To compare the analgesic efficacy of continuous interpectoral block (CIPB) compared to intravenous analgesia (IV) after breast surgery.
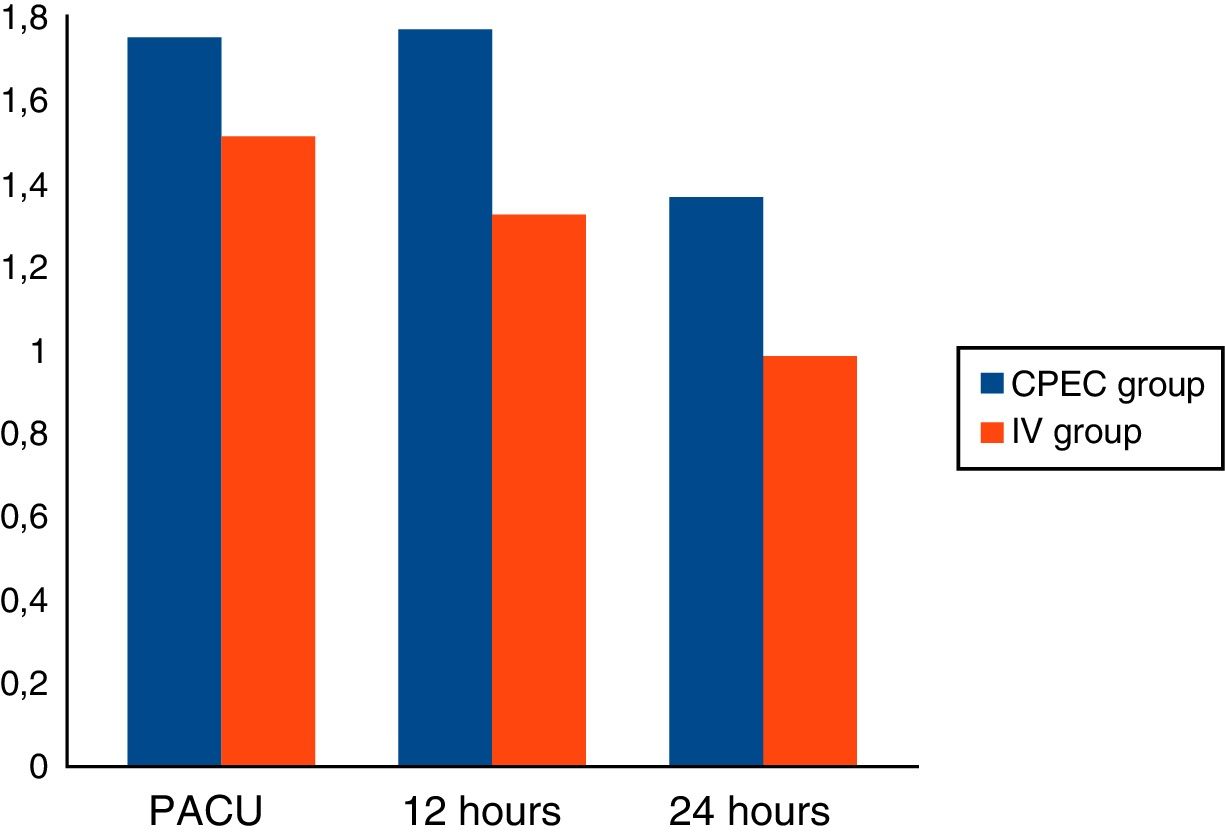
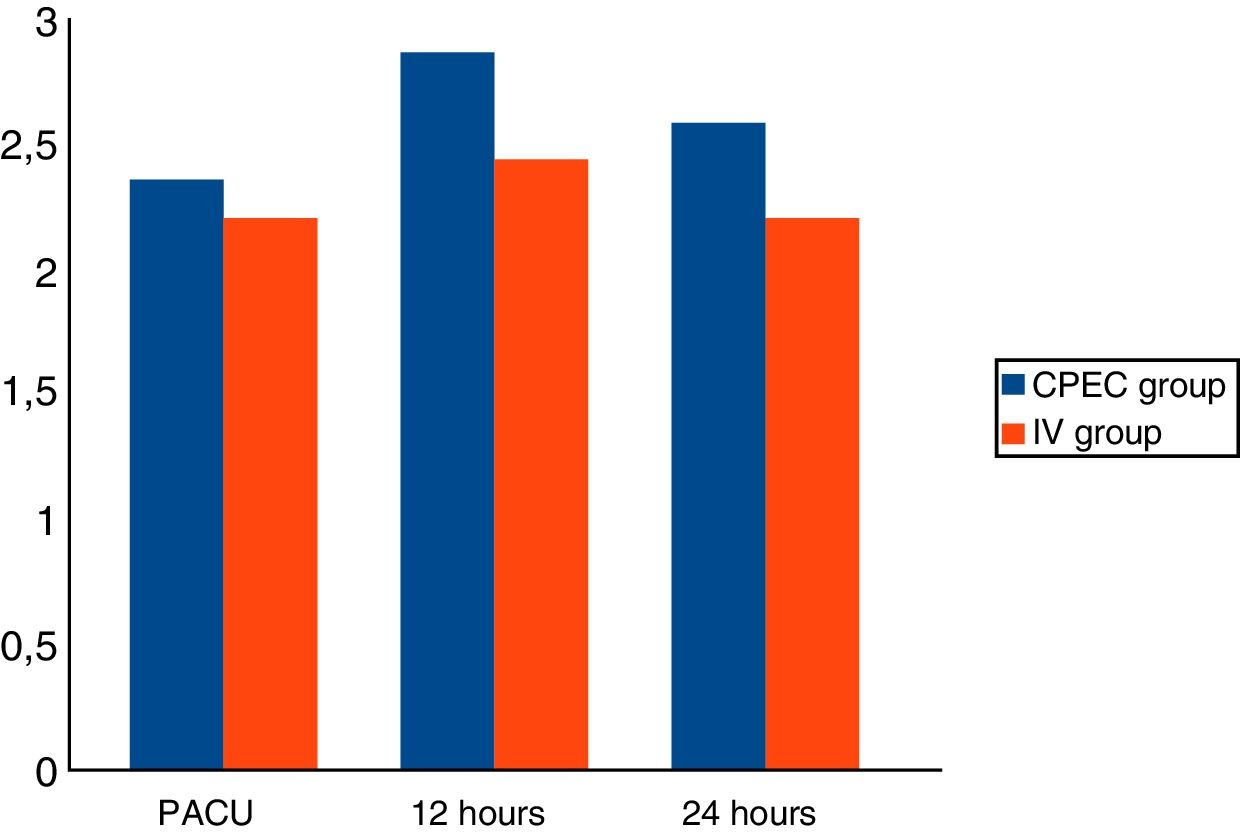
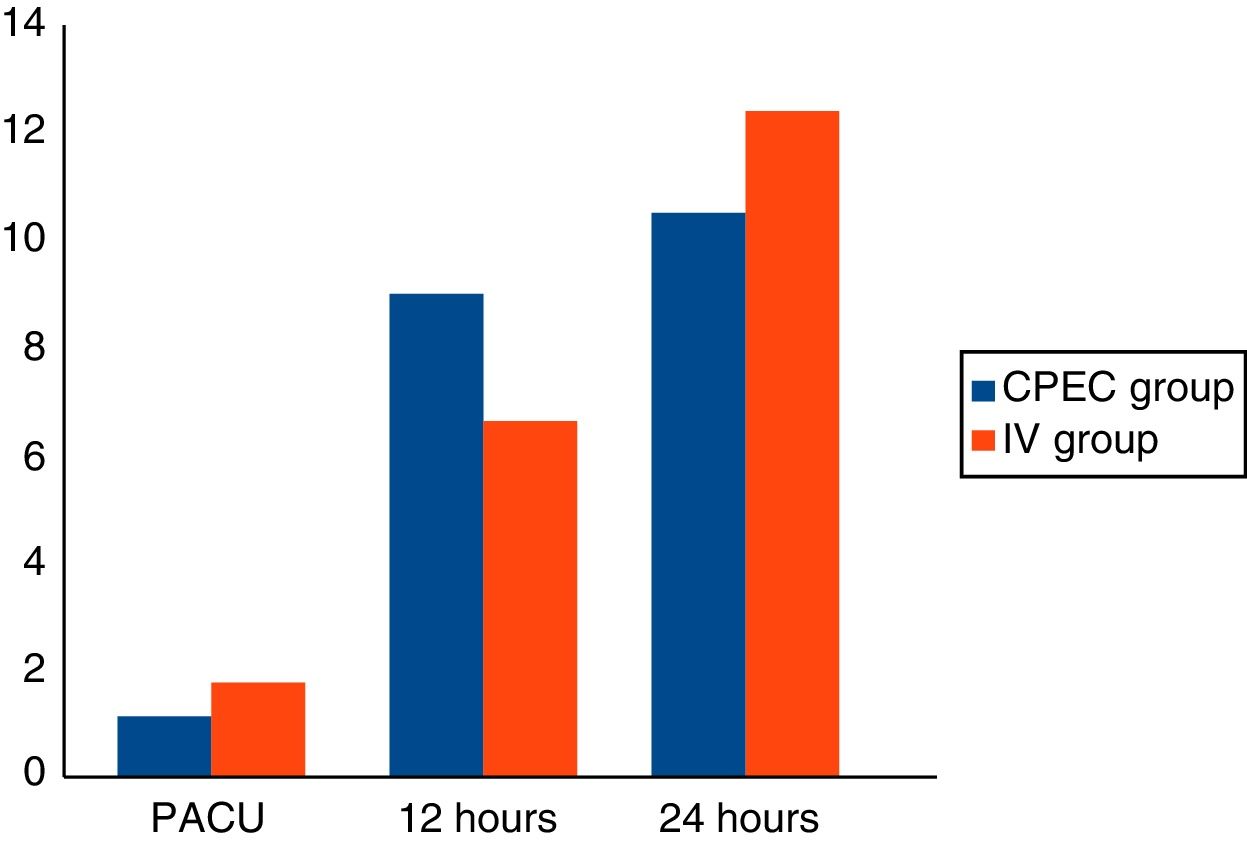
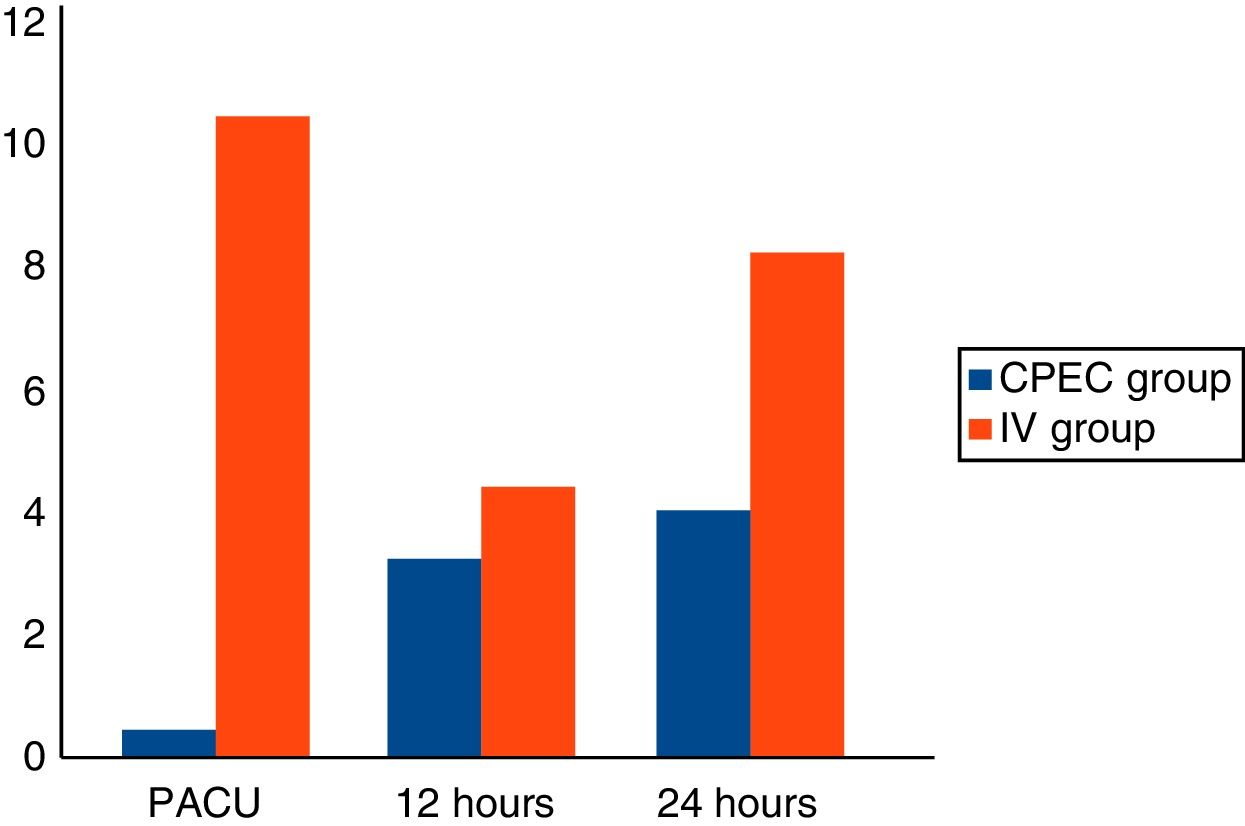
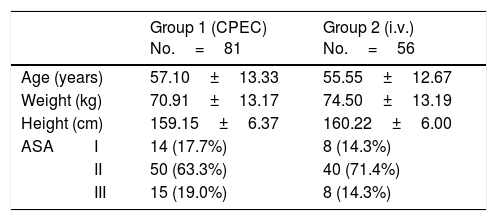
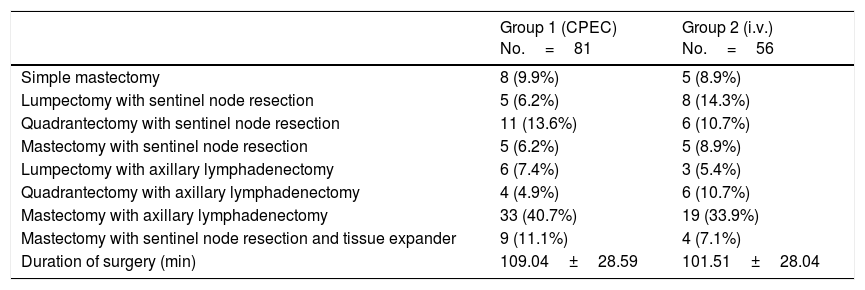
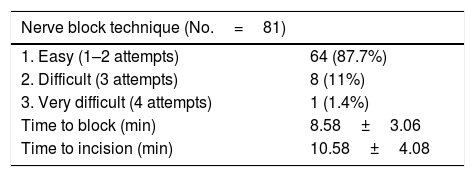
Material and methodA prospective, comparative and randomised study of women aged from 18 to 75years, ASAI-III, operated for breast cancer. In group1 (CIPB) after general anaesthetic, an ultrasound-guided interpectoral catheter was placed and 30ml of 0.5% ropivacaine was administered through it. In the event of an increase in heart rate and blood pressure >15% after the surgical incision, intravenous fentanyl 1μgkg−1 was administered, repeating the dose as necessary. In the postoperative period, perfusion of ropivacaine 0.2% 5mlh−1; with PCA bolus 5ml/30min was administered through the catheter for 24h and rescue analgesia prescribed with 5mg subcutaneous morphine chloride. In group2 (IV), after induction of general anaesthesia, intravenous fentanyl was administered in the same way as in the other group. The patients received metamizole 2g with dexketoprofen 50mg and ondansetron 4mg postoperatively followed by perfusion of metamizole 4%, tramadol 0.2% and ondansetron 0.08% 2mlh−1; with PCA bolus 2ml/20min for 24h. The same rescue analgesia was prescribed. The principal variables recorded were pain at rest and during movement, according to a simple verbal scale (VAS 0–10) and the rescue analgesia required on discharge from recovery, at 12 and at 24h.
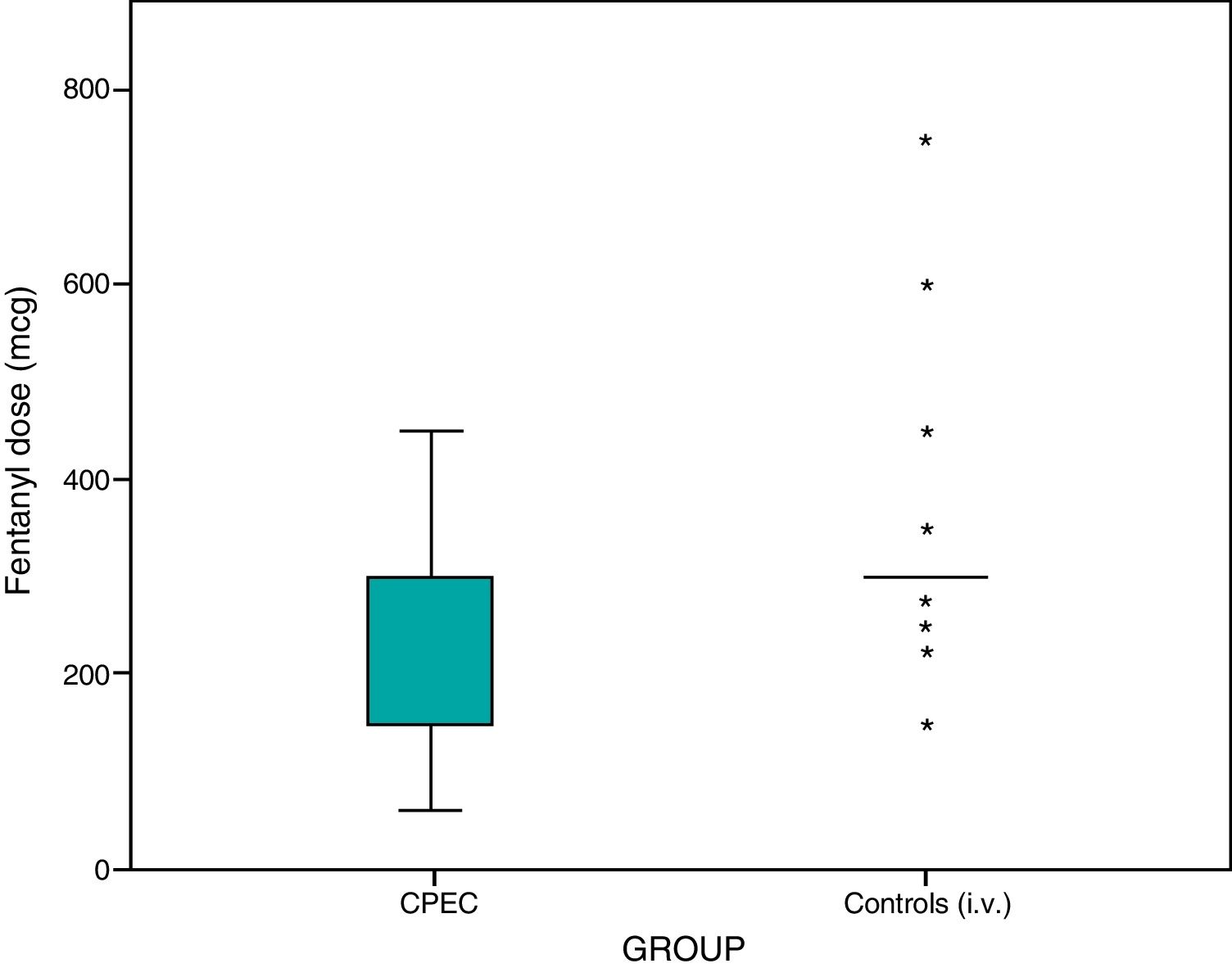
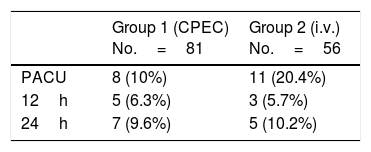
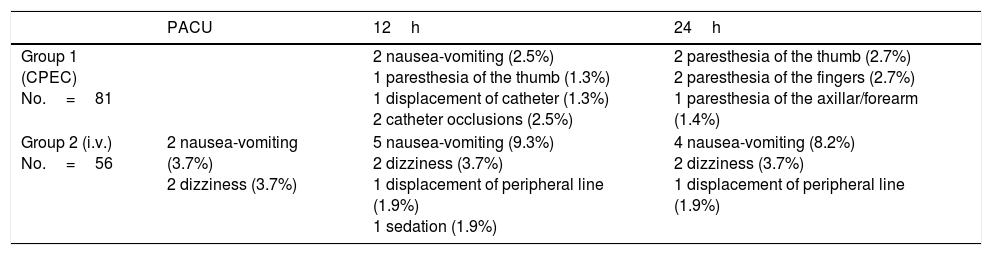
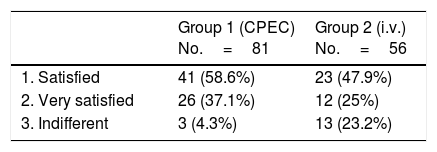
Results137 patients were included: 81 in group1 (59.12%) and 56 in group2 (40.87%). No significant differences were observed in the analgesia between either group, but differences were observed in the dose of intraoperative fentanyl (p<.05). Differences that were not significant were observed in the rescue analgesia required on recovery (10% fewer on group1).
ConclusionsBoth techniques provided effective postoperative analgesia, but the CIPB group required significantly less intraoperative fentanyl.
Comparar la eficacia analgésica del bloqueo interpectoral continuo (BIPC) frente a la analgesia intravenosa (i.v.) tras cirugía de mama.
Material y métodoEstudio prospectivo, comparativo y aleatorizado sobre mujeres de 18-75años, ASAI-III, intervenidas de cirugía oncológica de mama. En el grupo1 (BIPC), tras la inducción de anestesia general se colocó un catéter interpectoral ecoguiado y se administró ropivacaína 0,5% 30ml a su través. Tras la incisión quirúrgica, si la frecuencia cardiaca y la presión arterial se incrementaron >15% se administró fentanilo i.v., 1μg·kg−1, repitiendo la dosis en caso necesario. En el postoperatorio se inició perfusión de ropivacaína 0,2% 5ml·h−1; con bolo PCA 5ml/30min por el catéter durante 24h, y se prescribió analgesia de rescate con cloruro mórfico 5mg subcutáneo. En el grupo2 (i.v.), tras la inducción de anestesia general se administró fentanilo i.v. en caso necesario de la misma forma que en el otro grupo. En el postoperatorio se administró metamizol 2g con dexketoprofeno 50mg y ondansetrón 4mg seguido de perfusión de metamizol 4%, tramadol 0,2% y ondansetrón 0,08% 2ml·h−1; con bolo PCA 2ml/20min durante 24h. Se prescribió el mismo rescate analgésico. Las variables principales registradas fueron dolor en reposo y durante el movimiento, según una escala verbal simple (EVA 0-1), y la analgesia de rescate precisada al alta de reanimación, a las 12 y a las 24h.
ResultadosSe incluyeron 137 pacientes: 81 en el grupo1 (59,12%) y 56 en el grupo2 (40,87%). No se observaron diferencias significativas en analgesia entre grupos, pero sí en la dosis de fentanilo intraoperatorio (p<0,05). Se observaron diferencias no significativas en la analgesia de rescate requerida en reanimación (10% menor en el grupo1).
ConclusionesAmbas técnicas proporcionaron analgesia postoperatoria eficaz, pero el grupo BIPC precisó significativamente menos fentanilo intraoperatorio.