Granulomatosis with polyangiitis is a small- and medium-sized vasculitis. It is characterized by formation of granulomas and necrotizing inflammation with a predilection for the respiratory tract and glomeruli. The case is presented of a 14-year-old female debuting with hypoacusis, skin lesions, sinusitis; episcleritis, anti-PR3 ANCA positivity and histological findings from the skin lesions with neutrophilic infiltration, necrosis and fibrin. Granulomatosis with polyangiitis can present otological and skin manifestations as initial signs, and it is important to take the differential diagnosis into consideration.
La granulomatosis con poliangeítis (GPA) es una vasculitis de pequeño y mediano calibre caracterizada por la formación de granulomas e inflamación necrosante con predilección de las vías respiratorias y los glomérulos. Se reporta el caso de una adolescente de 14 años que comienza con hipoacusia y lesiones cutáneas; sinusitis, epiescleritis, PR3-ANCA positivo y biopsia de piel con infiltrado neutrofílico y necrosis. La GPA puede presentar manifestaciones otológicas y dermatológicas como signo inicial, es importante tomarlo en consideración en el diagnóstico diferencial.
Granulomatosis with polyangiitis (GPA), formerly called Wegener's granulomatosis, is a vasculitis of small and medium caliber vessels, systemic, necrotizing and granulomatous, with low incidence in pediatric patients, with a female–male ratio of 3–4:1.1 It is believed that some trigger factor penetrates the airways causing a neutrophilic response that promotes the synthesis of anti-neutrophil cytoplasmic antibodies (ANCA), cellular activation and finally a vascular lesion.2,3
It affects the upper and lower respiratory tract, as well as the kidney, therefore, its clinical findings include: asthenia, anorexia, weight loss; compromise of the upper respiratory tract (96%) such as sinusitis, otitis, subglottic tracheal stenosis, even with destruction of the nasal septum, which results in a saddle nose; renal involvement such as glomerulonephritis (88%), and ocular (52%), cutaneous (32%) and musculoskeletal (32%) involvement.1,4
GPA, Churg-Strauss syndrome and microscopic polyangiitis are vasculitides that affect small vessels; because of their association with ANCA, they are called ANCA positive vasculitis and of them, GPA is the most frequent. Its diagnosis is based on the clinical manifestations, the biopsy of the affected organs and the presence of ANCA in the serum.5 The objective of this article is to review the clinical manifestations in this patient who did not have renal manifestation and to review the current diagnosis of GPA.
Clinical observationA 14-year-old adolescent girl who is admitted because of having purulent rhinorrhea and fever of one week of evolution, hyperchromic dermal lesions on an erythematous base and two ulcers with thick scabs of 2 years of evolution. As an antecedent she presented hypoacusis that had begun at 7 years of age, assessed in another institution. On physical examination, stood out the cutaneous lesions located in the lower limbs, bilateral, symmetrical, that affected the dorsum of the feet, ankles and distal third of the legs, which began with papules, pustules and evolved to necrosis, it was observed the presence of two ulcers of 2cm in diameter covered by a deep serohematic crust, leaving hypo and hyperpigmented and atrophic scar lesions, which occur with periods of remission and exacerbation; and the presence of bilateral anterior episcleritis (Fig. 1).
Among the complementary tests: the complete blood count, CRP, erythrocyte sedimentation rate, urea, creatinine, complement and urine test were normal. The serology for HIV was negative. The peripheral blood smear did not reported blasts. The IgG was elevated, 2446IU/ml (reference value: 1264±280). The CT scan of the paranasal sinuses revealed opacity of maxillary sinuses and mucosal thickening of the maxillary and ethmoid sinuses and turbinates (Fig. 2). The chest CT scan showed no pulmonary nodules.
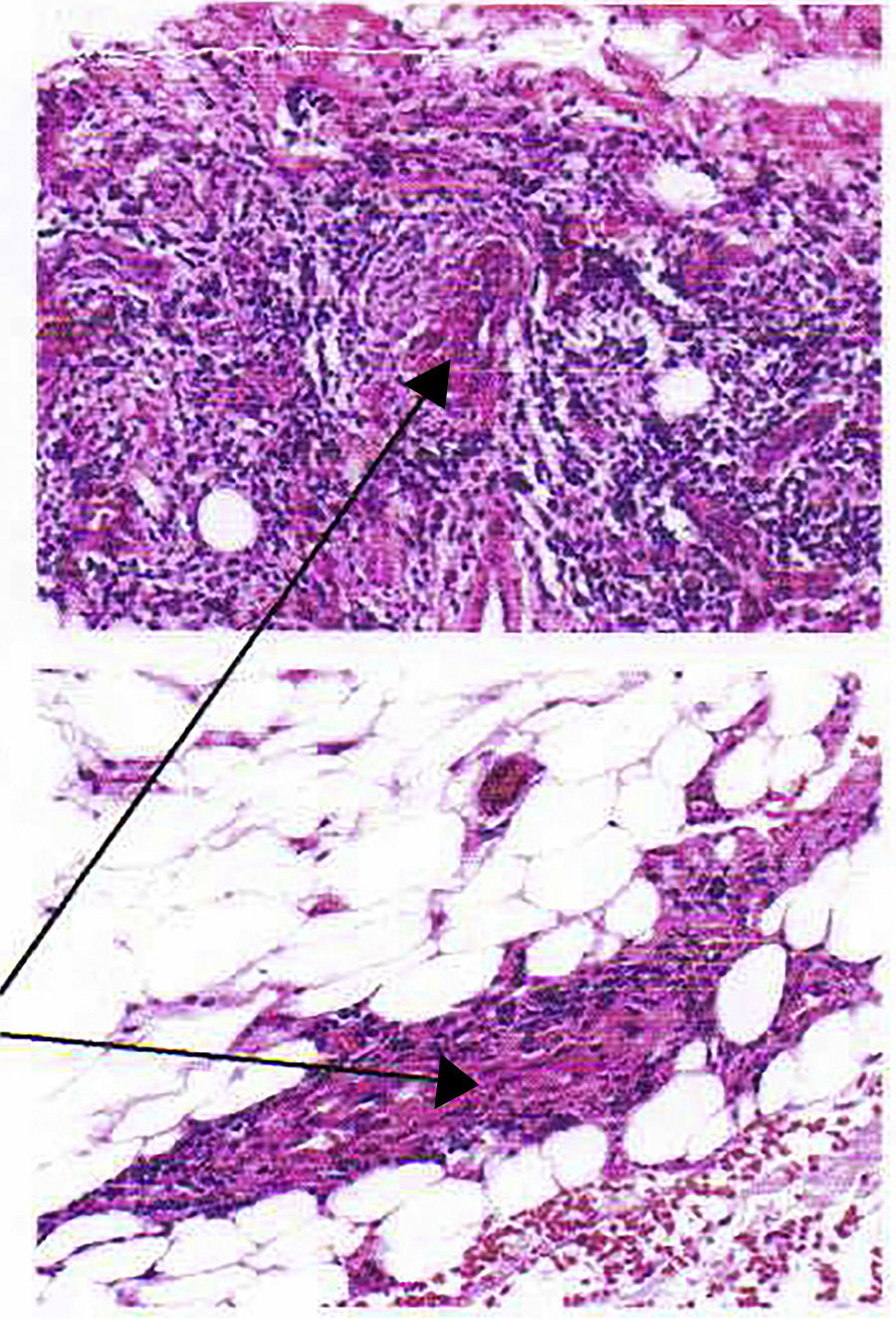
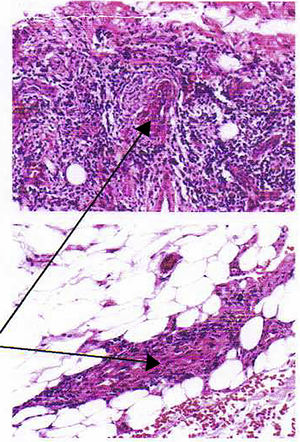
The skin biopsy shows a dermis with perivascular and interstitial lymphocyte, plasmacytic and histiocytic infiltrate; lymphocytic and neutrophilic infiltrate in the wall of superficial, deep and hypodermic vessels of small caliber, with necrosis and fibrin deposition, erythrocyte extravasation and hemosiderin deposition; concluding that it is a vasculitis of small cutaneous and subcutaneous vessels. (Fig. 3) PR3-ANCA was requested, which was positive, 9.5U/ml (reference value: 0–5).
The patient was assessed by otorhinolaryngology; in the otomicroscopy of both ears they found the external auditory canal free and the tympanic membrane was intact. The audiometry reported severe bilateral mixed hearing loss, air threshold in the right ear in 68db (GAP of 10), air threshold in the left ear 77db (GAP of 20).
The patient completed 2 classification criteria (Table 1) for GPA with a suggestive disease and other compatible clinical manifestations; therefore, it was started treatment with corticosteroid pulses (30mg/kg/day) for 3 days, then prednisone at 1mg/kg/day and methotrexate 20mg/m2 weekly subcutaneously. The Birmingham Vasculitis Activity Score before treatment was 13, and at 45 days of treatment it was 2. The lesions improved, she had no longer ulcers, while the hypoacusis persisted (Fig. 4).
Diagnostic criteria for granulomatosis with polyangiitis.
| Three of the following characteristics must be present: |
| Abnormal urine test |
| Biopsy with granulomatous inflammation |
| Inflammation of the paranasal sinuses |
| Subglottic, tracheal or endobronchial stenosis |
| Abnormal chest X-ray or tomography |
| Positive PR3-ANCA or c-ANCA |
Significant hematuria or proteinuria.
If the kidney biopsy is performed, it typically shows a pauci-immune necrotizing glomerulonephritis.
Source: Ozen et al.6
GPA, according to the new CHCC 2012 (Chapell Hill Consensus 2012) nomenclature, formerly called Wegener's granulomatosis, typically presents necrotizing granulomatous inflammation that affects the upper and lower respiratory airways, and necrotizing glomerulonephritis. In addition, ocular vasculitis and pulmonary capillaritis are frequent. Granulomatous and nongranulomatous extravascular inflammation is also common.2,3,6
GPA is very rare in children, the incidence is estimated at 0.1 per 100,000 inhabitants, while in adults is one per 100,000 inhabitants.4 Initially, the nonspecific symptoms or the localized forms can make diagnosis a real challenge. The diagnostic delay in the patient was of 7 years from the first symptom (hypoacusis). The otological manifestations, such as otitis media, tinnitus, and vertigo are described in 20–60% of patients, and hypoacusis in 16%. Conductive hearing loss, although described in children, is much less frequent than in adults (29% in adults, 11% in children). Early treatment improves the prognosis of hearing.4,7–9 The episcleritis and sinusitis that appeared late in the patient are present in 44% of patients with GPA,8 and according to Pakrou et al., ocular involvement in GPA is common; in their review they report an incidence greater than 50–60% (up to 87%) in any period of the disease.10
ANCAs are a diagnostic criterion and they help in the follow-up. Of the 2 related autoantibodies: proteinase-3 (PR3-ANCA or c-ANCA) and myeloperoxidase (MPO-ANCA or p-ANCA), PR3-ANCA has a sensitivity and specificity of 90% for GPA.2,11
Histopathology confirms the diagnosis. Histological evidence of necrotizing granulomatous vasculitis, necrotizing granulomas without vasculitis, vasculitis of small and medium vessels or acute and chronic inflammation can be found depending on the biopsy site.3,12,13 At the level of the skin, the cutaneous biopsy reveals a leukocytoclastic vasculitis, that is, a small vessel vasculitis with a predominant neutrophil infiltrate, without deposits (or with scarce deposits) of complement and immunoglobulins in immunofluorescence. Often, necrotizing inflammatory granulomas are also seen constituting the characteristic histological picture.13 Even though the patient did not present granulomas, she did have vasculitis with neutrophilic infiltrate in superficial and deep small vessels with necrosis; that, added to the positive PR3-ANCA, the sinusitis and the other clinical data makes us think of GPA as a diagnosis.
ConclusionsPerforming a histopathology in lesions suspicious for vasculitis may clarify the diagnosis.
GPA must not necessarily have renal involvement; there are localized forms that only compromise the respiratory tract and the skin.
GPA should be part of the differential diagnosis of sensorineural or conductive hypoacusis. Even more considering that timely therapy improves the prognosis of hearing.
Conflict of interestThe authors declare that they do not have any conflict of interest.
Please cite this article as: Herrera CN, Barreno V ME, Quintana Vega VJ, Suquilanda Feria DB. Hipoacusia y vasculitis cutánea, manifestación inicial de granulomatosis con poliangeítis en una niña de 14 años. Rev Colomb Reumatol. 2019;26:216–219.