The aim of this study was to determine the reliability of cone beam computed tomography to locate and take measurements of the mandibular canal, as well as the vestibular bone wall, in the planning of the bone graft surgery in the mandibular body.
Material and methodsA total of 11 mandibles from fresh cadavers were studied (22 hemi-mandibles, half of them with teeth). A CBTC and a surgical procedure for the lateralization of the lower dental nerve were performed with the aim of measuring the thickness of the vestibular table and the mandibular canal (MC) or lower dental nerve at 5, 15, and 25mm from the most posterior position of the mentonian hole.
ResultsThe results obtained in the study indicate that CBTC, being the best diagnostic tool currently available, still appears to be unreliable when compared to actual results. This discrepancy is a mean of 1.15mm as regards the thickness of the vestibular bone wall that covers the MC, and a mean of 0.3mm in relation to the thickness of the lower dental nerve.
DiscussionIt is important to know and assess these discrepancies in view of the multitude of surgical procedures that can be performed in this area, and in the vicinity of the lower dental nerve.
El objetivo de nuestro estudio fue determinar la fiabilidad del estudio tomográficopara localizar el conducto mandibular y tomar mediciones exactas del diámetro de dichoconducto y de la pared ósea vestibular, como mediciones principales en la planificación dela toma de injerto óseo de cuerpo mandibular.
Material y métodoSe estudiaron 11 mandíbulas (22 hemimandíbulas) de cadáver fresco, lamitad de ellas dentadas, a las cuales se les realizaron una CBTC y un procedimiento qui-rúrgico de lateralización del nervio dentario inferior con el objetivo de medir el grosor de latabla vestibular y el grosor del conducto mandibular o dentario inferior (CDI) a los 5, 15 y 25mm de la parte más posterior del agujero mentoniano.
ResultadosLos resultados obtenidos por nuestro estudio indican que el CBTC, siendo elmejor método diagnóstico disponible en la actualidad, aún presenta diferencias respecto ala realidad. Esta discrepancia es de 1,15mm de media con relación al grosor de la tabla óseavestibular que lo recubre y de 0,3m de media con relación al grosor del CDI.
DiscusiónConocer y valorar estas discrepancias es importante dada la multitud de procedi-mientos quirúrgicos que se pueden realizar en esta zona, y la vecindad con el nervio dentarioinferior.
Currently, the advances in implantology and its recognition as one of the most important therapeutic weapons in the field of Odontology have led to the need to use bone graft techniques for the provision of this tissue in certain areas for adequate implant rehabilitation.1–3
There is a wide range of techniques, some of which are performed in the anatomical area of the mandible. For the latter, the mandibular ramus and body grafts have been frequently mentioned in publications in recent years.4,5
The main noble structure in this area that must be carefully handled at all times is the intraosseous trajectory of the inferior dental nerve (IDN), located in the inferior dental canal (IDC).4
Thus, determining the location of this structure before surgery to avoid damage is essential for the planning of a mandibular body bone graft. Therefore, it is important to understand the reliability of the techniques that surgeons may implement.6
In some patients, the IDC cannot be identified using a panoramic X-ray.7,8 Besides, this technique does not allow for a three-dimensional assessment of the mandible. Towards the end of the last century, the development of IT software together with computed tomographies (CT scans) introduced a major breakthrough for clinicians. Currently, the CT scan technique provides the largest amount of data compared to other diagnostic techniques in relation to the planning of bone tissue surgery.6
Previous studies on the reliability of CT scans and cone beam computed tomographies (CBCT) for the planning and selection of mandibular dental implants of adequate diameter and length, specifically about their reliability for the correct measurement of the distance between the upper rim of the mandibular canal and the upper rim of the mandible, have indicated that some anatomical points and accidents (such as the mental foramen) are essential and may not be seen clearly.9–11
Based on this approach, the studies conducted present contradictory results.12,13 Our study was centred on the same area. However, instead of focusing on the coronal area of the IDC, we focused on the vestibular area. In this area, measurements must be based on a lower number and smaller anatomical accidents than those in the alveolar area. However, the potential consequences of an incorrect measurement are more serious in bone grafting surgery than in implant insertion surgery.4
The objective of our study was to determine the reliability of the tomography study (CBCT) to locate the IDC and take precise measurements of its diameter and of the vestibular bone wall, which are the main measurements for the planning of a mandibular body bone grafting surgery or any other kind of surgery in this area.
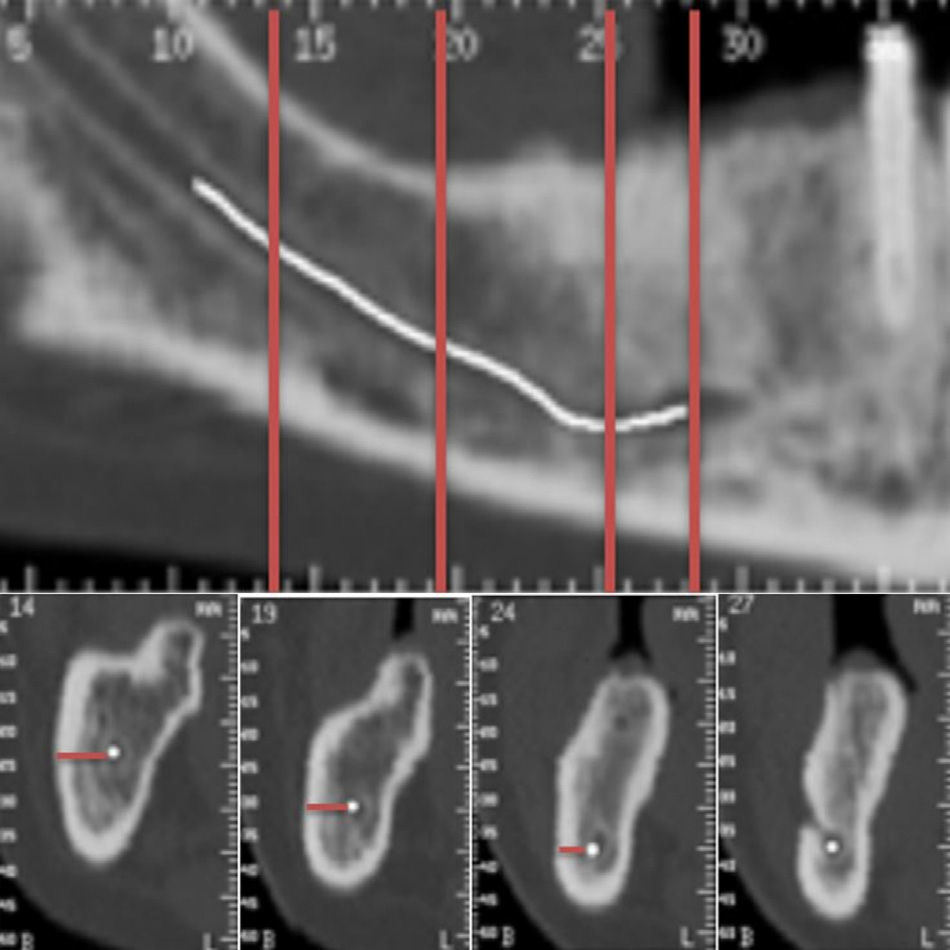
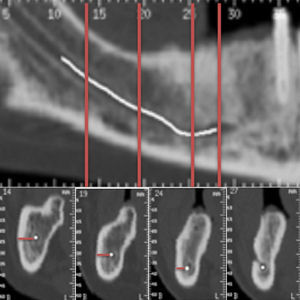
Material and methodThe study involved 11 mandibles (8 male subjects and 3 female subjects), 22 mandibular hemiarches, half of which had teeth, obtained from fresh corpses. The mandibles were requested, under due authorisation, by the Lavante Centre, which had been authorised by the Board of Andalucía. Before conducting the clinical study for the obtaining of actual measurements, these underwent a CBCT (GE Locus Ultra, GE Healthcare, United Kingdom). The images obtained were based on the following parameters: 120kV, 20mA, exposure time of 16s, and incisions of 154μm thick. Images were subject to a three-dimensional treatment, visualisation and measurement using the software Romexis Viewer (Planmeca OY, Finland) (Fig. 1).
The buccal distance was measured from the most lateral area of the IDC towards the vestibular area up to the bone buccal margin. This measurement was based on an incision perpendicular to the basal plane of the mandible in the following points: at 5, 15 and 25mm from the most rear part of the mandibular mental foramen (Fig. 1). The distance was always measured by the same person. The coronal-caudal diameter of the inferior dental canal was measured in the same way.
After the radiological measurement, the following protocol was carried out on the heads of the corpses to obtain the actual measurement of the distances between the most outer part of the IDC and the limit of the vestibular cortical bone of the mandible. After a surgical approach to this anatomical location, the mental foramen was identified and, on its rear part, at 5, 15 and 25mm, subsequent osteotomies were conducted (with a handpiece and a fissure drill under irrigation) to access the area to be measured (a fenestration was performed until nerve exposure, and the walls and the canal were subsequently measured using a gauge). Measurements were taken using a manual gauge, and one tenth of a millimetre was established as the base unit (Figs. 2 and 3).
As happened with the radiological measurements, only one independent observer, after the surgical preparation, measured each of the distances: the width of the vestibular bone wall of the IDC and the coronal-caudal diameter of the IDC.
Apart from these main measurements or variables, other measurements were collected in relation to the part of the mandible from which measurements were taken (right or left) and to the gender of the patient.
Finally, the data collected were included in a spreadsheet that was exported to SPSS v.14 (IBM Corp., USA) for their statistical analysis. The Mann–Whitney U statistical test was applied.
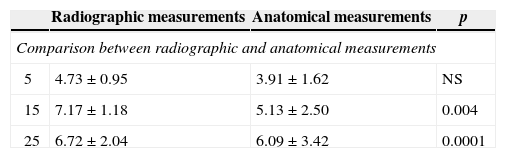
ResultsThe thickness of the vestibular wall of the IDC amounted to 4.73±0.95mm when radiographically measured and to 3.91±1.62mm when directly measured, at 5mm from the mental foramen. At 15 and 25mm from this point, on a radiographic level, the measurements were 7.17±1.18 and 6.72±2.04mm, respectively. When directly measured, these amounted to 5.13±2.50 and 6.09±3.42mm, respectively. The differences were statistically significant both at 15 and at 25mm from the mental foramen (Table 1).
Measurements related to the vestibular wall of the inferior dental canal, distal to MF in mm.
| Radiographic measurements | Anatomical measurements | p | |
|---|---|---|---|
| Comparison between radiographic and anatomical measurements | |||
| 5 | 4.73±0.95 | 3.91±1.62 | NS |
| 15 | 7.17±1.18 | 5.13±2.50 | 0.004 |
| 25 | 6.72±2.04 | 6.09±3.42 | 0.0001 |
| Male subject | Female subject | p | |
|---|---|---|---|
| Comparison between radiographic measurements by group | |||
| Gender | |||
| 5 | 4.77±1.03 | 4.60±0.75 | NS |
| 15 | 7.30±1.30 | 6.76±0.68 | NS |
| 25 | 6.78±2.35 | 6.55±1.30 | NS |
| Right | Left | p | |
|---|---|---|---|
| Hemimandible | |||
| 5 | 4.89±0.96 | 4.56±0.96 | NS |
| 15 | 7.48±1.37 | 6.86±0.89 | NS |
| 25 | 7.28±2.49 | 6.16±1.50 | NS |
| Male subject | Female subject | p | |
|---|---|---|---|
| Comparison between anatomical measurements by group | |||
| Gender | |||
| 5 | 4.03±1.72 | 3.56±1.36 | NS |
| 15 | 5.18±2.98 | 5.00±1.00 | NS |
| 25 | 6.16±3.98 | 5.88±1.23 | NS |
| Right | Left | p | |
|---|---|---|---|
| Hemimandible | |||
| 5 | 4.11mm±1.91 | 3.70mm±1.31 | NS |
| 15 | 5.53mm±3.81 | 4.72mm±1.63 | NS |
| 25 | 6.50mm±4.21 | 5.67mm±2.54 | NS |
NS: not statistically significant difference; MF: mental foramen.
The data used for the comparison of anatomical measurements based on gender or location, as well as the data used for the comparison of radiological measurements, present no statistically significant differences (Table 1).
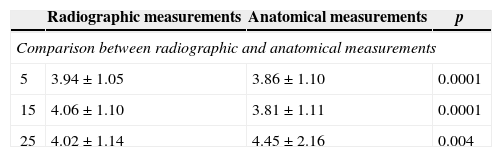
The diameter of the interior dental canal radiographically measured amounted to 3.94±1.05, 4.06±1.10 and 4.02±1.14mm, respectively, at 5, 15 and 25mm from the mental foramen. When directly measured, these presented the following results at 5, 15 and 25mm from the mental foramen, respectively: 3.86±1.10, 3.81±1.11 and 4.45±2.16mm. All the differences were statistically significant (Table 2).
Measurements related to the diameter of the inferior dental canal, distal to MF in mm.
| Radiographic measurements | Anatomical measurements | p | |
|---|---|---|---|
| Comparison between radiographic and anatomical measurements | |||
| 5 | 3.94±1.05 | 3.86±1.10 | 0.0001 |
| 15 | 4.06±1.10 | 3.81±1.11 | 0.0001 |
| 25 | 4.02±1.14 | 4.45±2.16 | 0.004 |
| Male subject | Female subject | p | |
|---|---|---|---|
| Comparison between radiographic measurements by group | |||
| Gender | |||
| 5 | 4.20±1.09 | 3.23±0.43 | 0.007 |
| 15 | 4.33±1.16 | 3.35±0.46 | 0.01 |
| 25 | 4.35±1.17 | 3.13±0.17 | 0.001 |
| Right | Left | p | |
|---|---|---|---|
| Hemimandible | |||
| 5 | 4.02±1.07 | 3.85±1.06 | NS |
| 15 | 3.92±1.15 | 4.20±1.08 | NS |
| 25 | 4.02±1.22 | 4.00±1.10 | NS |
| Male subject | Female subject | p | |
|---|---|---|---|
| Comparison between anatomical measurements by group | |||
| Gender | |||
| 5 | 3.38±1.13 | 2.18±0.24 | 0.01 |
| 15 | 3.60±1.16 | 2.93±0.12 | 0.003 |
| 25 | 4.22±1.35 | 3.10±0.49 | 0.01 |
| Right | Left | p | |
|---|---|---|---|
| Hemimandible | |||
| 5 | 3.26±1.32 | 2.84±0.86 | NS |
| 15 | 3.56±1.17 | 3.27±0.89 | NS |
| 25 | 4.00±1.16 | 3.83±1.43 | NS |
NS: not statistically significant difference; MF: mental foramen.
The data used for the comparison of anatomical measurements based on location did not present significant differences. However, in comparisons based on gender, female subjects did present a significantly smaller diameter of the IDC than male subjects, on both a radiological and an anatomical level (Table 2).
DiscussionAlthough the IDN presents only one sensible component, patients and clinicians consider its damage as a failure in the planning of a treatment.4 Therefore, it is necessary to conduct a precise assessment of its anatomy and location to prevent any damage.
Several surgical procedures, such as the placement of implants, mandibular ramus or body block grafts, embedded third-molar exodontia, ramus sagittal osteotomy, nerve transposition and the placement of miniscrews for orthodontics, pose a risk of damage to the IDN.14–17
Currently, the planning of these surgical procedures greatly benefits from the use of CT scans, which have been applied to the anatomical study of these areas.18
However, given the importance of preserving noble structures and the aggressiveness of some of these techniques, it is essential to understand the correlation between radiological measurements and actual measurements, so as to avoid planning errors.
In relation to the vestibular wall of the IDC, its radiological thickness ranged from 4.75–5mm from the mental foramen to 7–25mm from said point. When measured directly from the corpse, said thickness ranged from 4 to 6mm under the same conditions. The mean difference between radiological measurements and anatomical measurements amounted to 1.15mm. This difference must be taken into account upon planning surgical interventions on this area when performing a CBCT.
Our results from the radiological measurements were slightly higher than those obtained in the study conducted by Massey et al.,19 although it is rare that, in that study, radiographic measurements were lower than anatomical measurements in the rear areas but higher than the latter in the areas surrounding the mental foramen. It would seem that the magnification of the CBCT varies from one area to the other until it disappears and turns into a negative value. This effect was not observed in our study, where radiological measurements were higher than anatomical ones in all cases, regardless of their statistical significance in some situations.
In the work conducted by Kamburoglu et al.,12 which was focused on this same area, it was observed that anatomical measurements were somewhat higher than radiological ones, but almost practically the same.
The study conducted by Leong et al.4 was focused on the thickness of the buccal cortical bone. The data collected showed that the thickness of this structure ranged from 2.53 to 2.81mm in the buccal area. Based on these data and on the mean thickness of the vestibular mandibular cortical bone measured in our study (6.20mm when radiographically measured/5.05mm when anatomically measured), there would be a space of 2–2.5mm of trabecular bone over the IDC on a buccal level.
The mean thickness of our measurements was similar to that obtained in other studies, such as the one performed by Levine et al. in 2007 and by Yashar et al. in 2002 (4.9mm).20–22
The results related to the thickness of the IDC demonstrated that, in all locations, the radiologically measured thickness was greater than the anatomically measured one (mean value of 0.3mm).
Several articles indicate that the thickness of the vestibular table is reduced if the analysed individuals are Caucasian or older in the area of the furca of the first molar.20–22
In our study, we did not find differences in relation to the thickness of the vestibular table based on gender or location. However, the thickness of the IDC is lower for female subjects (for both anatomical and radiological measurements) than for male subjects.
In conclusion, the results obtained in our study indicate that the CBCT still presents differences when compared to actual measurements, despite being the best diagnostic method currently available. This difference amounts to a mean value of 1.15mm in relation to the thickness of the surrounding vestibular bone table and a mean value of 0.3m in relation to the thickness of the IDC.
It is essential to understand and assess these differences, given the wide range of surgical procedures that may be performed in this area and its closeness to the IDN.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Azcárate-Velázquez F, Bertos-Quilez J, Marmesat-Guerrero F, Núnez-Arcos P, Hernández-Alfaro F, Ferrés-Padrós E, et al. Fiabilidad del uso de la tomografía computarizada de haz cónico en la localización y medida del conducto mandibular en la planificación de técnicas quirúrgicas en el cuerpo mandibular. Rev Esp Cir Oral Maxilofac. 2015;37:182–187.