 424 patients in the double row group (49.3%) were analysed. The mean age was 59.9 years (SD: 3.1) in the single-row group and 59.1 years (SD: 3.6) in the double row group. There were no statistically significant differences between the two groups (SMD: 0.02; 95% CI: −.22 to .27; p=0.84).8,20,24,25,27,28 No statistically significant differences were found regarding patient gender (OR: .83; 95% CI: .61–1.13; p=.23). Appendix A shows variables studied in the articles analysed, such as the types of rupture, the number of tendons involved, the size of the rupture, and fatty atrophy. No article reported statistically significant differences between the two groups for these variables.
Clinical resultsThe most frequently used scales were the UCLA scale, the Constant-Murley scale, and the ASES scale.17–21 Four studies used at least two of these functional scales,17,18,26,27 and three studies used all three (Table 1). Significant differences in outcomes were found with the double row technique for the UCLA scale (SMD: .22; 95% CI: .05–.38; p=.01), with no heterogeneity (I=00%; p=.89).17–19,21,23,25,26,28 (Fig. 4a) However, no significant differences were found at the Constant-Murley scale level (SMD: −.02; 95% CI: −0.21 to .18; p=.87) with mild heterogeneity (I2=32%; p=.16),17,19,20,22,25,27–29 (Fig. 4b) nor at the ASES scale level (SMD: .05; 95% CI: −.13 to .24; p=.56) with zero heterogeneity (I2=0%; p=.48)19,22,24–28 (Fig. 4c).
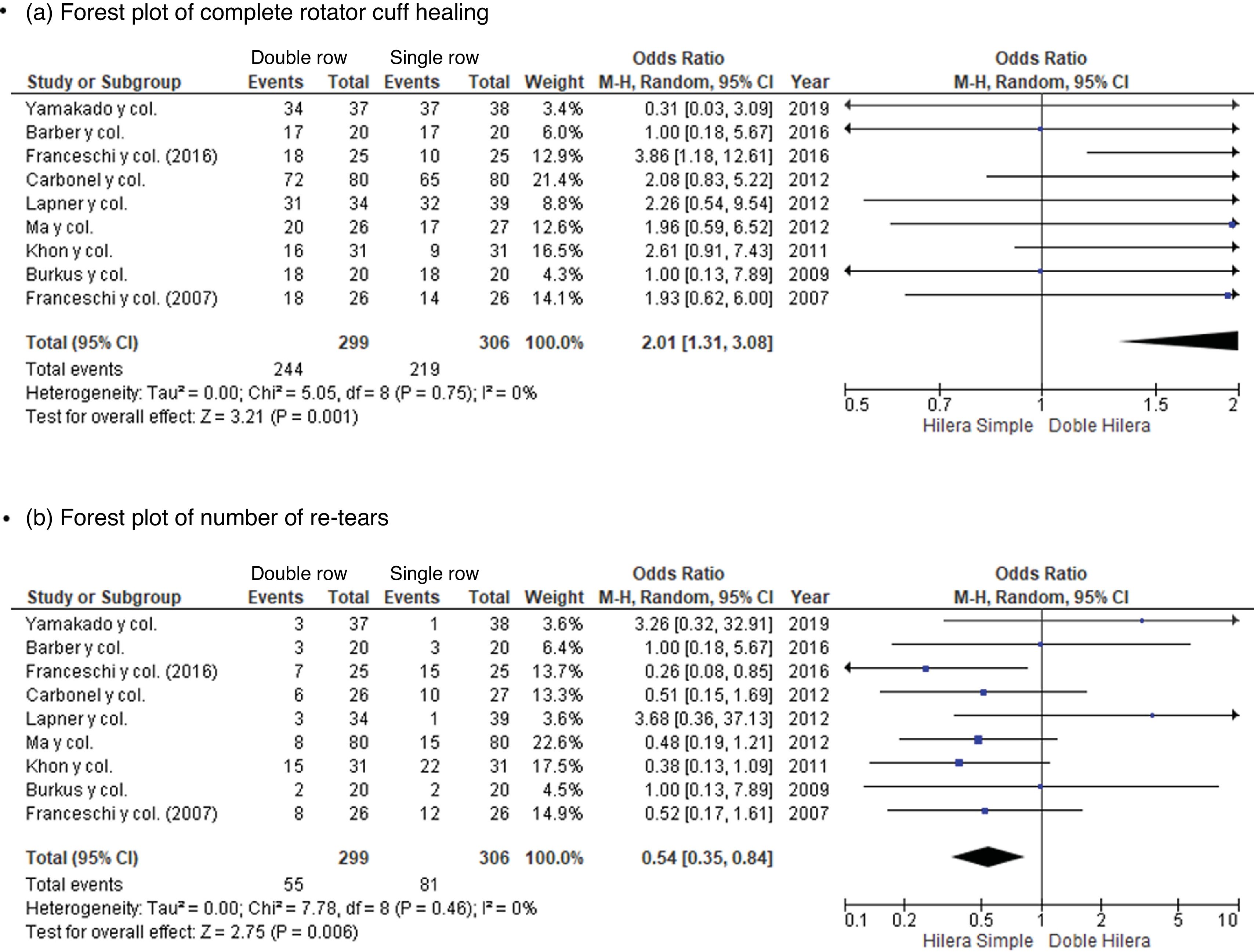
Surgical resultsSignificant differences were found with a higher healing rate at the level of the rotator cuff with the double row technique (OR: 1.85; 95% CI: 1.19–2.87; p=.006) with zero heterogeneity (I=0%; p=.46)18,19,21–23,25–28 (Fig. 5a). Likewise, significant differences were found, with a lower risk of rotator cuff re-tears with the double row technique (OR: 1.54; 95% CI: .35–.84; p=.006) with no heterogeneity (I=.0%; p=.46)18,19,21–23,25–28 (Fig. 5b).
DiscussionThe main findings of the study were that there were no significant differences between the single-row and double row groups in clinical outcomes based on the Constant-Murley score or the ASES score. However, the UCLA score and tendon healing were significantly better for the double row technique than for the single-row technique.
No statistically significant differences were found between the two groups in terms of age, sex, and loss to follow-up, thus limiting demographic and loss bias. Study selection and homogeneity play an important role in quality control when performing a meta-analysis.30 Regarding clinical outcomes, significant differences were only found at the level of the UCLA score. This evidence is consistent with previous meta-analyses.11,31 Sobhy et al.,31 in their meta-analysis of 7 RCTs, found a better UCLA score in double row patients (SMD: .69; 95% CI: .19–1.20; p=.007) with no heterogeneity (I=.0%; p=.84). Ying et al.,11 in their meta-analysis of 11 RCTs, also found a better UCLA score in double row patients (SMD: .66; 95% CI: .20–1.13; p=.005) with no heterogeneity (I=0%; p=.89). It should be noted that only 2 RCTs (Imam et al.17 and Carbonel et al.25) had found a difference at the level of the UCLA score between both techniques, these two studies being with a large number of patients studied (Carbonel et al. with 80 patients per group, and Imam et al. with 40 patients per group). In both our meta-analysis and that of Sobhy et al.,31 and Ying et al.11 the study by Carbonel et al.25 was among the studies analysed. This raises the observation that appropriately calculated sample sizes can yield significant differences in functional outcomes, and that most studies, even RCTs, have small sample sizes.18–24,26–29 Excluding the studies by Carbonel et al.,25 and Iman et al.,17 the remaining RCTs analysed did not find clinical differences at the level of any of the three functional scales.18–24,26–29 There are meta-analysis-type studies that disagree with our findings.13,17 Ponugoti et al.,13 in their meta-analysis of 14 studies (6 RCTs, 2 prospective studies, and 6 retrospective studies), found no significant differences between the two techniques on any of the three scales studied in our study (UCLA, Constant, and ASES). However, the majority of their patient sample was from retrospective studies. Sheibani-Rad et al.,14 in their meta-analysis of 5 RCTs, also found no differences between the two techniques on the UCLA, Constant, and ASES scales. However, the RCTs by Carbonel et al.,25 and Iman et al.17 were not included in their study.
There was a higher rate of healing at the rotator cuff level with the double row technique. This finding is consistent with the literature, both with previous meta-analyses and with other types of prospective non-randomised studies and retrospective studies.11,32,33 In their meta-analysis, Ying et al.11 found a higher rate of healing at the rotator cuff level with the double row technique (OR: 1.79; 95% CI: 1.19–2.68; p=.005) with no heterogeneity (I2=0%; p=.78), compared with the single-row technique. Hantes et al.,32 in their prospective non-randomised study of the mid-term radiological and clinical outcomes between single-row and double row fixation techniques for arthroscopic rotator cuff repair in patients younger than 55 years, concluded that the double row repair technique provided better tendon healing. Similarly, Gartsman et al.,33 reported a significantly higher tendon healing rate (as determined by ultrasonographic examination) when using a double row transosseous arthroscopic repair, compared with single-row arthroscopic repair. Xu et al.,34 in their meta-analysis, found in the pooled results a statistically significantly higher incidence of re-ruptures in the single-row repair group (40.2%) compared with the double row group (23.8%). It should be noted that healing and re-rupture rates were measured in the studies included in the meta-analysis18,19,21–23,25–28 and in the studies discussed above32–34 using postoperative ultrasound or MRI. Studies may have clinical outcomes assessed with functional scales that differ from radiological outcomes assessed with MRI or ultrasound. Some studies have shown that improvement in pain and shoulder function does not always correlate with the integrity of the repair.35 However, the literature also reports that patients with improved tendon healing are generally more likely to experience better clinical outcomes.35,36
Some limitations of the present study should be noted. First, the number of included studies is small, which may result in insufficient data. However, only RCTs were included, which is a strength. RCTs can optimise follow-up and data quality, with low selection bias and confounding factors.30 Second, the relatively short follow-up time in the included studies, with only three studies with a follow-up of 36 months. Currently, the comparative data available between single-row and double row techniques for rotator cuff repair are limited. Furthermore, regarding the double row technique, the analysis did not separate whether it was a double row technique or an equivalent transosseous technique, as this was not the current objective of the study. Further high-quality studies are required to evaluate the clinical outcomes and cost-effectiveness of these different techniques.
In conclusion, the double row technique was found to be superior to the single-row technique for rotator cuff repair in terms of a better UCLA score, a better tendon healing rate, and a lower re-rupture rate. No clinically significant differences were found on the Constant-Murley score or the ASES score.
Level of evidenceLevel of evidence I.
FundingWe did not receive any financial support from any institution for the preparation of this article.
Conflict of interestsThe authors have no conflict of interests to declare.
| Study | Type of tearDegenerative/traumatic | Type of tear<3cm/>3cm | Number of tendons involved (only supraspinatus) | Fatty atrophy | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SR | DR | p value | SR | DR | p value | SR | DR | p value | SR | DR | p value | |
| Imam et al. | 37/3 | 36/4 | .69 | 17/23 | 19/21 | .074 | NM | NM | NM | NM | NM | NM |
| Yamakado et al. | NM/8 | NM/4 | .17 | NM | NM | NM | NM | NM | NM | NM | NM | NM |
| Barber col. | NM | NM | NM | NM | NM | NM | NM | NM | NM | NM | NM | NM |
| Franceschi et al. | NM/7 | NM/8 | >.05 | 11/14 | 12/13 | >.05 | 10 | 10 | .05 | NM | NM | NM |
| Nicholas et al. | NM | NM | NM | 8/12 | 7/9 | .89 | NM | NM | NM | NM | NM | NM |
| Carbonel et al. | NM | NM | NM | 51/29 | 53/27 | .74 | NM | NM | NM | NM | NM | NM |
| Lapner et al. | NM | NM | NM | NM | NM | NM | NM | NM | NM | NM | NM | NM |
| Ma et al. | NM | NM | NM | 19/8 | 17/9 | .69 | NM | NM | NM | NM | NM | NM |
| Khon et al. | NM | NM | NM | NM | NM | NM | NM | NM | NM | NM | NM | NM |
| Aydin et al. | NM | NM | NM | NM | NM | NM | NM | NM | NM | NM | NM | NM |
| Burkus et al. | NM | NM | NM | 18/2 | 15/5 | NM | NM | NM | NM | NM | NM | NM |
| Grasso et al. | NM | NM | NM | NM | NM | NM | 19 | 20 | .80 | 37 | 35 | .27 |
| Franceschi et al. | NM | NM | >.05 | NM/26 | NM/26 | >.05 | 12 | 15 | >.05 | NM | NM | NM |
DR: double row; SR: single row; NM: not mentioned.