Introduction. Physical activity can provide long-term benefits for systemic lupus erythematosus (SLE).
Objective. This study sought to demonstrate the effects of progressive resistance training on the muscular strength, bone mineral density (BMD) and body composition of pre-menopausal women with SLE undergoing glucocorticoid (GC) treatment.
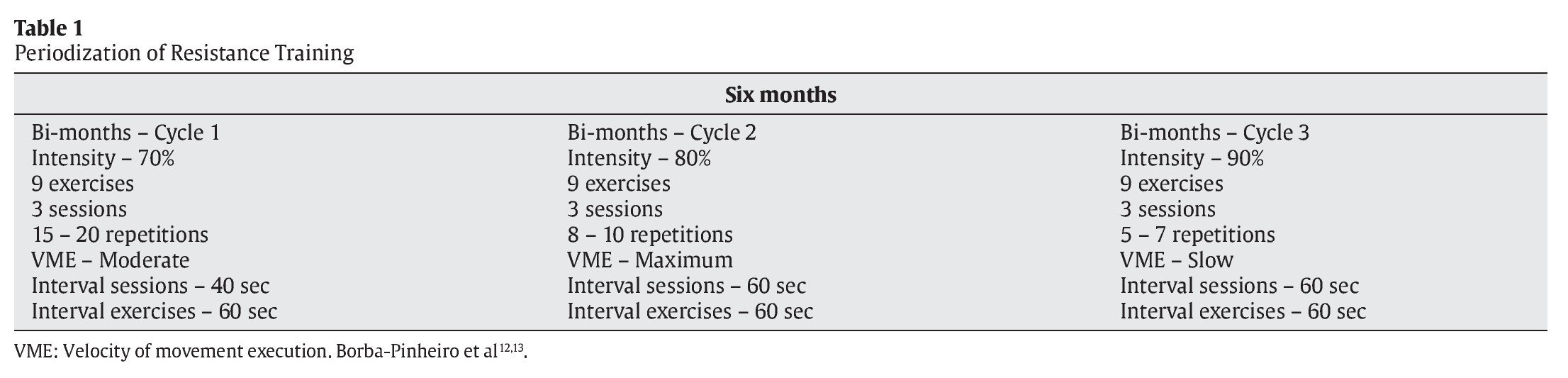
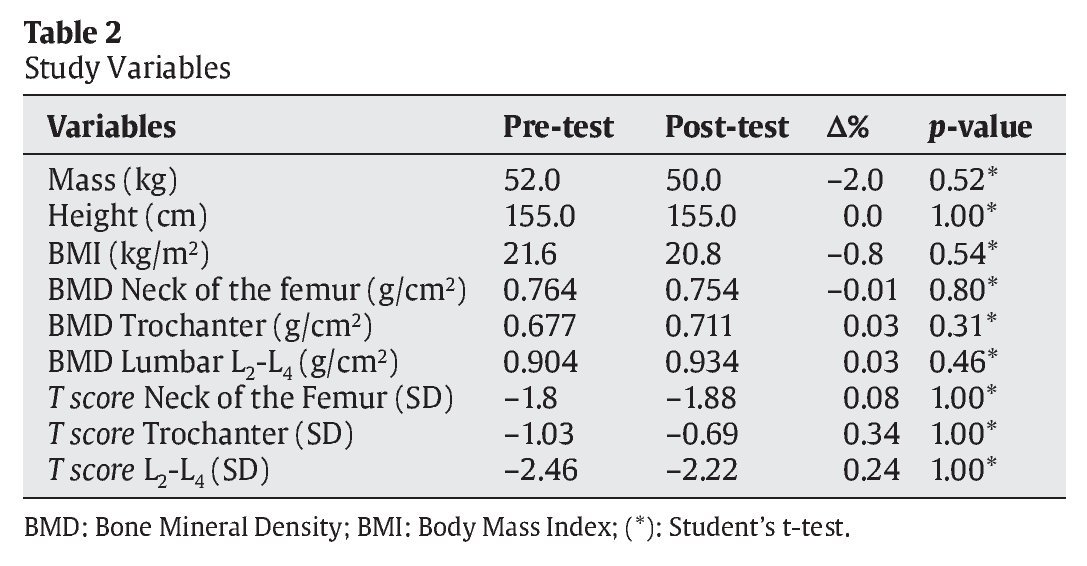
Materials and Methods. This is the case report of a 43-year-old African-South American premenopausal woman with non-extensive SLE and low bone density. A six-month program with three bimonthly cycles of 70%, 80%, and 90% intensity according to the 10 maximum-repetition test was used. Dual-energy X-ray absorptiometry (DXA) was used to measure the BMD, T-scores and body composition, and indirect fluorescence was used to measure the levels of antinuclear antibodies. Student's t-test was used.
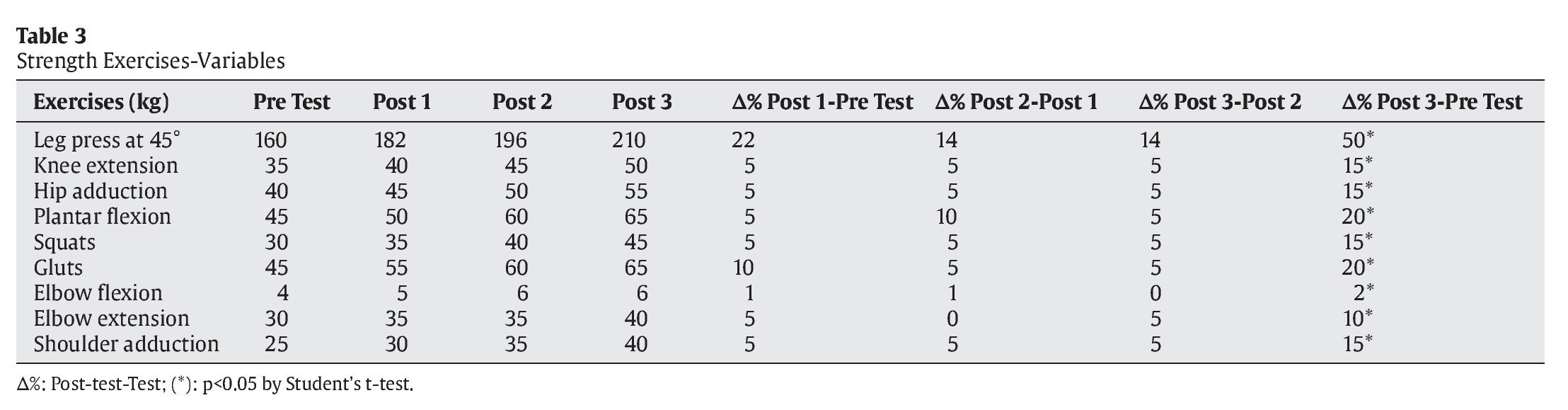
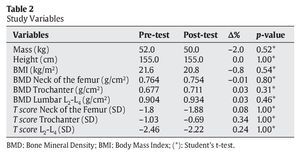
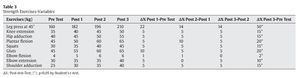
Results. Statistical improvement was noted in all strength exercises, including the 45° leg press (Δ%=+50%, p<0.001) and knee extension (Δ%=+15%, p=0.003) to maintain the BMD of the L2-L4 lumbar (Δ%=+0.031%; p= 0.46) as well as the trochanter (Δ%=+0.037%; p=0.31) and BMI (Δ%=-0.8, p=0.54).
Conclusion. In this case study, the presented methodology had a positive effect on strength and contributed to the maintenance of BMD and body composition in a woman with SLE undergoing GC treatment.
Introducción. La actividad física puede proveer beneficios a largo plazo para el lupus eritematoso sistémico (LES).
Objetivo. Esta investigación busca demostrar los efectos del entrenamiento de resistencia progresiva sobre: la fuerza muscular, la densidad mineral ósea (DMO) y la composición corporal de una mujer premenopáusica con LES sometido a tratamiento con glucocorticoides.
Materiales y Métodos. Una mujer con 43 años de edad, afrodescendiente, premenopáusica con LES sin gravedad y baja DmO fue sometida a programa de 6 meses con 3 ciclos bimestrales de 70, 80 y 90% de intensidad, considerando un test de fuerza máxima de 10 repeticiones máximas. Se utilizó, para medir la DMO, la absorptiometría de doble energía con rayos X, evaluando los T-scores, el índice de masa corporal y la fluorescencia indirecta para medir los anticuerpos antinucleares. Para la comparación de medias de variables, se utilizó el test de la T de Student.
Resultados. Se observó mejora en la fuerza, incluyendo (Δ% = 50%, p < 0,001) en la prensa de piernas de 45°, (Δ% = 15%, p = 0,003) en la extensión de la rodilla, como el mantenimiento de la DMO de la columna lumbar L2-L4 (Δ% = 0,031%, p = 0,46) y trocánter (Δ% = 0,037%, p = 0,31), además de mantener el índice de masa corporal (Δ% = -0,8, p = 0,54).
Conclusión. En este estudio de caso, se observaron efectos positivos sobre la fuerza muscular e indicios de mantenimiento de la DMO y de la composición corporal de una mujer con LES en tratamiento con glucocorticoides.
Introduction
Systemic lupus erythematosus (SLE) is a chronic inflammatory immune system disease of unknown etiology in which antibodies and immune complexes injure different cells and tissues1. The risk for SLE development has a genetic component that is often associated with environmental factors and lifestyle choices, such as solar , radiation exposure, stress, sedentary behavior, and the use of certain medications, that tend to trigger disease manifestation2.
SLE can occur in all ethnic and age groups, and it is more severe in children and young adults despite being more frequently diagnosed in women of reproductive age3. The SLE diagnosis was established by the American College of Rheumatology in 1982 and revised in 19974, and it is based on the presence of at least four of eleven criteria, including discoid lesions (erythematous), photosensitivity, arthritis (non-erosive with pain, swelling, and joint effusion) and abnormal titers of antinuclear antibodies (ANA)4. Although there are many criteria related to the SLE diagnosis, the positive result of ANA revealed by immunofluorescence may be indicative of the diagnosis5.
For the treatment of SLE, glucocorticoids (GC) are among the drugs used most commonly because they have an anti-inflammatory effect that reduces pain and immunosuppression, which inhibits the synthesis of autoantibodies6. However, the main adverse effects resulting from the prolonged use of GC include a reduction in bone mineral density (BMD)6. In addition, the sarcopenia is another effect that reduces muscle mass and consequently the strength with negative consequences for the functional autonomy, with an increased risk of falls7.
Most existent studies have investigated aerobic capacity8-11, and few studies have focused on the effects of resistance training (RT) in older women with SLE11.
The studies suggest that physical activity can provide long-term benefits for SLE8,10 and that measures aimed at improvement through physical exercise can contribute to overall functional performance, fatigability, social stress and quality of life in individuals affected by diseases that result in bone demineralization by helping to control BMD loss8,9,11.
Among the different types of physical activities, RT has demonstrated effectiveness in treating women with low BMD through effective control of the volume and intensity of loads to favor strength and BMD increases12-14. In addition, the RT can protect against sarcopenia. This process produces important and severe effects on the functional autonomy and quality of life in older women and is the most frequent cause of discapacity, dependency and increased or morbi-mortality7. However, few studies related to SLE and physical activity, especially regarding RT, have been presented in the literature8. Thus, this case study aimed to demonstrate the effects of progressive RT on BMD and muscle strength in premenopausal women with SLE treated with GC.
Materials and methods
The individual in this intra-subject study was a 43-year-old premenopausal female volunteer with normal ovulation, who was 155 cm in height and weighed 52 kg. The subject did not engage in any physical activity for four months, even though she used to practice RT and walked regularly before this period. She is an African-South American woman, whose disease was detected 15 years ago. However, she did not have extensive SLE, nor was her system compromised by lupus. In addition, the volunteer had a history of chronic arthritis with pain, edema and photosensitivity. The patient also presented ANA 1:160 (fine speckled), which can suggest the presence of positive anti-SSa/Ro. The fact that the patient presented negative anti-DNA and anti-Sm (Smith) does not exclude the diagnosis of lupus, as the patient did not present signs or symptoms of dry mouth syndrome, which rules out the diagnosis of Sjögren's syndrome.
The volunteer had normal functional activity and carried out her daily work activities. Her treatment, prescribed by the physician in charge, was based on the daily use of 7.5 mg/day of GC and 6 mg/kg/day of hydroxychloroquine sulfate; the dose was adjusted as necessary throughout the study period. In addition, the volunteer was not taking medication for anti-conception for more than 20 years and was also not taking medications such as bisphosphonates for low BMD. However, less than 5 years prior to the study, the volunteer had begun taking vitamin D+/day (400 UI). This regimen was continued throughout the study period.
The volunteer agreed to the presentation of her case for scientific research purposes by signing an informed consent form. The project was approved by the research ethics committee at the University Castelo Branco-RJ COMEP / PROCIMH under proposal number 0171/2008.
The osteopenia diagnosis was obtained using a dual-energy X-ray absorptiometry (DXA) machine manufactured by Lunar® (USA; DPX class with a 750-μA current, calibrated daily). A medical specialist performed the examination with the volunteer in a supine position on the equipment table with her legs supported at an immobile 30o angle. Scanning was performed in the region of the right femur and lumbar spine. The variables provided by DXA were body composition (height, mass and BMI), BMD (g/cm2) and negative T-scores for the lumbar spine L2-L4, femoral neck, and trochanter.
Based on the DXA, the BMD of the lumbar L2-L4 was 0.904 g/cm2 with a T-score of -2.46 standard deviations (SD). For the femoral neck, the BMD was 0.764 g/cm2 with a T-score of -1.80 SD; for the trochanter, the BMD was 0.677 g/cm2 with a T-score = -1.03 SD.
Because the subject had already practiced RT and did not present swollen joints or muscle soreness, the RT followed the timeline proposed by Borba-Pinheiro et al12,13 using bimonthly cycles, with the 10 maximum repetition test (10RM) performed at progressive intensities. The subject performed the 10 RM test at the beginning and the end of each cycle over the six-month training period (table 1). Each training session lasted sixty minutes and was performed three times per week on alternate days.
The volunteer performed nine exercises: the 45° leg press, knee extension, hip adduction, plantar flexion, gluts, squats, elbow flexion, elbow extension, and shoulder adduction. The equipment used for the training was manufactured by Pró-Physical® (Brazil).
Results
At the end of the six-month period, new evaluations were conducted, and the volunteer demonstrated maintenance of the BMD and T-scores. The absolute percentage difference was calculated by subtracting the initial test from the post-test [Δ% = post-test - pre-test]. Then, Student's t-test for BMD variables was used, as shown in table 2.
Table 3 presents the percentage improvements in muscle strength observed throughout the progressive load increase utilized in the three 10RM tests.
Discussion
The results achieved in this case report directly demonstrate the percentage increase of muscle strength in all of the performed exercises and the maintenance of the BMD of the lumbar L2-L4 and greater trochanter, although the volunteer used GC, which promotes a reduction in BMD. The low BMD of the volunteer may be attributed to the daily use of GC for the control of articular pain6.
In a similar studies, Borba-Pinheiro et al12,13 report that RT planned over a 12-month period for post-menopausal women, consisting of three weekly sessions and different bimonthly intensities, was effective for increasing muscle strength and the BMD of the lumbar L2-L4, femoral neck, and greater trochanter of the volunteers compared with those engaged in other activities and the control group.
Borba-Pinheiro et al12,13 emphasize that effective gains and the maintenance of muscle strength and BMD require periodized resistance training, which is corroborated by other studies13,14. In addition to the load test, the training program is based on individual biology in terms of the selection of exercises and the use of interdependent volumes and intensities to establish the number of exercises, sets, repetitions, breaks, weekly sessions and intensities that would serve each individual best4.
As to the relationship between SLE and physical activity, there are few reports addressing the effects. However, Ayan and Martin8 suggest that physical exercise can improve cardiovascular fitness, reduce metabolic abnormalities or fatigue and consequently contribute to an improved quality of life for individuals with this disease. The study performed by Carvalho et al9 reinforces this hypothesis because it reported a significant improvement in exercise tolerance, aerobic capacity, quality of life and depression symptoms after the completion of a supervised cardiovascular training program for patients with SLE.
In another study using two groups of volunteers with SLE, one performing aerobic training and the other performing strength training with 70-80% of the maximum load with 2-3 sets of 10 repetitions at three weekly 50-minute sessions, the exercises performed by both groups were considered safe and did not aggravate the symptoms of SLE over a period of eight months11. Individuals from both groups showed improvements in fatigue, functional capacity, cardiovascular fitness, and muscle strength11. In this same study, an increase in bone turnover was noticed; however, the BMD remained unchanged in both groups.
Our work revealed that during the study period, there was an improvement in the levels of muscular strength and BMD maintenance in the volunteer. These results suggest an alternative methodology based on RT to aid in the treatment of this disease, because the approach described here could also be used for prevention and treatment strategies that protect against sarcopenia7. A recent review reinforces the findings of this study, suggesting that physical activity may have direct effects on reducing the level of systemic inflammation in chronic autoimmune diseases15.
In this review, no adverse effects due to exercise were found in patients with autoimmune disease. The fact that no adverse effects were observed can be explained by the fact that the induction of stress caused by exercise may provide physiological function alterations in the immune system that can increase the associated defense mechanisms15.
Another study showed that an increase in body composition may be associated with osteopenia and sarcopenia in women with lupus16. This information confirms the importance of the present study because it can minimize the effects caused by disease through the possible maintenance of weight, body mass index and bone density with increasing muscle strength and, consequently, the control of sarcopenia, which is corroborated by other studies13-15.
This report suggests that the progressive RT associated with drug therapy can minimize the symptomatic autoimmune effects of SLE. In addition to increasing muscle strength, the control of BMD and can maximize these results in favor of a better quality of life for the volunteer. However, this case study also demonstrates the need for new studies of experimental and control groups to verify the effects of RT associated with the use of medication for SLE.
Conclusion
In this case study, the presented methodology had a positive effect on strength, and it may contribute to the maintenance of BMD and the body composition of women without extensive SLE who are required to undergo GC treatment.
Conflict of Interest
This study did not have financial support from any institution, so there are no potential conflicts of interest.
History of the article:
Received March 15, 2012 Accepted April 30, 2012
Correspondence:
C.J. Borba-Pinheiro.
Instituto Federal do Pará
Street Canadá n.° 40, District/Vila Permanente.
Postal Code 68464-000, Tucuruí-PA/Brazil.
E-mail:
borba.pinheiro@ifpa.edu.br