Despite the recognized importance of the anterolateral ligament (ALL) in rotational stability of the knee, some studies still deny its role and even its existence. We studied the prevalence of the ALL in a Caucasian population, as well as its characteristics and anatomical relationships.
Materials and methodsThe study was performed on 20 knees from 10 embalmed cadavers. A lateral approach, as described by Steven Claes, was used and the relations of the ALL with the lateral epicondyle, lateral inferior genicular artery, lateral meniscus, Gerdy's tubercle and fibular head were recorded. Its length and its width were also measured.
ResultsThe ALL was identified in 16 knees. Its origin was at a distance inferior to 1mm posterior and proximal to the lateral femoral epicondyle and insertion within a mean distance of 2.1±0.6mm from de tibial articular surface, 20.6±1.3mm from the Gerdy's tubercle and 20.3±1.2mm from the fibular head. In all cases ALL presented mutual fibers with the lateral meniscus. The length was 35.8±4.6mm and the width was 4.2±1.3/4.9±1.0/6.5±1.5mm at its proximal, middle and distal third, respectively. No difference was found between gender and the dimensions of the ligament.
ConclusionsThe ALL was found in 80% of the knees. Its origin is closely related to the lateral collateral ligament and its insertion is halfway between the fibular head and the Gerdy's tubercle. In all cases, we verified the connection between ALL and the lateral meniscus.
Aunque ha sido reconocida la importancia del ligamento anterolateral (ALL) en la estabilidad rotacional de la rodilla, algunos estudios siguen negando su existencia. Estudiamos la prevalencia del ALL en una población caucásica, así como sus características y relaciones anatómicas.
MétodosEl estudio se realizó en 20 rodillas de 10 cadáveres embalsamados. Se utilizó un abordaje lateral, como lo describe Steven Claes, y se registraron las relaciones del ALL con el epicóndilo lateral, la arteria genicular inferior lateral, el menisco lateral, el tubérculo de Gerdy y la cabeza del peroné. También se midió el ancho y el largo.
ResultadosEl ALL fue identificado en 16 rodillas. Su origen estaba a una distancia inferior a 1mm posterior y proximal al epicóndilo femoral lateral y su inserción a una distancia media de 2,1±0,6mm de la superficie articular tibial, 20,6±1,3mm de la tuberosidad de Gerdy y 20,3±1,2mm de la cabeza del peroné. En todos los casos se presentaban fibras mutuas con el menisco lateral. El largo fue de 35,8±4,6mm y el ancho fue de 4,2±1,3/4,9±1,0/6,5±1,5mm en su tercio proximal, medio y distal.
ConclusionesEl ALL se encontró en el 80% de las rodillas. Su origen está íntimamente relacionado con el ligamento colateral lateral y su inserción se encuentra a media distancia entre la cabeza del peroné y el tubérculo de Gerdy. En todos los casos comprobamos la conexión entre el ALL y el menisco lateral.
Recent studies on the anatomical and functional characteristics of the anterolateral ligament of the knee (ALL) have renewed the interest in this structure.1–3
Much importance has been given to the anterolateral complex deficiency in patients undergoing anterior cruciate ligament (ACL) reconstruction. Especially those who have specific risk factors that predispose them to an increased risk of ACL graft rupture, after an appropriately performed ACL reconstruction.4–5 Some of this risk factors are young age, high demand athletes, high grade pivot-shift and ACL revision procedure.4 In these patients, some authors choose to reinforce an ACL reconstruction with lateral extra-articular procedures, more commonly with Lemaire technique or reconstruction of the ALL.6–9 Also, this combined procedure was associated with a significantly lower rate of failure of medial meniscal repairs when compared with those performed at the time of isolated ACL reconstruction.10
However, knowledge about the ALL is controversial. Some researchers revealed difficulties in anatomic dissection of ALL, reporting the impossibility of differentiating it from the other structures of the anterolateral part of the knee, mainly from the articular capsule.1
Different anatomic characteristics are found in literature and even the nomenclature is not unanimous, including lateral capsular ligament,11 capsulo-osseous layers of the iliotibial tract,12 anterior band of the lateral collateral ligament (LCL)13 and anterior oblique band.14
Dissection method and preservation mode of the cadavers are the most common causes for the lack of congruence in different studies.1–2
With this work we have studied the prevalence of the ALL in a Caucasian population, as well as its characteristics and anatomical relationships.
Materials and methodsThe cadavers derived from body donation with informed consent, written and signed by donator himself in accordance with national decree of law and ethical norms.
The study was performed on 20 knees from 10 alcohol–glycerol embalmed cadavers (7 males and 3 females; mean age of 78 years (72–83 years). Our exclusion criteria were pediatric age (under 18 years), past knee surgery, severe lower limb deformities and any type of previous lower limb dissection. All knees were dissected by a last year orthopedic resident and a knee specialist orthopedic surgeon. A lateral approach of the knee as described by Claes et al.,15 was used. Dissection begun with a curvilinear incision proximal to the lateral epicondyle and extending distally between the fibular head and Gerdy tubercle. After iliotibial band (ITB) was visualized, a transverse incision was made approximately 6–8cm proximal to the lateral epicondyle. The ITB was then reflected distally. Careful reflection of the ITB is essential in identification of the ALL, especially in the region of lateral epicondyle where the proximal ALL is closely adhered to the ITB. The reflection of the ITB was then taken further distally until its insertion onto the Gerdy's tubercle, and the underlying adipose tissue was removed.
When the lateral collateral ligament (LCL) was palpated, the leg was internally rotated with a flexed knee, to enhance the visualization of ALL. We observed if there was dense fibrous tissue, that ran superficial to the LCL in the anterolateral capsule the knee, which corresponded to the ALL.
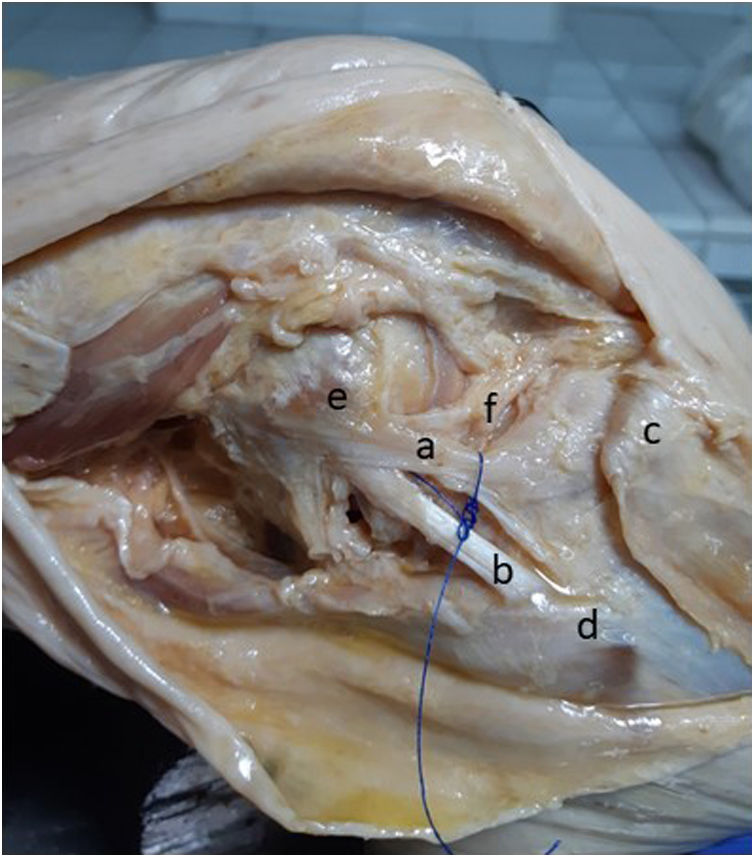
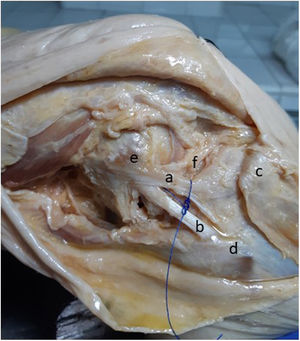
When the ALL was found, its relations with the lateral epicondyle, lateral inferior genicular artery, lateral meniscus, Gerdy's tubercle and fibular head were noted (Fig. 1). Its origin and insertion were documented, and its length (from its insertion points) and its width (in its proximal, middle and distal third), were measured on knee extension using digital calipers (Neiko 01407A Electronic Digital Caliper).
Statistical analysis was performed using IBM SPSS statistics, version 25 (IBM Corp., USA®). Study data was summarized using descriptive statistics (mean, standard deviation, frequency, percentage). To compare the morphometric parameters of the ALL as well as the incidence between female and male, the Student t-test and Chi-squared tests were used. A p-value of <0.05 was considered significant.
ResultsThe ALL was identified as a distinct structure at the anterolateral part of the knee joint in 16 knees. Seven cadavers had the ALL in both knees, one had in the right knee and one in the left. Its origin was located posterior and proximal to the lateral femoral epicondyle in a mean distance inferior to 1mm. Running obliquely, the ALL inserts in the tibial plateau with a mean distance of 2.1±0.6mm from de articular surface, 20.6±1.3mm from the Gerdy's tubercle and 20.3±1.2mm from the fibular head. In all cases we verified the presence of fibers connecting the ALL with the body of the lateral meniscus. In 11 knees we identified the inferior lateral genicular artery crossing between the ALL and the lateral meniscus. The average length was 35.8mm±4.6mm and the average width was 4.2±1.3/4.9±1.0/6.5±1.5mm at its upper, middle and lower third, respectively. No statistical differences were found between knees of the same cadaver. There was also no statistical difference regarding incidence (p=.143) or dimensions (p=.192) of the ALL between male or female gender.
DiscussionPrevalence of the ALL in literature is quite variable, ranging from 40 to 100% in different studies.1,8,16,17 Some authors verified the presence of the ALL in most of the samples,17–19 others did not identify this ligament in even half of the specimens1,16 and others showing no evidence of this ligament at all.20–21 In most of those where the ALL was not found, the authors stated that a capsular thickening was visible on the middle third of the lateral colateral ligament (LCL) but could not identify any ligament structure. These contradictory results motivated us to conduct this morphometric study to analyze this ligament.
In our work, with the dissection technique described by Claes et al.,15 the ALL was found in 80% of the knees. Its origin was closely related to the LCL and its insertion was halfway between the fibular head and the Gerdy's tubercle. It was important to define these structures during dissection in order to predict the position of the ligament and find it more easily. In the work of Fardin et al.21 where they studied 15 cadaveric knees fixed in formalin solution at mesoscopic level, they didn’t find evidence of any ligament with the same anatomical features of other ligaments in the region. They concluded that the structure known as ALL would not necessarily be an individualized ligament but rather part of another structure of the knee being possibly an artifact of dissection. In a work of Cho et al.,1 with 64 Korean adult fresh frozen cadavers, the prevalence of ALL was 42.5%. They refered that ALL could be clearly distinguished from the capsule-osseous layer of the ITB. However, the anterior border was indistinct and appeared combined with the anterior joint capsule. They concluded that ALL could be a local thickening of the capsule, possibly due to external physical stress, naming it anterolateral “capsular” ligament. In our study, we believe we didn’t find the ALL in 4 cases because of two reasons, already mentioned as pitfalls in Daggett's22 surgical dissection technique. In specimens with poor tissue quality, the lack of constant flexion and internal rotation removes tension to the ALL being easier to accidentally damage it. Also, the failure to separate ITB from ALL, especially in the lateral epicondylar region where they are strongly adhered, can put at risk the identification of the ALL.
The length of the ligament measured in our work (35.8±4.6mm) agrees with other studies and also the width showed similar values.1,15,18,19 In all cases, we verified the connection between the ALL and the lateral meniscus, which could be one reason to the high rate of meniscal tears in association with ALL tear.23
Despite the close relation of ALL and inferior lateral genicular artery, we found no information concerning vascular lesion in ALL tear or reconstruction procedure. However, this fact should motivate even more careful haemostasis after anterolateral ligament reconstruction procedures, to avoid post-operative hemarthrosis.
Considering known differences in height and weight between genders, we did not find any significant variations regarding the dimensions of the ALL. This result is in conformity with most works, apart from a previous study by Daggett et al.,24 which referred different thickness and length between genders. This study also reported a reduced number of cases with the presence of ALL in both knees (15/56), what was not verified in our work. The fact that the elements responsible for the dissection already had experience in knee surgery, may be one of the reasons for the high percentage of ALL in our study.
Our results seem to match the results of other Caucasian populations.15,25 However, there are studies in these populations that refer the presence of ALL between 40 and 60%,16,17 similar to the results found in Asian populations.1,26 Therefore, it is possible that the variability of these numbers is due only to the greater number of studies carried out in different Caucasian populations or to the dissection technique used.
Adding an ALL reconstruction procedure to augment primary ACL reconstruction is a current hot topic. The recently published results from SANTY study group27 compared isolated ACL reconstruction and combined ACL+ALL reconstruction with a total of 86 matched pairs, they reported significantly better long-term ACL graft survivorship (96.5% vs. 82.6%; p=.0027) with no increased complications in ACL+ALL group.
The small sample size is a limitation of our study, however it is not very different from other works published in this area. Also, the histological analysis of the found structure could have provided important additional information for this work.
ConclusionsWith a uniform and careful dissection technique, it is possible to find ALL in most cases. Probably, it's time to move the discussion from the question of the existence to the assessment of the true role of this structure in knee stability. Better understanding of the isometry and mechanical properties of the ALL could give important information to the development of new reconstruction techniques of this structure and the correct indications to do it.
DeclarationsThe authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
EthicsTwenty lower limbs from 10 embalmed cadavers were subjected to routine dissection at the Unit of Anatomy, of Medicine Faculty of Porto. The cadavers derived from body donation with informed consent, written and signed by donator himself (Portuguese decree-law 271/99). Data on patients’ demographics were collected from donation records.
Level of evidenceLevel of evidence v.
Financial supportThere was no financial support from public, commercial, or non-profit sources.
Conflict of interestThe authors declare no conflict of interest regarding the research, authorship, and/or publication of this article.