The new coronavirus disease 2019 (COVID-19) outbreak has rapidly spread throughout the world, becoming a serious public health problem. COVID-19, in addition to respiratory symptoms, has neurotropic characteristics that can impact the nervous system. We present a 22-year-old female who developed diplopia and numbness of her limbs eight days after affecting by COVID-19 and she showed a left-sided outward gaze palsy without any history of previous a specific illness or medication. Supratentorial, infratentorial, and cervical cord enhancing plaques confirmed an acute demyelinating process in favor of Acute disseminated encephalomyelitis (ADEM). Her oligoclonal bands (OCB) were positive as well. As a result, a provisional diagnosis of ADEM was made. Her condition improved dramatically after starting corticosteroids and rituximab.
El nuevo brote de coronavirus de 2019 (COVID-19) se ha propagado rápidamente a nivel mundial, convirtiéndose en un serio problema de salud pública. La COVID-19, además de síntomas respiratorios, tiene características neurotrópicas que pueden repercutir en el sistema nervioso. Presentamos el caso de una mujer de 22 años que desarrolló diplopía y entumecimiento de las extremidades inferiores 8 días después de verse afectada por la COVID-19, mostrando parálisis de la mirada excéntrica en el lado izquierdo sin antecedentes de enfermedades o medicaciones específicas previas. La intensidad de las placas supratentoriales, infratentoriales y de la columna cervical confirmó un proceso desmielinizante agudo que favorecía encefalomielitis diseminada aguda (ADEM). Asimismo, sus bandas oligoclonales fueron positivas. En consecuencia, se diagnosticó provisionalmente ADEM. Su situación mejoró considerablemente tras iniciar tratamiento con corticosteroides y rituximab.
The present coronavirus disease 19 (COVID-19) pandemic is still affecting people all over the world. The COVID-19 situation in Iran (the Islamic Republic) is as follows according to the information reported to WHO until 14 May 2022, A total of 7,227,043 cases and a cumulative total of 141,201 deaths.1 This novel coronavirus often manifests with fever, cough, myalgia, and signs and symptoms of the respiratory system.2–4 Severe acute respiratory coronavirus 2 (SARS-CoV-2), is a neurotropic virus leading to complications in both the central and peripheral nervous systems.5 In this regard, headache, ataxia, seizures, polyneuropathies, cerebrovascular disorders, and demyelinating illnesses are among the consequences that might occur after a viral infection, with an incidence of 36 percent.6–8 Following a COVID-19 infection, demyelinating disorders such as acute disseminated encephalomyelitis (ADEM) have been reported in the literature.9 In the present study, we present a rare case of ADEM in a 22-year-old female following SARS-CoV-2 infection.
Case presentationA previously healthy 22-year-old female without any specific pathological history was referred to an outpatient clinic for post-COVID-19 follow-up on November 11th, 2021. She had referred to an outpatient clinic (October 9th, 2021) due to a COVID-19 infection with typical signs and symptoms, including fever, cough, and myalgia. Her COVID-19 infection had been confirmed by real-time polymerase chain reaction (RT-PCR) without pulmonary involvement on the first CT scan. Her symptoms gradually improved with isolation instructions without receiving medication. Throughout the day after the next eight days of her positive COVID-19 test, she was hospitalized with complaints of severe fatigue, diplopia, dizziness, and nausea, associated with numbness and intermittent tingling on the right side of her face and her fingers. She never had any of these symptoms before. She also denied having ever had a migraine or having any relatives with neurological disorders.
On examination, she was afebrile, with a blood pressure of 110/80mmHg, respiratory rate of 16 per minute, heart rate of 65 per minute, and oxygen saturation of 98%. Her fundoscopic exam findings were normal. As for visual acuity, there was not any deficit except diplopia which was due to internuclear ophthalmoplegia (INO) on the left side. Respiratory and cardiovascular examinations were non-significant.
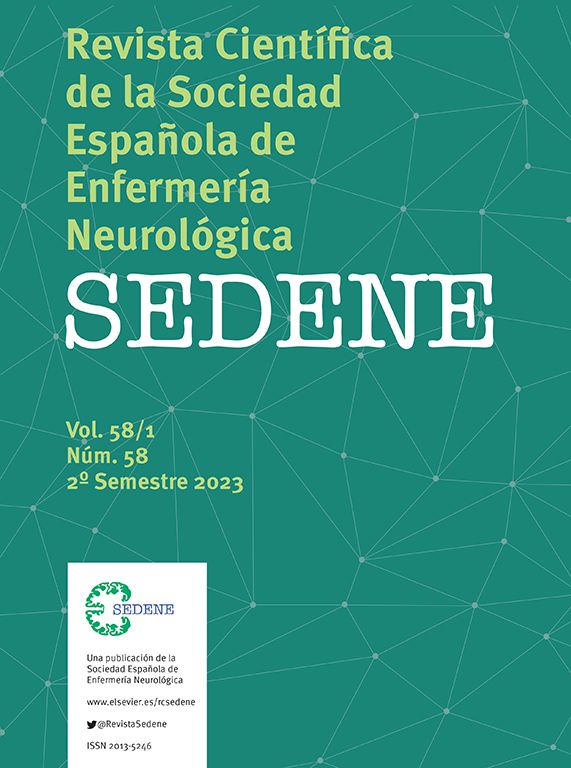
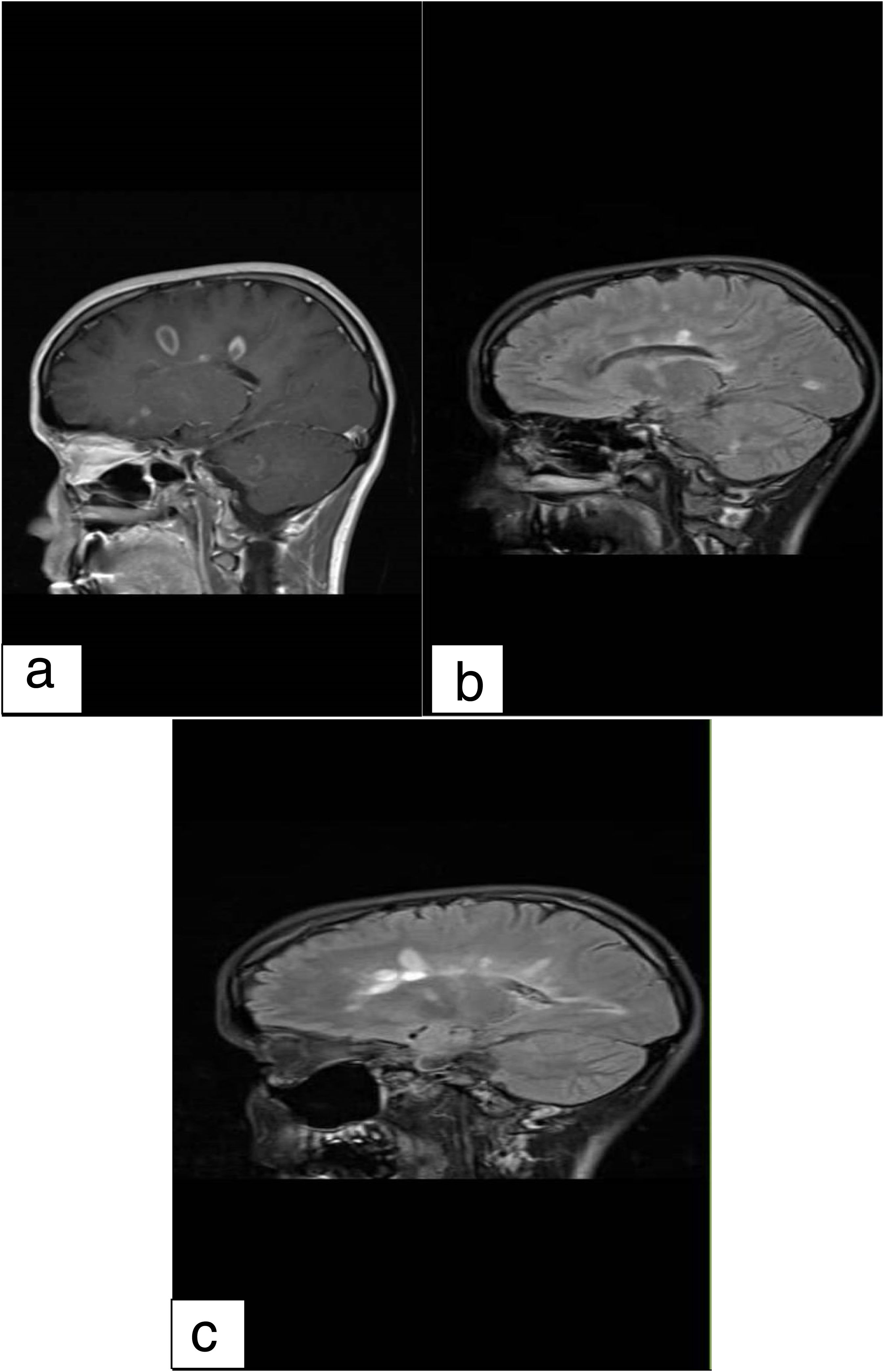
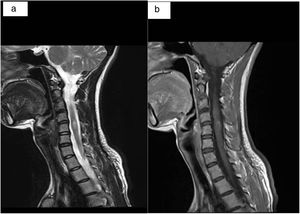
With respect to magnetic resonance imaging (MRI) of the brain and cervical spine, multiple bilateral periventricular lesions and subcortical white matter, hyper signal foci were seen in fluid-attenuated inversion recovery (FLAIR) sequence (Fig. 1a) with peripheral incomplete ring enhancement in post-contrast images (Fig. 1b). As it has been shown in Fig. 1c, the lesion showed perpendicular orientation to the callosal axis (Dawson's finger). Brain stem and cerebellar hemispheres showed similar lesions. C3-C4 and C7-T1 short segment peripheral enhancing lesions were seen in T1 with gadolinium and T2 (Fig. 2). Therefore, supratentorial, infratentorial, and cervical cord enhancing plaques confirmed an acute demyelinating process in favor of ADEM. These neuropathologic lesions are primary demyelinating process due to Para infection and no other findings in favor of other pathological processes were observed in imaging.
Autoimmune screening, including antinuclear antibody (ANA), antineutrophil cytoplasmic antibodies (ANCA), antiphospholipid antibodies, human leukocyte antigen (HLA) B5, and HLA-B51 was negative. Other serological tests such as venereal disease research laboratory (VDRL), erythrocyte sedimentation rate (ESR), and rheumatoid factor (RF) were unremarkable.
Viral screening tests, moreover, for human immunodeficiency virus (HIV), hepatitis B virus (HBV), and hepatitis C virus (HCV) were also negative. The PCR test of the patient's CSF sample was negative for detecting SARS-CoV-2. Furthermore, there were oligoclonal bands (OCB) in her spinal fluids, while no band was seen in her serum specimen.
Based on history, physical examination, and detailed investigations, a diagnosis of ADEM triggered by COVID-19 was made, as no other etiology was identified. She was admitted for 12 days, she didn’t require intubation during hospitalization, managed to receive 10g of corticosteroids (1g daily for 10 days), and then take 1g of rituximab. The next dose is to receive rituximab 6 months later. Her double vision was improved. The numbness of the limbs improved significantly, which took a short time to completely resolve.
DiscussionEven though SARS-CoV-2 is primarily a respiratory virus, it can also impact the cardiac, hematological, gastrointestinal, renal, hepatic, dermatological, and neurological systems. COVID-19's neurotropic properties and impacts on the nervous system as a primary organ have recently been suggested.10,11 In this regard, neurologic disorders in patients with COVID-19 are as follows: acute disseminated encephalomyelitis (ADEM), toxic encephalopathy, viral encephalitis, Guillain-Barre syndrome, peripheral nerve disease, MS, etc.11,12 Our case involved the cervical part of the spinal cord, which was similar to the case reported by Sarwar et al.13 On the other hand, olfactory bulb involvement was reported in Fragoso et al.,14 while our case did not have any such involvement. As a result, it could be hypothesized that central nervous system (CNS) involvement in ADEM following COVID-19 patients is not similar. Among different patients, indicating probable different pathogenesis of neurological involvements in patients with COVID-19 infection. Several studies have connected autoimmune diseases to a variety of viruses, including the parainfluenza virus and the coronavirus after 6–7 weeks of exposure.15 Previous investigations revealed various mechanisms of COVID-19 neurotropism to illustrate how COVID-19 works as a neuropathogenic. The virus may increase the permeability of the blood-brain barrier (BBB) via cytokines produced by macrophages, allowing it to permeate the brain, inducing glial cell activation and demyelination of nerve fibers.16 The SARS-CoV-2 might have triggered T-lymphocyte activation, which would have resulted in demyelination, activation of microglia, and the release of inflammatory mediators.17 The presence of angiotensin-converting enzyme 2 (ACE2) receptors in the nervous system, including glial cells, and basal ganglia and their affinity to SARS-CoV-2, moreover, the direct invasion of SARS-CoV-2 into the brain through the nasopharyngeal area, all of which culminate in the onset of neurologic symptoms.18,19 However, the data to support this idea is insufficient. The clinical manifestation of our case developed after the patient's recovery from COVID-19-related symptoms as well as she met the diagnostic criteria for ADEM, it is safe to presume that the disease's pathogenic process had already begun following the SARS-CoV-2 infection. As a result, COVID-19 may have acted as a triggering element in the development of ADEM in our case. The number of cases infected with COVID-19 triggering and aggravating autoimmune disorders is growing in the literature, and future research into the causal relationship between ADEM and COVID-19 infection is needed.
ConclusionThe temporal association between viral infection and the commencement of demyelinating events like in our case suggests that the mechanism is post-infectious rather than parainfectious. Our case indicates that SARS-CoV-2 may have a role in the development of ADEM, however, our research is confined to a single case. As a result, COVID-19, due to its neurotropism properties, may occur in the early stages of some neurological illnesses, such as ADEM, for which more evidence is needed to determine causality.