Hyperprolactinemia is a frequent condition in clinical practice, responsible for 20–25% of secondary amenorrhea cases. We performed an electronic survey among members of the Brazilian Society of Metabolism and Endocrinology (SBEM) and the Brazilian Federation of Association of Gynecology and Obstetrics (FEBRASGO) to assess diagnostic and therapeutic preferences for management of hyperprolactinemia. Electronic addresses of SBEM and FEBRASGO members were obtained from the directories of these societies, and these members were invited, through electronic messages (e-mail), to answer an online questionnaire that included 10 questions about the treatment of micro and macroprolactinomas, maximum dose of dopamine agonist, how to exclude primary hypothyroidism and macroprolactinemia, hyperprolactinemia and pregnancy. We received responses to the questionnaire by e-mail from 521 SBEM members and 233 FEBRASGO members. The results of this survey demonstrate that there are many area of agreement between SBEM and FEBRASGO members and most of their responses follow the latest Endocrine Society Guideline. Relative to a survey performed several years ago, our findings show that SBEM members have incorporated some of latest recommendations in this field. The principal issues of concern for both groups are duration of dopamine agonist treatment for patients with microprolactinoma and dopamine agonist withdrawal during pregnancy.
La hiperprolactinemia es una alteración frecuente, siendo responsable del 20 al 25% de los casos de amenorrea secundaria. Se realizó una investigación electrónica entre los miembros de la Sociedad Brasileña de Endocrinología y Metabología (SBEM) y de la Federación Brasileña de Ginecología y Obstetricia (FEBRASGO) para evaluar sus preferencias en el diagnóstico y el tratamiento de la hiperprolactinemia. Las direcciones electrónicas de miembros SBEM y de FEBRASGO se obtuvieron a partir de los directorios de esas sociedades. Se invitó a estos miembros a responder un cuestionario que incluía 10 cuestiones sobre el tratamiento de los micro y macroprolactinomas, dosis máxima del agonista dopaminérgico, hiperprolactinemia e hipotiroidismo primario, macroprolactinemia, prolactinoma y embarazo. Hemos recibido respuestas de 521 miembros de la SBEM y de 233 miembros FEBRASGO. Los resultados demuestran que hay bastantes áreas de concordancia entre los miembros de la SBEM y de la FEBRASGO y que la mayoría de las respuestas están de acuerdo con el último consenso de la Endocrine Society. En cuanto a una encuesta similar realizada hace años, nuestros resultados muestran que los socios de SBEM incorporaron algunas de las últimas recomendaciones propuestas en esa área. Los principales aspectos de interés en ambos grupos son la duración del tratamiento con el agonista dopaminérgico y la retirada del mismo durante el embarazo.
Hyperprolactinemia is a frequent condition in clinical practice, responsible for 20–25% of secondary amenorrhea cases,1 and prolactinomas are an important cause of pathological hyperprolactinemia. They are classified according to their size: micro (<10mm in diameter) and macroprolactinomas (>10mm in diameter). Most are small, intrasellar, and rarely increase in size.2,3
The principal symptoms of hyperprolactinemia are amenorrhea in women, erectile dysfunction in men and infertility and reduced libido in both sexes. Patients with large prolactinomas may also present with hypopituitarism, headache and visual field loss.4
The primary treatment objective in patients with microprolactinoma or idiopathic hyperprolactinemia is to restore gonadal and sexual function by normalizing prolactin levels.2 However, in the presence of macroprolactinomas, reducing and controlling tumor size are also fundamental goals.2
Dopamine agonists (DAs) are the first treatment option for prolactinomas. All DAs are efficacious, but cabergoline and bromocriptine are most commonly used worldwide. These drugs are able to normalize prolactin levels, restore gonadal function and promote tumor reduction in the majority of patients.2
Despite existing guidelines regarding the management of hyperprolactinemia,2 controversies remain regarding when to screen for macroprolactinemia, what kind of patients should be treated, treatment duration, maximum dose of the DA and treatment approach during pregnancy.
We performed an electronic survey among members of the Brazilian Society of Metabolism and Endocrinology (SBEM) and the Brazilian Federation of Association of Gynecology and Obstetrics (FEBRASGO) to assess diagnostic and therapeutic preferences for management of hyperprolactinemia.
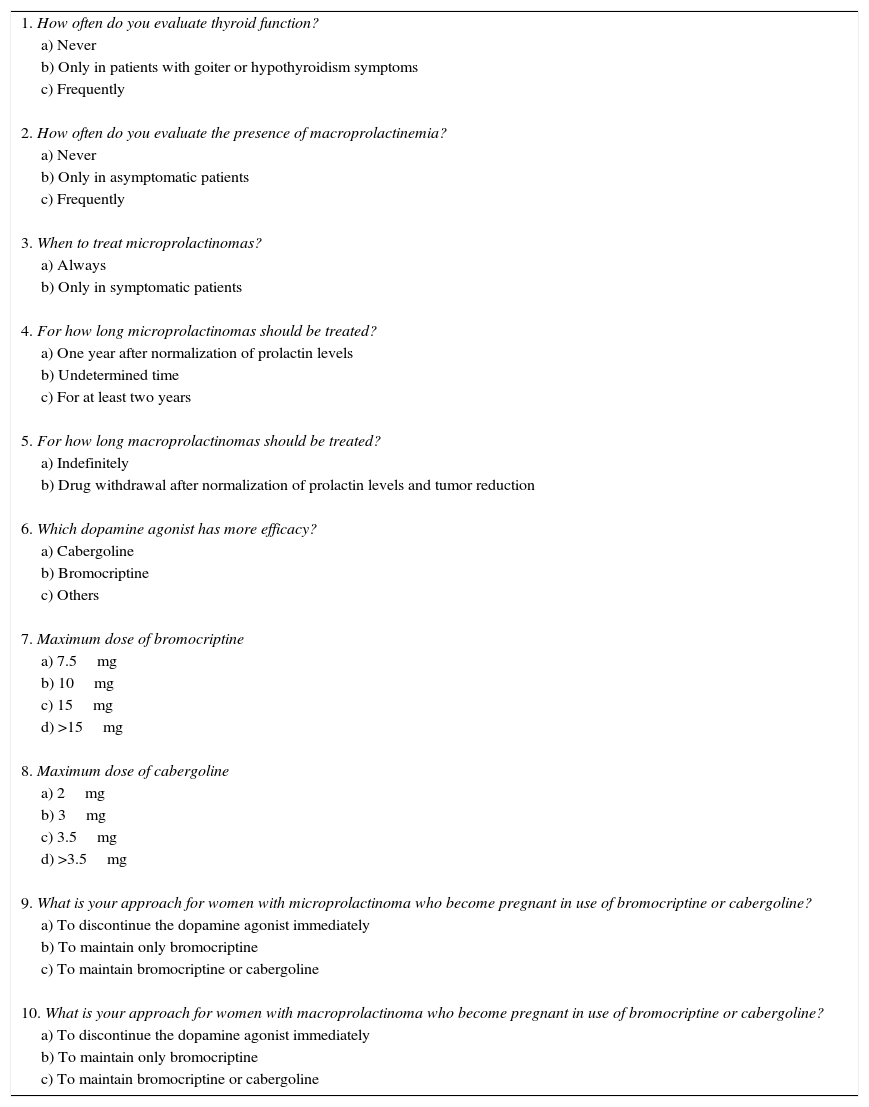
MethodsElectronic addresses of SBEM and FEBRASGO members were obtained from the directories of these societies, and these members were invited, through electronic messages (e-mail), to answer an online questionnaire that included 10 questions about controversial issues concerning the management of hyperprolactinemia (Table 1). For each question, the participant could select only one answer. The first two questions were about how to exclude primary hypothyroidism and macroprolactinemia in asymptomatic patients. Questions 3–5 addressed the treatment of micro and macroprolactinomas, and questions 6–8 inquired about the efficacy of bromocriptine and cabergoline and maximal doses of each drug. The remaining two questions dealt with hyperprolactinemia and pregnancy. The local ethical committee approved this study.
Questionnaire on the management of hyperprolactinemia.
| 1. How often do you evaluate thyroid function? |
| a) Never |
| b) Only in patients with goiter or hypothyroidism symptoms |
| c) Frequently |
| 2. How often do you evaluate the presence of macroprolactinemia? |
| a) Never |
| b) Only in asymptomatic patients |
| c) Frequently |
| 3. When to treat microprolactinomas? |
| a) Always |
| b) Only in symptomatic patients |
| 4. For how long microprolactinomas should be treated? |
| a) One year after normalization of prolactin levels |
| b) Undetermined time |
| c) For at least two years |
| 5. For how long macroprolactinomas should be treated? |
| a) Indefinitely |
| b) Drug withdrawal after normalization of prolactin levels and tumor reduction |
| 6. Which dopamine agonist has more efficacy? |
| a) Cabergoline |
| b) Bromocriptine |
| c) Others |
| 7. Maximum dose of bromocriptine |
| a) 7.5mg |
| b) 10mg |
| c) 15mg |
| d) >15mg |
| 8. Maximum dose of cabergoline |
| a) 2mg |
| b) 3mg |
| c) 3.5mg |
| d) >3.5mg |
| 9. What is your approach for women with microprolactinoma who become pregnant in use of bromocriptine or cabergoline? |
| a) To discontinue the dopamine agonist immediately |
| b) To maintain only bromocriptine |
| c) To maintain bromocriptine or cabergoline |
| 10. What is your approach for women with macroprolactinoma who become pregnant in use of bromocriptine or cabergoline? |
| a) To discontinue the dopamine agonist immediately |
| b) To maintain only bromocriptine |
| c) To maintain bromocriptine or cabergoline |
The results are predominantly given as percentages. The proportions of chosen answers for each question, between and within groups, were compared using the Goodman multinomial proportions test. p values <0.05 were considered statistically significant.
ResultsSurvey response and characteristics of respondentsWe received responses to the questionnaire by e-mail from 521 SBEM members (approximately 17% of total) and 233 FEBRASGO members (approximately 2% of total). The majority of respondents were either general endocrinologists or general gynecologists.
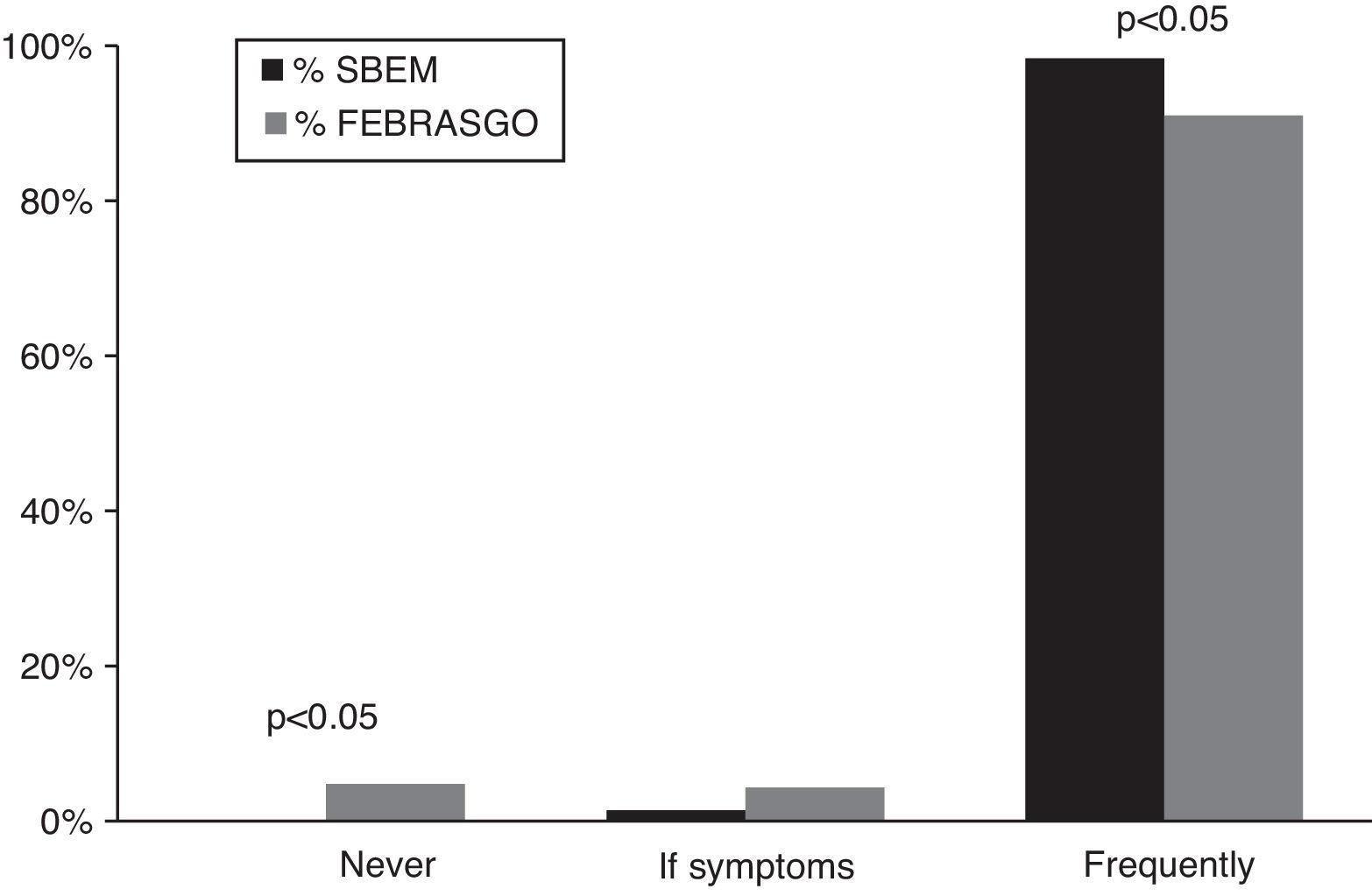
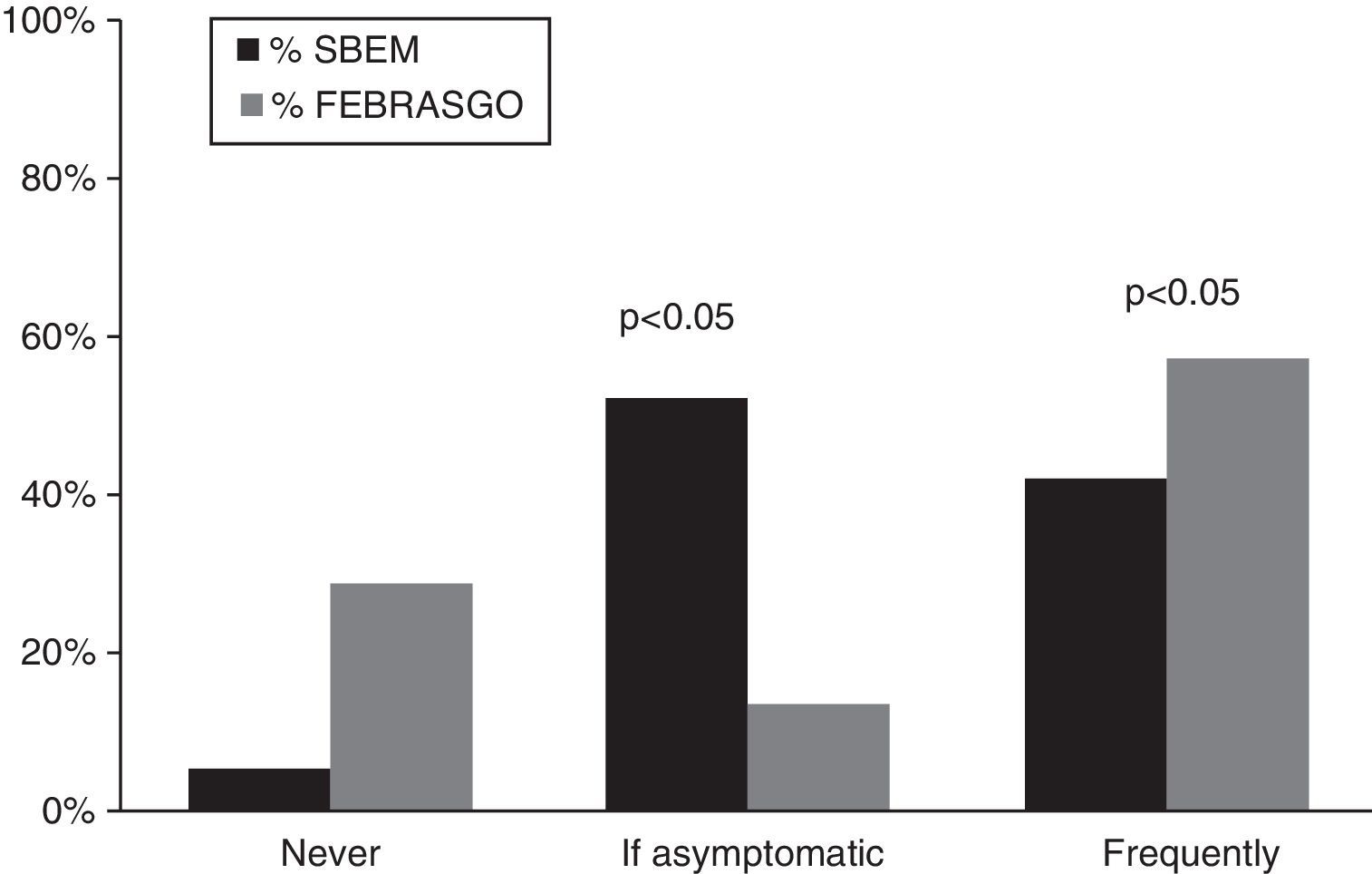
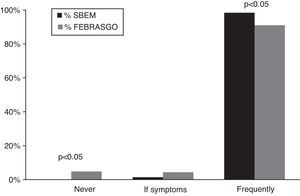
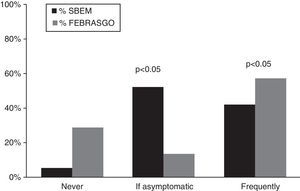
Diagnostic evaluation of hyperprolactinemiaTo exclude primary hypothyroidism, responders answered that they evaluate thyroid function frequently, more frequently in SBEM group (SBEM, 99% vs FEBRASGO, 91%; p<0.05) (Fig. 1). Gynecologists evaluate macroprolactin levels more frequently than do endocrinologists (FEBRASGO, 58% vs SBEM, 42%; p<0.05) (Fig. 2). On the other hand, more endocrinologists answered that they assess macroprolactin levels only in asymptomatic patients (SBEM, 52% vs FEBRASGO, 14%; p<0.05).
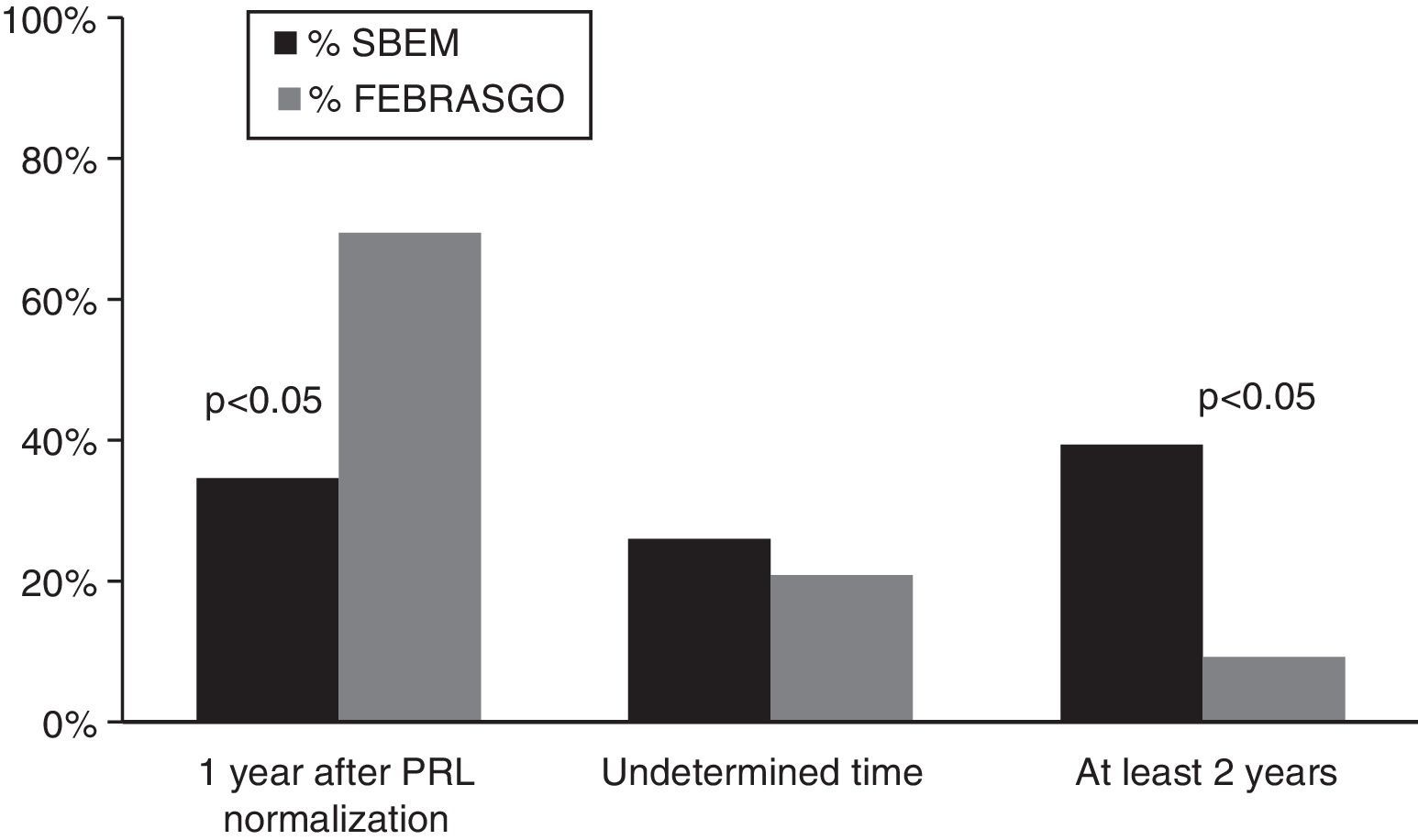
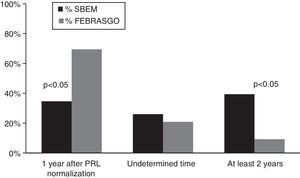
Prolactinoma treatmentTreatment of microprolactinoma did not differ between the groups; many choose to treat with a DA (SBEM, 57% vs FEBRASGO, 53%). SBEM members appear to treat for a longer duration than do FEBRASGO members (40% of SBEM members treat for at least two years, whereas 70% of FEBRASGO members continue the medication for one year after normalization of prolactin levels and improvement of symptoms; p<0.05) (Fig. 3).
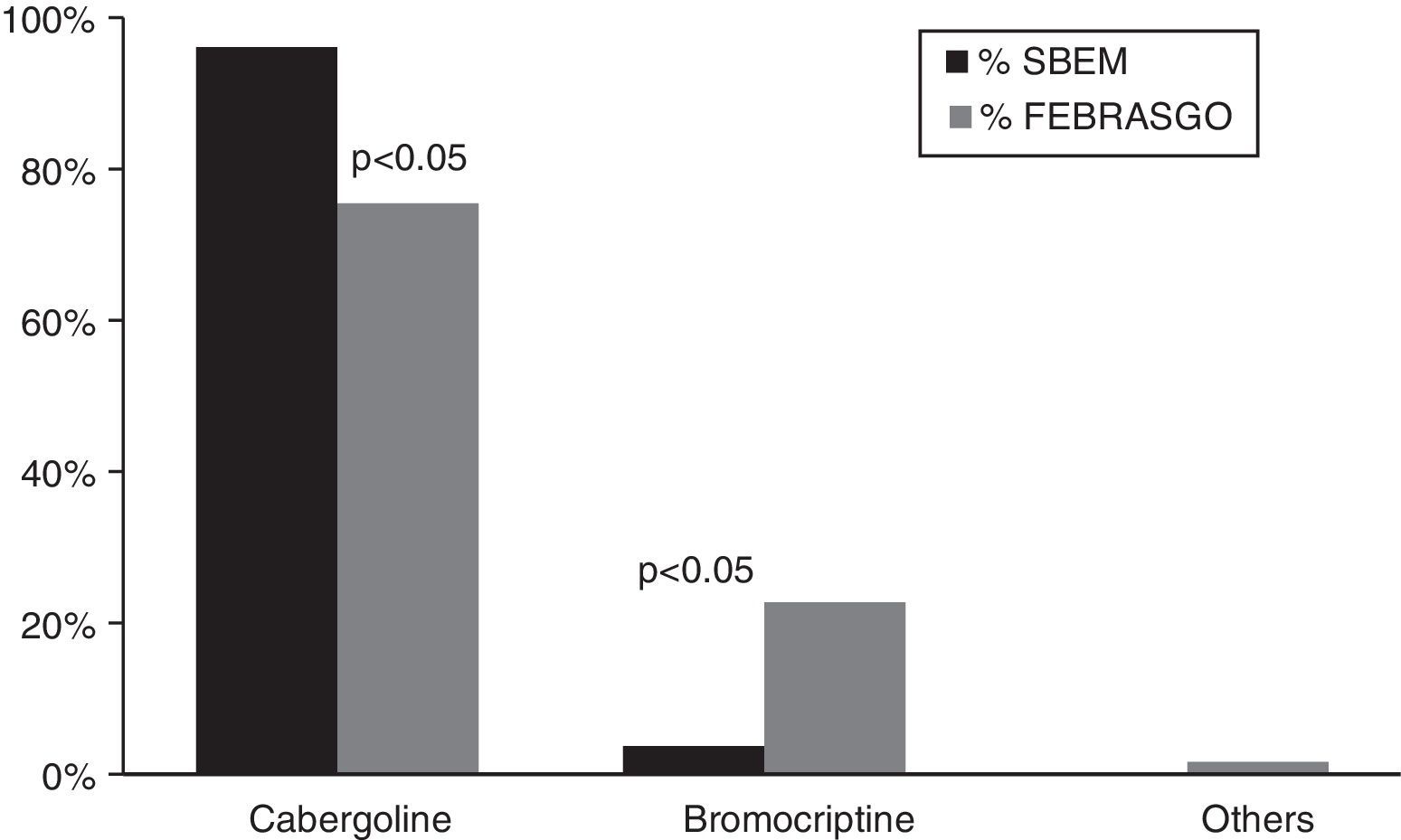
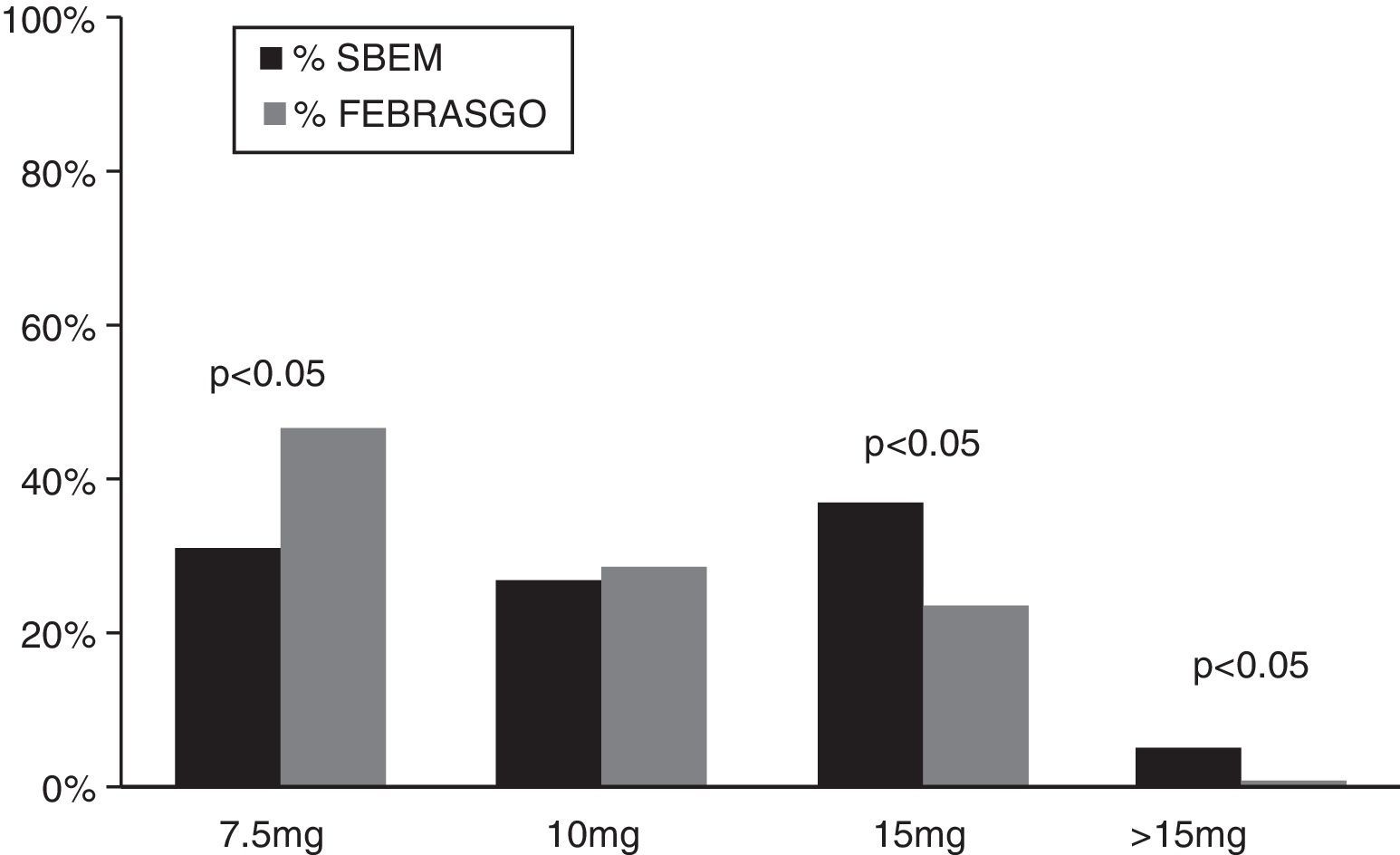
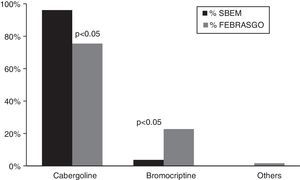
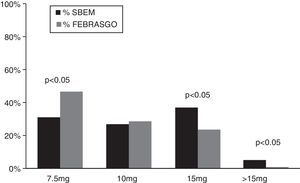
Concerning the treatment duration for macroprolactinoma, there was no difference between the groups; they both usually withdraw the DA an undetermined time after normalization of prolactin levels and tumor shrinkage (SBEM, 71%, FEBRASGO, 77%). Most respondents believe cabergoline is more effective and safer than bromocriptine (SBEM, 96% vs FEBRASGO, 75%; p<0.05) (Fig. 4). The maximum dose of bromocriptine most often prescribed by endocrinologists is 15mg, 37%, but gynecologists most frequently, 47%, prescribe 7.5mg (Fig. 5). Concerning maximum dose of cabergoline, many specialists do not prescribe more than 2mg per week (SBEM, 43% vs FEBRASGO, 56%).
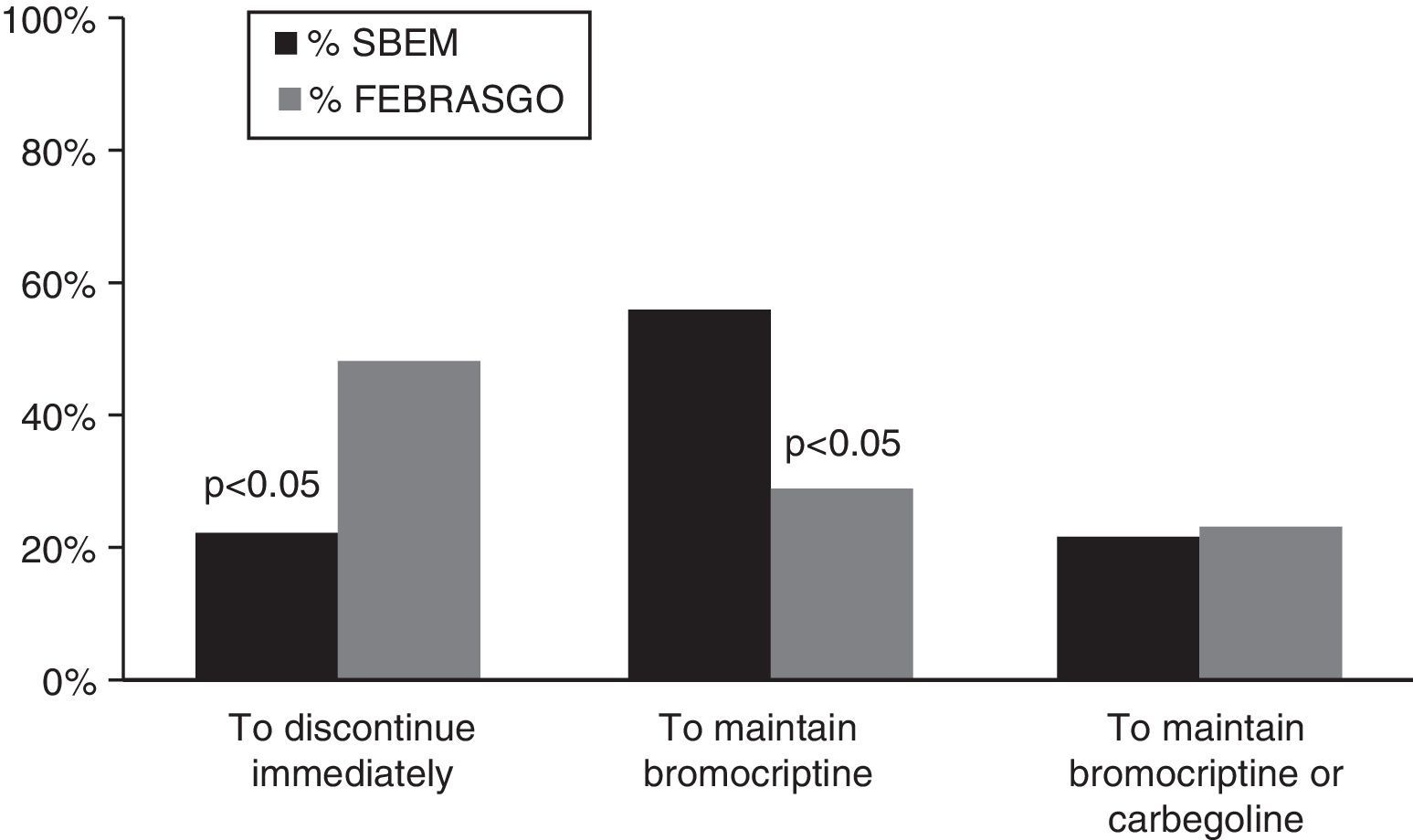
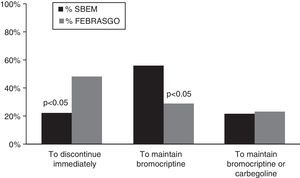
Prolactinoma and pregnancyFor women who become pregnant during therapy with a DA, most respondents recommend stopping drug treatment for microprolactinoma patients (SBEM, 82% vs FEBRASGO, 78%), with no difference between the groups. For individuals with macroprolactinoma, most of SBEM members would maintain treatment (SBEM, 56.1% vs FEBRASGO, 28.8%; p<0.05), but the majority of FEBRASGO members would interrupt therapy (SBEM, 20% vs FEBRASGO, 48%; p<0.05) (Fig. 6).
DiscussionDespite the simplicity of electronic media, few members answered our survey; the response rates were 17% and 2%, respectively, for SBEM and FEBRASGO members. Unfortunately, this limits the generalizability of our results; our data may not be representative of all SBEM and FEBRASGO members. The low response rate probably occurred due to lack of interest in the survey and the time interval that the survey was available. In a recently published survey of SBEM members about the same subject, the response rate was slightly higher (24%) than that of the current study.5
Although prolactinomas are the most important cause of pathological hyperprolactinemia, this disorder is also observed in approximately 40% of patients with primary hypothyroidism.6 Moreover, inadequate treatment of primary hypothyroidism may lead to pituitary hyperplasia, sometimes mimicking an adenoma.7 Therefore all evaluations of hyperprolactinemia must exclude hypothyroidism.2 In our survey, the majority of respondents answered that they usually evaluate thyroid function in patients with hyperprolactinemia; the SBEM group did so significantly more frequently (99% vs 91%).
Evaluation of hyperprolactinemia entails two potential diagnostic challenges: the presence of macroprolactin and the so-called ‘hook effect’.8 Macroprolactinemia is a condition defined as hyperprolactinemia with a predominance of the high-molecular isoform (>l00kDa) of prolactin, termed macroprolactin.9 Because this isoform has low bioactivity and bioavailability, macroprolactin is usually thought to occur in patients without classic symptoms of hyperprolactinemia.2 However, galactorrhea, infertility, and menstrual disorders may coincide with the presence of macroprolactinemia and some studies have confirmed this association.10–12 Therefore, to prevent misdiagnosis and costly spending, some researchers have suggested evaluating macroprolactin levels in all patients with hyperprolactinemia.13 In this survey, most endocrinologists answered that they measure macroprolactin only in asymptomatic patients, whereas most gynecologists frequently investigate this prolactin isoform (52% and 57% respectively). The proportion of respondents who answered that they evaluate macroprolactin levels was higher (42% vs 26%) than in a prior investigation that asked the same question of SBEM members.5 This increase may have been due to recent publications of the association macroprolactinemia with monomeric hyperprolactinemia.14,15
Several studies that compared cabergoline with bromocriptine for treating hyperprolactinemia demonstrated cabergoline's superior efficacy (reduction of prolactin levels, tumor shrinkage and restoration of gonadal function) and tolerability.16–21 In addition, two systematic reviews using meta-analysis reported that evidence favors the use of cabergoline over bromocriptine for the treatment of prolactinoma and idiopathic hyperprolactinemia.22,23 In the first review, cabergoline was superior in the normalization of prolactin levels, normalization of menstruation and induction of ovulation. It was also better tolerated than bromocriptine. On the other hand, bromocriptine has been satisfactorily used for years, yielding prolactin normalization in 48% to 72% of patients and tumor reduction to 70% of macroadenomas.20,24–27 In our survey, 96% of SBEM members responded that cabergoline is safer and more effective than bromocriptine. The majority of the FEBRASGO group answered the same; however, 23% responded that bromocriptine is the most effective DA. This was probably due to their limited experience with cabergoline and because they predominantly treat women who want to become pregnant, and the safety of bromocriptine has been studied in larger numbers of pregnancies than cabergoline.
Hyperprolactinemia treatment has changed some what during recently years, principally in the therapy of microprolactinoma and idiopathic hyperprolactinemia. The two last Endocrine Society guidelines suggested that asymptomatic patients harboring microprolactinomas should not be treated with a DA, because they rarely enlarge.2 In this survey, 56% of the SBEM group and 53% of the FEBRASGO group favored always treating microprolactinomas with a DA. On the other hand, in the SBEM group, the proportion of responders who only treats symptomatic patients was higher than in Vilar's survey (43% vs 25%, respectively).5 This suggests that endocrinologists have updated their understanding of this topic through conferences, web meetings and articles.
Increasingly, evidence indicates that patients with prolactinoma may have persistent normal prolactin levels without tumor enlargement after long-term DA therapy is discontinued.28–30 Therefore, the Endocrine Society recommends that therapy with the DA should be tapered and perhaps discontinued in patients who have been treated with a DA for at least two years, who no longer have elevated serum prolactin and who have no visible tumor remnant on magnetic resonance imaging.2 For treatment of patients with microprolactinoma, 35% of SBEM members and 70% of FEBRASGO members answered that they continue medicating for one year once prolactin levels have normalized and symptoms have improved;40% and 9%, respectively, treat for at least two years. In Vilar's survey, one-third of the endocrinologists favored discontinuing DAs 2–3 years after prolactin normalization and 48% recommended continuing treatment indefinitely.5 For treatment of patients with macroprolactinoma, 29% of SBEM and 24% of FEBRASGO members answered never suspending DAs, regardless of the evolution of the macroprolactinoma; 71% and 76%, respectively, discontinue the DA an unspecific time after prolactin normalization and tumor reduction. In Vilar's survey, 70% of respondents answered that they prescribe a DA indefinitely and 20% suspend the drug 2–3 years after prolactin normalization. This is further evidence indicating that endocrinologists have updated their knowledge of hyperprolactinemia treatment.
The fact that the endocrinologists see both women and men, and men are more likely to have aggressive macroprolactinomas, may explain why they prescribe maximum dose of DA higher than gynecologists do.
Finally, most responders replied that they withdrawal DAs immediately in women with microprolactinomas who became pregnant while receiving bromocriptine or cabergoline (82% of SBEM and 78% of FEBRASGO members). In patients with macroprolactinoma, 56% of endocrinologists responded that they continue the DA during pregnancy, whereas 48% of gynecologist preferred to suspend the drug immediately. According to the Endocrine Society Clinical Practice Guideline, women with prolactinoma should be instructed to discontinue DA therapy as soon as they discover that they are pregnant.2 However, for selected patients with macroprolactinoma, without prior surgical or radiation therapy who became pregnant while on DA therapy, medical treatment could be continued throughout the pregnancy, especially if the tumor is invasive or abuts the optic chiasm.2
In conclusion, the results of this survey demonstrate that there are many area of agreement between SBEM and FEBRASGO members and most of their responses follow the latest Endocrine Society Guideline. Relative to a survey performed several years ago, our findings show that SBEM members have incorporated some of latest recommendations in this field. The principal issues of concern for both groups are duration of DA treatment for patients with microprolactinoma and DA withdrawal during pregnancy.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestsThe authors have no conflicts of interest to declare.
This work was supported by Brazilian National Research Council, CNPq; grant N# 576445/08-8. We thank Brazilian Society of Metabolism and Endocrinology (SBEM) and the Brazilian Federation of Association of Gynecology and Obstetrics (FEBRASGO).