A major challenge during the COVID-19 outbreak is the sudden increase in ICU bed occupancy rate. In this article we reviewed the strategies of escalation and de-escalation put in place at a large university hospital in Madrid during the COVID-19 outbreak, in order to meet the growing demand of ICU beds.
Materials and methodsThe data displayed originated from the hospital information system and the hospital contingency plan.
ResultsThe COVID-19 outbreak produced a surge of ICU patients which saturated the available ICU capacity within a few days. A total of four new ICUs had to be opened in order to accommodate all necessary new ICU admissions. Management challenges included infrastructure, material allocation and ICU staffing. Through the strategies put in place the hospital was able to generate a surge capacity of ICU beds of 340%, meet all requirements and also maintain minimal surgical activity.
ConclusionsHospital surge capacity is to date hardly quantifiable and often has to face physical limitations (material, personnel, spaces). However an extremely flexible and adaptable management strategy can help to overcome some of these limitations and stretch the system capacities during times of extreme need.
Uno de los principales retos en el manejo de la COVID-19 es el aumento súbito de la demanda de camas de cuidados intensivos. En este artículo se describen las estrategias de gestión hospitalaria durante la escalada y desescalada de la respuesta a la epidemia de COVID-19 en un hospital terciario de Madrid.
Materiales y métodosLos datos derivan del sistema informático del hospital y del plan de contingencia del mismo.
ResultadosLa epidemia de COVID-19 produjo un rápido aumento de los pacientes con necesidad de cuidados intensivos, lo que saturó las camas de UVI disponibles en pocos días. El hospital tuvo que aumentar su capacidad abriendo cuatro UVI adicionales para proporcionar los cuidados necesarios a todos los pacientes. Los retos principales fueron relativos a la infraestructura hospitalaria, los materiales y el personal. Gracias a las estrategias de gestión utilizadas, el hospital fue capaz de aumentar su capacidad de camas de UVI en un 340%, proporcionar cuidados a todos los pacientes con necesidad y mantener una mínima actividad quirúrgica programada.
ConclusionesLa capacidad de un hospital de aumentar su capacidad para enfrentarse a eventos excepcionales es difícil de cuantificar y se enfrenta a limitaciones físicas (materiales, personal, espacios). Con una gestión flexible y adaptable durante eventos excepcionales se pueden alargar significativamente estos límites.
By early 2020, the pandemic caused by SARS-CoV-2 had spread to most countries in the world. In Spain, the disease spread with greater virulence in early March, and the autonomous community of Madrid has been the most severely affected region, with around 33% of deaths caused by COVID-19. One of the main challenges in managing COVID-19 was the sudden and exponential increase in demand for intensive care beds and mechanical ventilators,1,2 and the Madrid regional health system in particular was faced with the difficult task of increasing the capacity of its intensive care units (ICU).
In this article, we describe our experience in the Intensive Medicine and Anaesthesiology services of a tertiary teaching hospital, and the most crucial problems that had to be overcome during this extremely difficult period. We focus in particular on the escalation and de-escalation strategies within the framework of the institutional response to the pandemic. The Ramón y Cajal Hospital is the reference centre for the northern sector of the city of Madrid and the Madrid region, which has a population of around 600,000. It is a reference centre for stroke, cardiothoracic surgery and aortic pathology, and has one of the most active liver and kidney transplantation programmes. Its usual capacity is 901 hospital beds, 45 operating rooms and 38 intensive care beds (divided into 2 units: 1 run by the Anaesthesiology service and the other by the Intensive Medicine service). We retrieved data on patients admitted to intensive care units during the months of March and April 2020 and on surgeries performed (scheduled and emergency) during the same period from the hospital's computer database. We evaluated the increase in patients requiring admission to intensive care units by comparing the availability of ICU beds in the hospital's contingency plan.
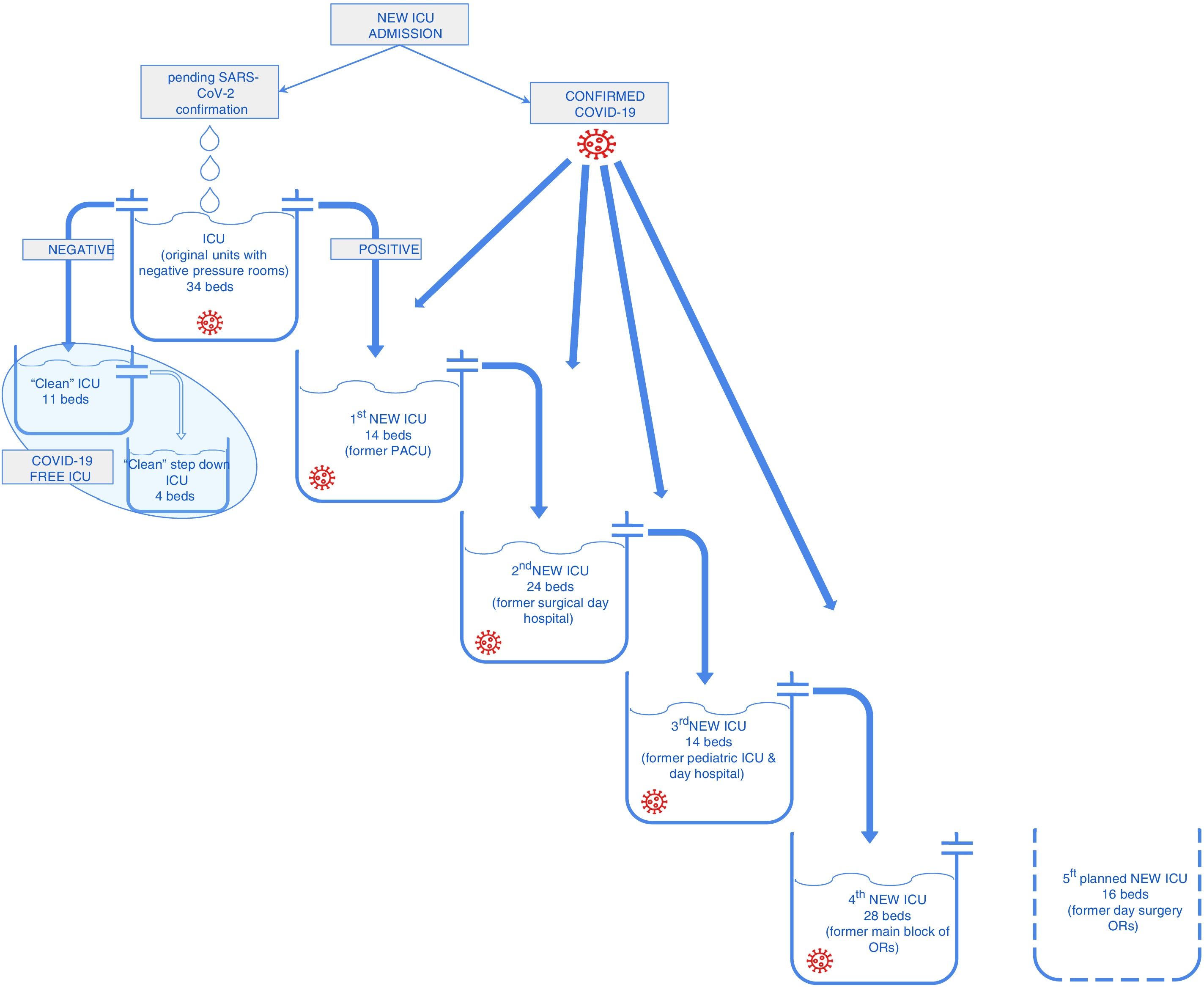
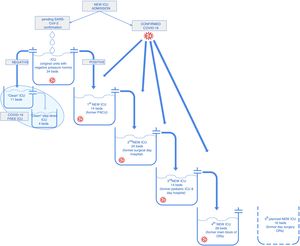
Reorganization of the hospital and the availability of critical beds: escalationAt the beginning of the outbreak in Madrid, the hospital’s management board created a working group to manage and reorganise the resources. One of the key aspects of this strategy was the capacity to adapt decisions and protocols (updated every day) to the rapidly changing situation imposed by the pandemic. The working group was responsible for implementing the contingency plan (opening new ICUs and distributing personnel) and validating institutional protocols for the management and treatment of the disease. Scheduled surgeries were minimised, mainly by suspending all outpatient surgery programmes and scheduled non-cancer surgeries. Exclusive circuits for COVID-19 patients were established to eliminate the potential intra-hospital spread of the disease. In the case of patients requiring critical care, all available ICU beds were regrouped and reorganized by merging the Anaesthesiology and Intensive Medicine services. Triage was carried out according to the guidelines of the Spanish Society of Intensive Medicine.3 Under a new institutional protocol, all patients with risk factors for clinical deterioration that were candidates for intensive care were flagged in the hospital’s computer system. This allowed the hospital emergency team to monitor potentially critical patients and promptly identify cases that required therapeutic escalation and admission to the ICU. Initially, the Surgical Critical Care unit, which has a negative pressure room, was reassigned to COVID-19 patients and received new admissions pending confirmation. Following this, a second unit for confirmed COVID-19 critical patients was opened and the former PACU was turned into a new critical care unit for PCR-negative patients. This meant that patients from the Emergency Department and from the wards were sent directly to a single unit where they could receive initial treatment without the risk of viral transmission. All critical patients from the Emergency Department or the ward were treated as suspected cases and were admitted to a negative pressure room in this “containment unit” until diagnosis was confirmed by PCR (between 4 and 6 h). Once diagnosis had been confirmed or ruled out, patients were transferred to the "unclean" ICU (COVID-19) or to the clean ICU, as appropriate.
This patient management strategy is the most widely described in the literature on epidemic outbreaks4 and was the most logical choice at the beginning of the outbreak, before the hospital became overwhelmed with new cases. In fact, this strategy only worked for a relatively short time, given the increasing number of patients requiring admission to the ICU, and new units were eventually opened to meet the demand for ICU beds. In 1 week (from 17 to 24 March 2020), 4 new units were opened to ensure that patients requiring critical care could be safely admitted to the ICU (Fig. 1). At this time, many patients were sent to the ICU from the wards with a confirmed diagnosis of COVID-19, and the number of admissions from the Emergency Room deceased accordingly. Patients with a diagnosis were admitted directly to COVID-19 units.
The challenge of increasing ICU capacityThe main problem to be overcome before opening new units in such a short period of time was the availability of infrastructure, personnel and material.
InfrastructureThe main obstacle to converting potentially suitable areas into intensive care units was the availability of gas outlet, aspiration systems and power supplies.5 The hospital's oxygen supply system had to be increased at an early stage of the pandemic in order to avoid the type of system shortages that occurred in Italian hospitals due to increased demand from a greater number of COVID patients.6,7 The areas to be turned into critical units were selected on the basis of the space available and the possibility of isolating or separating patients with the least possible alterations. Six areas of the hospital were selected for possible “new ICUs”: a 14-bed PACU, a 24-bed surgical day hospital area, a 14-bed PACU and paediatric day hospital, the hospital’s main 28-bed surgical suite (2 beds per operating room), a coronary unit with 15 beds, and a second surgical day hospital area with 16 beds. The possibility of increasing the number of ICU beds to 145 was studied, but this, fortunately, exceeded the real number required during the peak of the COVID-19 outbreak.
StaffApproximately 50% of specialists in the Anaesthesiology service had experience in critical care, and the curriculum of all anaesthesiology residents includes critical care training. This allowed us to created teams of physicians with more and less experience and thus guarantee uninterrupted care and guidance in anaesthesia procedures, and to assign clinicians with the greatest operating room experience to the management of critical patients. Residents nearing the end of their training who had greater experience in critical care also provided extremely valuable assistance in this regard. No new doctors had to be recruited to the Anaesthesiology service during the crisis. The Intensive Medicine service had to intensify its workload and reinforce its staff with 2 new members. This allowed the service to distribute its workload equally among its medical teams, achieving a doctor-patient ratio of 1:4–6 during the morning shifts and thus guaranteeing these complex patients the more detailed evaluation they require.
The nursing staff was a major challenge. A relatively small proportion of nurses receive critical care training, and this made it harder to create teams with varying degrees of experience to provide continuous guidance to less experienced staff. First, the operating room nursing staff, who had some experience in ventilator management and surgery, were reassigned to the “new ICUs”, but as more units were opened, ward staff also had to be redeployed and new nurses recruited. Despite our best efforts, not all reassigned nursing personnel received proper training during the crisis due to the overwhelming speed of escalation of the pandemic.
MaterialThe availability of ventilators has already been described as a crucial factor in managing the increase in critically ill COVID-19 patients. The first strategy was to redistribute old ventilators kept in storage. Once this supply had been exhausted, anaesthesia machines were removed from all operating rooms that had not been converted to ICUs and had therefore been closed due to the temporary suspension of all scheduled surgical activity. The use of anaesthesia machines to ventilate critically ill patients has been approved by most national regulatory bodies during the COVID-19 pandemic as an emergency measure to overcome shortages.8 Their use has guaranteed a rapid supply of mechanical ventilators, and they have also been used to administer anaesthetic gas to sedate some patients. The main challenges we faced with these ventilators were fresh gas flow adjustment and machine calibration. Manufacturers recommend different percentages of fresh gas during long-term mechanical ventilation.8,9 Our institutional policy was to establish a fresh gas flow of at least 100%. This reduced the condensation formed in the nozzles and extended the respirator recalibration period to 72 h.8,9 A transfer ventilator was used while the anaesthesia ventilator was checked, but this was time consuming for the medical and nursing staff.
To overcome this, anaesthesia ventilators were used in patients in more acute phases of the disease, many of whom required controlled ventilation and muscle relaxation. This freed up long-term mechanical ventilators for the most complex cases and for weaning. ICUs that used anaesthesia machines were staffed solely by anaesthesiologist, as they were more familiar with these machines and their idiosyncrasies.
Personal protective equipment (PPE) has also been in short supply, and sometimes of poor quality. Minimising the number of staff in charge of each patient and procedure and protocolising the administration of therapies and nursing care were the most effective PPE-saving strategies. Protocolising the administration and scheduling of treatments (such as prone positioning) has also helped reduce PPE use.10
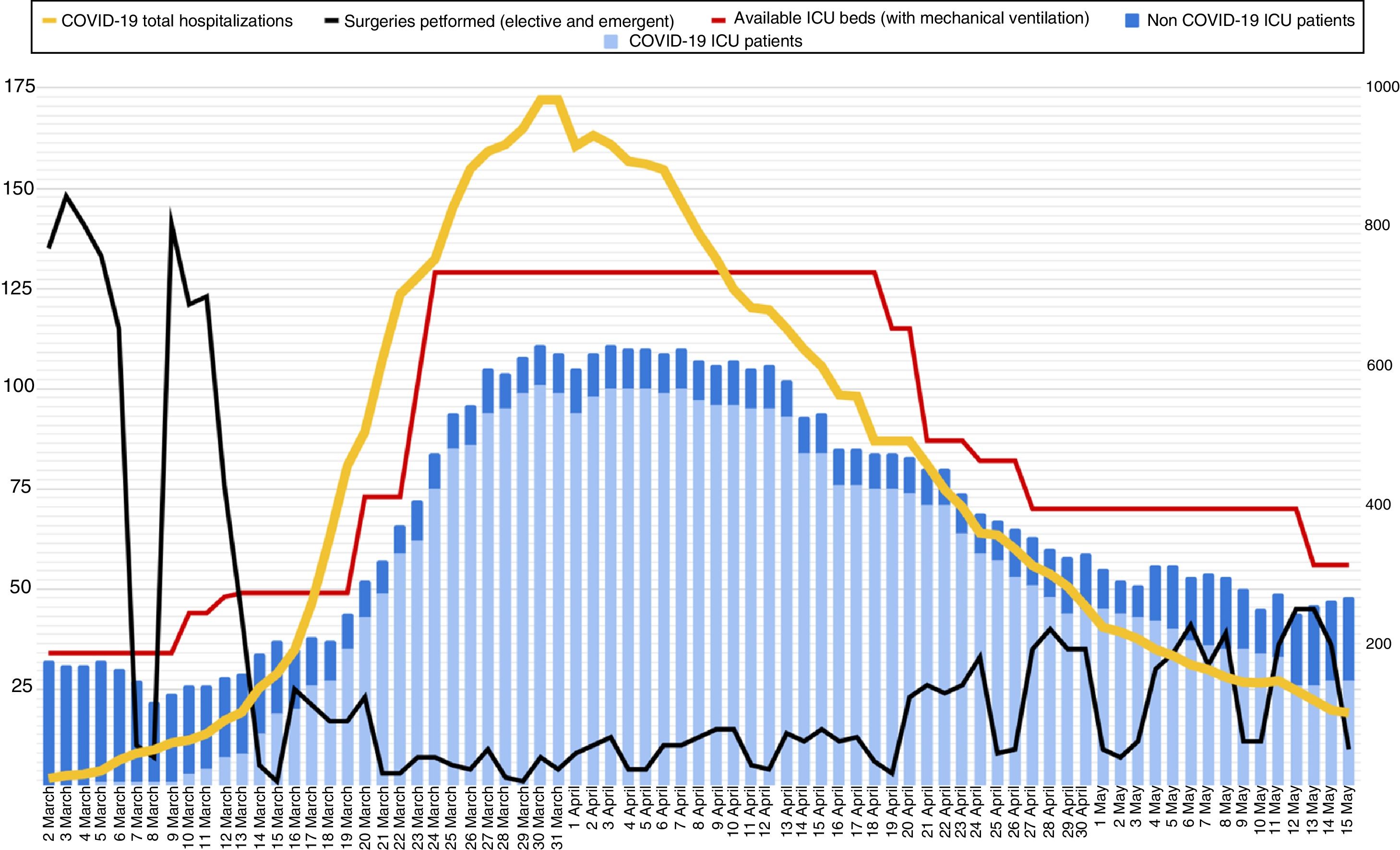
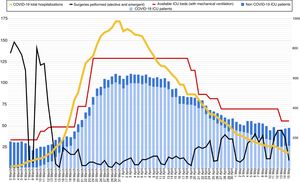
Reorganization of ICU bed capacity: de-escalation strategiesAt the peak of the epidemic (30 and 31 March 2020) 983 patients with a diagnosis of COVID-19 were admitted to the hospital, of these, 101 were admitted to an ICU and placed on invasive mechanical ventilation. There were another 10 patients without COVID-19 admitted to the ICU, bringing the total bed capacity to 129. The contingency plan ensured that the hospital would always have ICU beds available for all patients (Fig. 2).
Evolution of the number of ICU beds with availability of mechanical ventilation during the outbreak (red line) and number of patients admitted to the ICU, according to diagnosis (COVID-19 in light blue, non-COVID-19 in blue). The black line shows the number of surgical interventions (urgent and scheduled) performed in the hospital each day. The yellow line shows the total number of patients admitted with a diagnosis of COVID-19 (right axis).
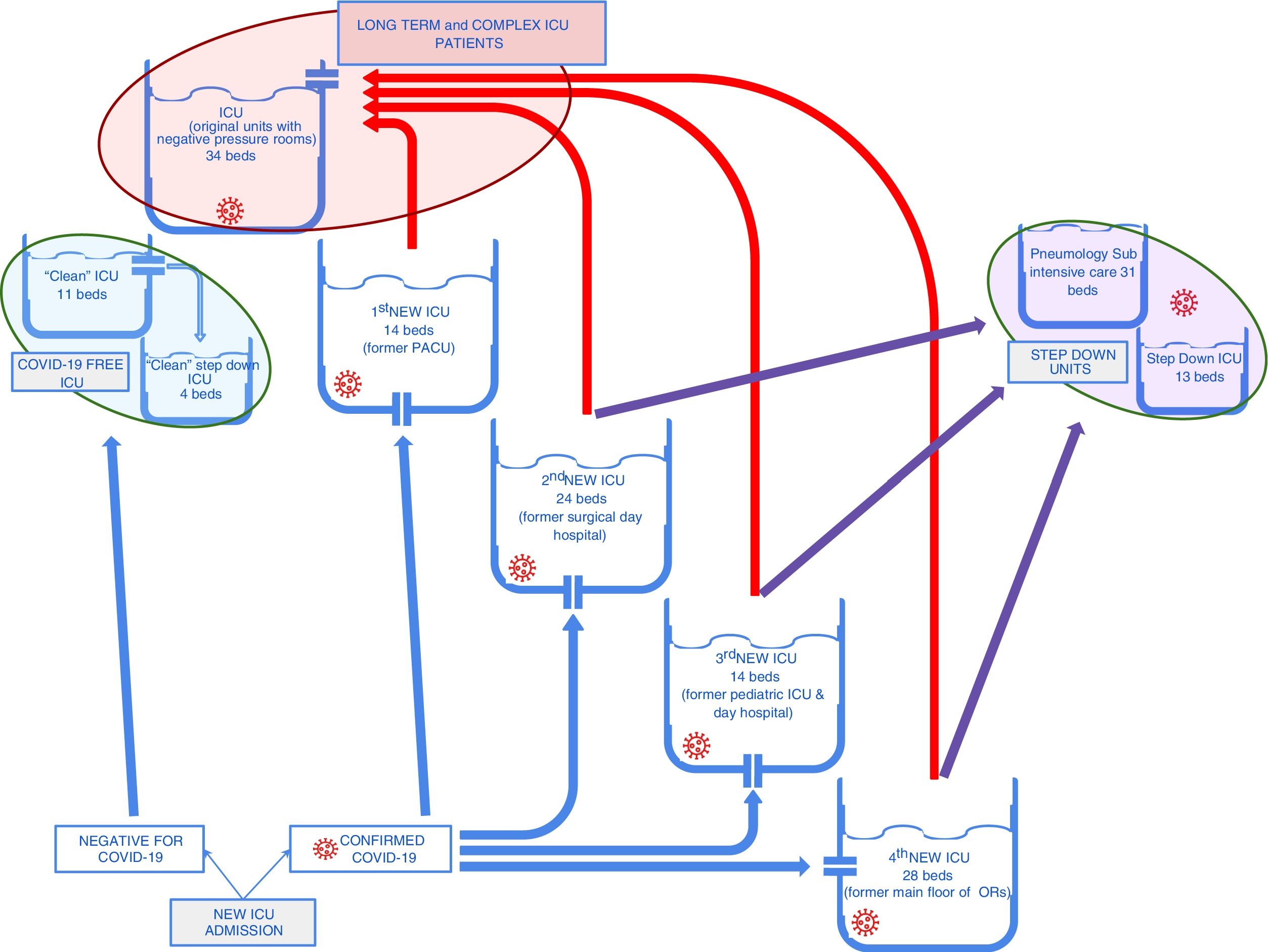
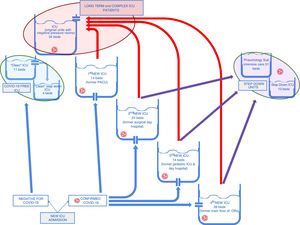
After 2 weeks of stabilization in the number of ICU admissions, hospitalization in critical units, hospital admissions, and bed occupancy, an active de-escalation strategy was initiated. Active de-escalation was implemented primarily by switching patients between COVID-19 ICUs and creating additional intermediate care units.
New ICU admissions were sent to the new units created in the surgical suites or in the PACU. More complex patients, with a longer evolution, or those with increasing need for support (renal replacement therapy, ECCO2R, ECMO) were transferred to the original ICUs as new beds became available. This meant that the "new" units received the bulk of the new admissions, performed triage and administered the initial treatment. Patients with a more favourable evolution that could be ventilated more easily and rapidly weaned remained in these units until they improved and could be transferred to intermediate units. The more complex patients were transferred to the original ICUs, which were better prepared for managing this population.
This strategy enabled us to close down 2 of the new ICUs relatively quickly, and group patients with more severe disease (Fig. 3). Closure of the "new" ICUs allowed us to reorganise staff. Some returned to their pre-epidemic activities (particularly the operating room staff, following the resumption of scheduled surgical activity) and the rest remained in the ICU to take part in training activities and collect data, and would be available in the event of a new escalation of COVID-19 cases.
Patient flow between the different ICUs during the active de-escalation phase. The red arrows show the flow of critically ill patients with a long ICU stay who were concentrated in the "original" ICUs. The purple arrows show the flow of patients with the fastest clinical improvement that could be transferred to intermediate care units.
The COVID-19 pandemic is an extraordinary challenge for healthcare systems, and tests to the limit their ability to provide critical care to large numbers of patients.
Specific challenges in this regard include infrastructure issues, such as the availability of scarce, complex resources such as mechanical ventilators, and particularly of personnel, specifically trained nurses.
We strongly believe that clear escalation and de-escalation strategies are vital to effectively cope with the increase in critical care patients. The strategies implemented in our hospital, which were rapidly adapted to meet changes in the arrival and departure of patients from and between the different units, allowed us to constantly adjust the system to the daily reality of the COVID-19 epidemic.
We also believe that despite multiple limiting factors, including human resources, infrastructure, and materials, ICU bed capacity can be significantly increased through skilful and, above all, flexible management.
The strategies described here allowed us to increase the availability of ICU beds by 340% from 38 to 129. This increased capacity allowed the hospital to provide intensive care to all patients in need without having to resort to interhospital transfers or to readjusting the ICU admission criteria. The active de-escalation strategy permitted an early resumption of scheduled surgical activity, and ensured the continuity of healthcare services after the peak of the epidemic.
Any hospital faced with a similar increase in the demand for ICU beds must establish a contingency plan with clear escalation and de-escalation strategies.
FundingThis article has not received any financial support.
Conflict of interestsThe authors declare that they have no conflict of interest.
Please cite this article as: Bardi T, Gómez-Rojo M, Candela-Toha AM, de Pablo R, Martinez R, Pestaña D. Respuesta rápida a COVID-19, estrategias de escalada y desescalada para ajustar la capacidad suplementaria de camas de UVI a una epidemia de gran magnitud. Rev Esp Anestesiol Reanim. 2021;68:21–27.