The physiological and energy demand responses to upper body aerobic exercises performed with different postures are not well known. The aim of the present study was to compare energy cost and physiological responses to upper body aerobic exercises performed with different postures.
MethodEight physically active males (>1 year active), untrained in upper body aerobic exercises, with 28.2±5.7 years, ht 173.7±7.4cm, body mass 74.1±11.4kg, VO2Peak 30.2±2.09ml/kg/min and Body Mass Index 24.4±2.5kg/m2 performed a preliminary maximal test and two upper body aerobic exercises 30-min sessions in different days.
ResultsMetabolic and hemodynamic responses to upper body aerobic exercises performed in sit-position and vertical-position were compared. The vertical-position trial showed greater total energy cost (14.3%; p=0.01), higher lipid catabolism (p=0.001) and a higher double product (p=0.04), when compared to the sit-position trial.
ConclusionThe upper body aerobic exercises performed in vertical-position induces a higher energetic demand and cardiovascular load than in sit-position.
Poco se conoce sobre la influencia de la variación de la postura sobre las respuestas fisiológicas y el gasto energético durante ejercicios con miembros superiores. El objetivo de este estudio fue comparar las respuestas fisiológicas durante ejercicios con miembros superiores realizados en diferentes posturas.
MétodoOcho hombres físicamente activos (>1 año), no practicantes de ejercicio con miembros superiores, con 28.2±5.7 años de edad, 173.7±7.4cm de talla, 74.1±11.4kg de masa corporal, VO2Pico de 30.2±2.09ml/kg/min e índice de masa corporal de 24.4±2.5kg/m2, fueron sometidos a un test máximo preliminar y a 2 sesiones de ejercicios con miembros superiores de 30min de duración, en días distintos.
ResultadosLas respuestas metabólicas y hemodinámicas, en la postura de sentado y vertical, fueron comparadas. La sesión de ejercicio con miembros superiores realizado en postura vertical generó mayor gasto energético total (14.3%; p=0.01), mayor catabolismo lipídico (p=0.001) y mayor doble producto (p=0.04), en comparación con la sesión realizada en postura sentado.
ConclusionesEl ejercicio con miembros superiores realizados en postura vertical eleva el gasto energético y la sobrecarga cardiovascular, en comparación con ejercicios con miembros superiores en postura sentado.
As respostas fisiológicas e de custo energético durante exercícios aeróbios de membros superiores realizados em diferentes posturas não são bem conhecidas. O objetivo do presente estudo foi comparar o custo energético e as respostas fisiológicas durante exercícios aeróbios de membros superiores realizados em diferentes posturas.
MétodoOito homens fisicamente ativos e não praticantes de exercícios aeróbios de membros superiores, com 28.2±5.7 anos de idade, 173.7±7.4cm de estatura, 74.1±11.4kg de massa corporal, VO2Pico de 30.2±2.09ml/kg/min e Índice de Massa Corporal de 24.4±2.5kg/m2, foram submetidos a um teste máximo preliminar e a 2 sessões de exercícios aeróbios de membros superiores com duração de 30min, em dias distintos.
ResultadosRespostas metabólicas e hemodinâmicas obtidas nas posturas sentada e verticalizada foram comparadas. A sessão de exercícios aeróbios de membros superiores realizado na postura verticalizada gerou maior gasto energético total (14.3%; p=0.01), maior catabolismo lipídico (p=0.001) e maior duplo produto (p=0.04), quando comparado com a sessão postura sentada.
ConclusõesO exercícios aeróbio de membros superiores realizado em postura verticalizada eleva o custo energético e a sobrecarga cardiovascular, quando comparado com oexercício aeróbio de membros superiores em postura sentada.
Upper-body exercises (UBE) can be inserted in training programs for health or improvement of athletic performance, especially in subjects with physical limitations or restrictions to perform lower-limbs exercises.1 When prescribed with the appropriate relationship between intensity and duration, UBE in a cycloergometer can compose a weight loss programs.2–4
The energetic cost of exercise be determined by, among other factors, the posture body assumed during performance.5 Thus, the posture is directly associated with mechanical power produced and the physiological demands.2,6,7 For example, changes on the posture during exercise causes redistribution of blood flow by changing the cardiac output and other hemodynamic responses such as: heart rate (HR), blood pressure (BP) and double-product (DP).8,9
Changes in posture can also change in the gas exchange during exercise. Ashe et al.6 compared cyclists in two different trunk positions: (a) vertical; and (b) parallel to the ground (aerodynamics), and found that the vertical posture changed the ventilation (VE) and increase the O2 consumption (VO2). The results demonstrated that the vertical posture increase the thorax expansion, allowing increased inspiratory volume and lower respiratory rate. Thus, it was suggested that changes in posture on UBE sessions with same intensity, produce different hemodynamic and metabolic adjustments, resulting also in a different energy cost exercise.
According to manufacturers, thousands of UBE were sold are present in clubs and gyms in many countries.4 Some equipment can be used in the seated position (SP) and in the vertical or orthostatic position (VP) and allow their cranks are moved independently, backward or forward, allowing great variability of movements.4,10 Indeed, the use of these devices may represent an advance on the inclusion of the paraplegics, because the exercise training can be realized completely seated. Considering also the growth of Paralympic sport,11 we believe that the use of UBE can be a training strategy for wheelchair cyclists on rainy days. Although, the use of this equipment can represent major expansion for this population, or between athletes with different levels of cardiopulmonary fitness,4,10 we consider poorly the scientific knowledge about the physiological responses during the UBE in different posture. It is possible that different posture adopted during UBE result in changes on energy cost. It is assumed that there is an increased energy cost in UBE sessions with VP, which could be characterized by greater VO2 response, VE and hemodynamic.
Therefore, we believe that the likely changes induced by manipulating the posture on the physiological responses and energy cost of UBE may contribute to the appropriate prescription of these exercises, supporting coaches with respect to greater effectiveness and safety of planning.12-14 Thus, the aim of this study was to compare the physiological responses during UBE realized in different posture.
MethodSampleBased on our pilot study (n=4) and the available literature, the sample size was calculated based on energy expenditure. To achieve 80% statistical power, it was calculated that a minimum sample of eight subjects would be necessary to detect an increase of 20kcal energy expenditure between group's (Granmo 5.2, IMIM®, Barcelona, Spain). The final sample was composed by 8 physical active men, with 28.2±5.7 years, 173.7±7.4cm of height, 74.1±11.4kg of body mass, 30.2±2.1ml/kg/min of VO2Peak and 24.4±2.5kg/m2 of Body Mass Index (BMI). On the experimental period, the volunteers were classified how physically active for at least 12 months and did not practice any type of aerobic exercises of the upper limbs. They do not present respiratory, neurological and vestibular disorders, changes in the electrocardiogram and blood pressure. After presented the risks and benefits of this study, the participants signed a free and informed consent form. All researches procedures were previously approved by the Ethics Committee of the University in which the study was conducted (protocol n.48/2014).
The data collection was divided into four stages: (I) an initial assessment with anamneses and pre-test examinations; (II) ergometry; (III) familiarization with the upper body cycle ergometer; (IV) UBE experimental sessions of 30min. The evaluations were conducted in a laboratory, with controlled temperature at ∼21°C, in the same period of the day. Volunteers were requested to make a light diet until two hours before the tests, and abstain from strenuous exercise for 24hours prior to the data collection.
ProceduresA standard anamneses was initially applied to trace the lifestyle and record the presence/occurrence of diseases and injuries of the participants. Then all volunteers rested (10min) on a stretcher to measure of the electrocardiographic signal (ECG) of 12 derivations. (Marquette Hellige v.3.0, CardioSmart®, Milwaukee, USA), rest Heart-rate (HRR) and rest blood pressure (BPR) (Missouri, Mikatos®, Embu das Artes, Brazil). A physician examined the results for ECG, HRR and BPR in comparison to the normal values for the health, in a presence of abnormality, the volunteer would be excluded from the final sample. Finally, anthropometric measurements of body mass and height were held in platform scale with coupled stadiometer (Personal Line, Filizola®, São Paulo, Brazil).
An upper-limbs CT was performed in a mechanic cycloergometer (M4100, CEFISE®, Nova Odessa, Brazil) how the beginning evaluation. After 60-seconds warm-up 15W load and 60 RPM cadence, the CT was beginning with increase of 15W/2min and fix cadence by 60 RPM to exhaustion. The end of test was determined by inability to maintain the pedal cadence at 60 RPM. The cardiopulmonary responses were obtained, breath-to-breath, by a gas analyzer (VO2000, MedGraphics®, St. Paul, MN, USA) with a software Ergo PC Elite 3.3 (Micromed®, Brasília, Brazil). Measurements how VO2 (ml/kg/min), VE (L/min), carbon dioxide (VCO2, ml/kg/min), respiratory quotient (RQ) and the ventilatory equivalents of O2 and CO2 (VE/VO2 and VE/VCO2, respectively) was obtained during the CT.
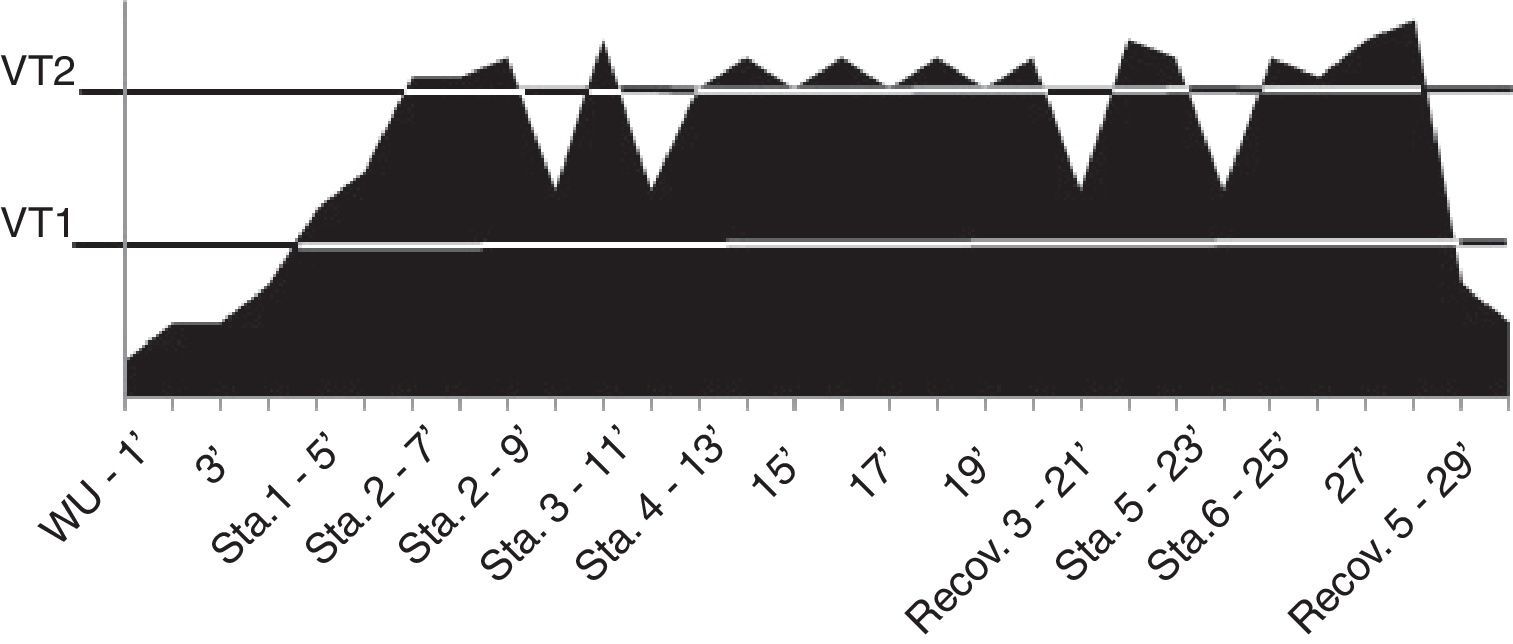
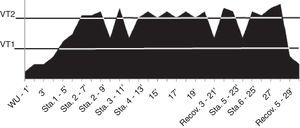
Before each test, the gas analyzer was calibrated according to the manufacturer's specifications, using known gas mixture of 17.0% O2 and 5.0% CO2. Peak VO2 being established as the arithmetic average VO2 in the final 20seconds on the last stage completed. In addition, ventilatory threshold (VT1 and VT2) were determinate15 considering the VT1 at the time of test in which we observed a nonlinear increase of RQ, concomitantly with lower values of VE/VO2. Whereas the VT2 was determined at the last point before the gradual increase in the VE values.15 The HR was measured during the CT through a bypass digital electrocardiograph (CM5, Micromed®, Brasília, Brazil).
For familiarization with the cycloergometer (III stage), each volunteer underwent two UBE sessions, lasting 30min. During these pre-tests participants performed consecutively: (I) 10min sitting by turning the handle forward and/or backward; (II) 10min in vertical position, turning the cranks forward and/or backward; (III) 10min of free movement. Each participant chose the direction that would like to turn the crank and this standard out for the experimental sessions. In pre-test exercise the intensity was monitored by Borg Scale (6–20).16 We stipulated that volunteers should keep the exercise intensity between 11 and 14 points of perceived exertion for 30min. The intake of ∼120ml of water was allowed.
The total energy cost for each UBE trial was calculated using the equation: 1L O2 consumed=5kcal/min; and 5.5kcal/L to 100% carbohydrate catabolism and 4.69 for fat catabolism.12 Given the limitations in obtaining the nitrogen balance in the exercise, we assumed the RQ non-protein. Thus, the catabolism rates of energy substrates such as fat and carbohydrate were obtained by kinetic response RQ (VCO2/VO2) throughout the exercise trial.
The experimental trial were random (phase IV) on two different days separated by 48–96hours and were composed by interval exercises with 30min each. Both UBE sessions SP and VP were performed with self-selected pace, the intensity was calculated by VT1 and VT2, to generate the metabolic demands: 20% intensity
During the UBE trial, VO2, VCO2, RQ, VE and HR were obtained continuously as previously described. Additionally, measurements of blood lactate (Accusport BM, Roche Diagnostics®, USA), systolic (SBP) and diastolic blood pressure (DBP) (Missouri, Mikatos®) were obtained two minutes before and immediately after the trial. Also, the estimated double product was calculated by multiplying HR by SBP for pre and post-trial.
Statistical analysisThe average and standard deviation, minimum and maximum values were determined to describe the results. The Shapiro–Wilk test was applied to determine the normal distribution. To compare trials (SP and VP) we applied t’-Student test for dependent samples (normal distribution) and Wilcoxon (non-normal distribution). The probability established was 5% and analyze were performed using SPSS version 10.0.
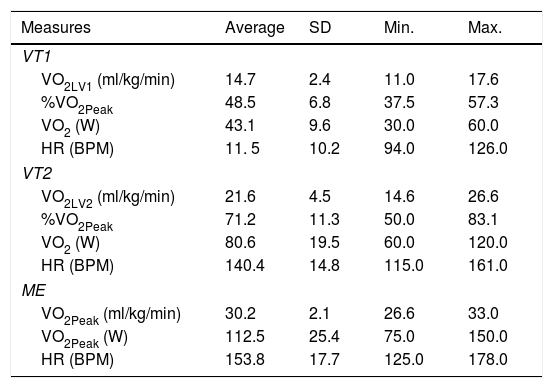
ResultsTable 1 presents the descriptive characteristics of the sample.
Descriptive characteristics (n=8) and thresholds VT1 and VT2.
| Measures | Average | SD | Min. | Max. |
|---|---|---|---|---|
| VT1 | ||||
| VO2LV1 (ml/kg/min) | 14.7 | 2.4 | 11.0 | 17.6 |
| %VO2Peak | 48.5 | 6.8 | 37.5 | 57.3 |
| VO2 (W) | 43.1 | 9.6 | 30.0 | 60.0 |
| HR (BPM) | 11. 5 | 10.2 | 94.0 | 126.0 |
| VT2 | ||||
| VO2LV2 (ml/kg/min) | 21.6 | 4.5 | 14.6 | 26.6 |
| %VO2Peak | 71.2 | 11.3 | 50.0 | 83.1 |
| VO2 (W) | 80.6 | 19.5 | 60.0 | 120.0 |
| HR (BPM) | 140.4 | 14.8 | 115.0 | 161.0 |
| ME | ||||
| VO2Peak (ml/kg/min) | 30.2 | 2.1 | 26.6 | 33.0 |
| VO2Peak (W) | 112.5 | 25.4 | 75.0 | 150.0 |
| HR (BPM) | 153.8 | 17.7 | 125.0 | 178.0 |
SD: standard deviation; Min.: minimum value; Max.: maximum value; VT1: ventilatory threshold 1; VT2: ventilatory threshold 2; ME: Maximum effort; VO2: peak oxygen consumption; VO2Peak%: percentage peak oxygen consumption; VO2 (W) load intensity is related to the consumption of oxygen or submaximal peak; HR: heart rate.
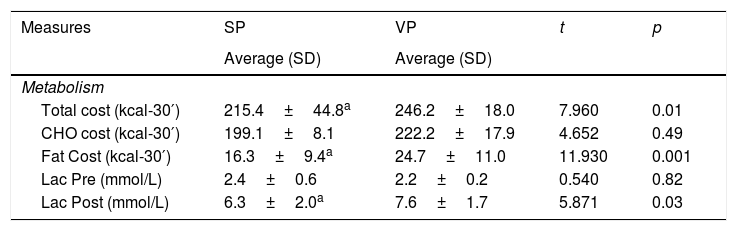
The results show that the total energy expenditure, lipid catabolism and the blood lactate concentration were lower (p<0.05) at the SP trial (Table 2).
Metabolic measurements for sitting (SP) and vertical position (VP).
| Measures | SP | VP | t | p |
|---|---|---|---|---|
| Average (SD) | Average (SD) | |||
| Metabolism | ||||
| Total cost (kcal-30′) | 215.4±44.8a | 246.2±18.0 | 7.960 | 0.01 |
| CHO cost (kcal-30′) | 199.1±8.1 | 222.2±17.9 | 4.652 | 0.49 |
| Fat Cost (kcal-30′) | 16.3±9.4a | 24.7±11.0 | 11.930 | 0.001 |
| Lac Pre (mmol/L) | 2.4±0.6 | 2.2±0.2 | 0.540 | 0.82 |
| Lac Post (mmol/L) | 6.3±2.0a | 7.6±1.7 | 5.871 | 0.03 |
SP: sitting position; VP: vertical position; SD: standard deviation; CHO: carbohydrate; Lac: blood lactate.
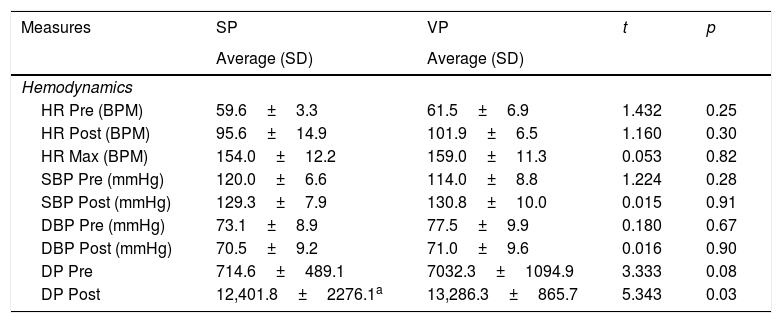
In VP was performed in a greater cardiovascular stress, considering the response of the double product when compared to the SP trial (p<0.05) (Table 3).
Hemodynamic measurements by sitting (SP) and vertical position (VP).
| Measures | SP | VP | t | p |
|---|---|---|---|---|
| Average (SD) | Average (SD) | |||
| Hemodynamics | ||||
| HR Pre (BPM) | 59.6±3.3 | 61.5±6.9 | 1.432 | 0.25 |
| HR Post (BPM) | 95.6±14.9 | 101.9±6.5 | 1.160 | 0.30 |
| HR Max (BPM) | 154.0±12.2 | 159.0±11.3 | 0.053 | 0.82 |
| SBP Pre (mmHg) | 120.0±6.6 | 114.0±8.8 | 1.224 | 0.28 |
| SBP Post (mmHg) | 129.3±7.9 | 130.8±10.0 | 0.015 | 0.91 |
| DBP Pre (mmHg) | 73.1±8.9 | 77.5±9.9 | 0.180 | 0.67 |
| DBP Post (mmHg) | 70.5±9.2 | 71.0±9.6 | 0.016 | 0.90 |
| DP Pre | 714.6±489.1 | 7032.3±1094.9 | 3.333 | 0.08 |
| DP Post | 12,401.8±2276.1a | 13,286.3±865.7 | 5.343 | 0.03 |
SP: sitting position; VP: vertical position; SD: standard deviation; HR (BPM): heart rate in beats per minute; SBP (mmHg): systolic blood pressure in millimeters of mercury; DBP (mmHg): Diastolic blood pressure in millimeters of mercury; DP: double product.
The results of this study suggest that UBE performed in the vertical posture increases the metabolic and hemodynamic responses. In fact, there was a 14.3% increase in total energetic costs as well as increased cardiovascular load associated with orthostatic stress (VP), corroborating previous findings.5 Only one study has investigated energy expenditure in specific cyclic trials of aerobic exercises in the upper limbs, Boyer et al.4 estimated energy expenditure of 269±87.8kcal for 30min sessions, an energy cost 8.5% higher in comparison with the present study. The higher energy costs4 depending on three factors: (I) the energetic cost of the trial was estimated by indirectly by HR and VO2; (II) the sample composed by more trained individuals; and (III) trial with alternating postures.
The lipid catabolism was altered, and matched the altered energetic expenditure between the two postures, so that the lipid catabolism was 51.53% in VP than in SP (p=0.001), despite the higher post-exercise blood lactate (p=0.03). Similar results were observed in subjects alternated body posture, however, without performing exercise.5 It can be suggested that the vertical position increase the lipid oxidation rates during the upper-limbs exercise.
In addition, other factors should be highlighted. In this study, the energy cost was established by indirect calorimetry, Boyer et al.4 predicted by a mathematical model. In addition, the sample of this study was formed by physically active subjects not practicing the UBE. Thus, it is suggested that the lower accuracy of the predictive model used in the study of Boyer et al.,4 compared to indirect calorimetry,12 well as the characteristics of the sample (trained individuals tend to choice higher self-selected intensities) can justify, at least in part, the differences in results between this study and other to which it was compared.
Possibly exercise in the vertical posture raise the energy demands of the muscle groups responsible for maintaining stand body posture, especially on the trunk and lower-limbs.7 Two studies17,18 showed that the contraction of muscles of the lower-limbs is dependent on the high perfusion pressure developed in the standing posture to generate muscle contraction. Thus, the change from the sitting to vertical position triggers, a compensatory response, that increase the modulation of the central command and yours afferent, increasing blood pressure during exercise.19,20 This compensatory mechanism is dependent on the increased sympathetic activity and the consequent reduction of the vagal modulation, for mediating the regulation of distribution of blood flow and maintaining blood pressure in the VP during physical exertion, which might justify the higher energetic cost in VP compared to SP.13
Regarding the hemodynamic adjustments, although most of the variables have not shown significant differences between the conditions, the data obtained in the VP condition had higher average values after exercise, compared to SP. These results can be interpreted as a major cardiovascular work for the maintenance of homeostasis in the VP.14
Despite the lower energy expenditure measured, UBE at SP presents itself as an exercise alternative for people that have difficulty in exercising in stand up position, for example, wheelchair users, obese and unable elderly.10,20 The concern in prescribing exercise to these populations is linked to the limited mobility of subjects, which increases the propensity to sedentary behavior.21,22 Certainly, studies on energetic expenditure have pointed out the total time sitting as responsible for the chronic diseases such as obesity and diabetes type II.23,24 Among the limitations of this study, the volunteers realized the exercise trial of free choice, since the ergometer used allows. Another factor would be to perform the measurement in a single trial, most measures may have a better metabolic profile as the energetic cost on VP or SP, as well as conducting classes with mixed posture and monitoring of post-exercise energy expenditure.
We conclude that upper body aerobic exercises in a vertical position raise the energetic cost, lipid catabolism and cardiovascular stress, compared to siting trial with the same intensity. These results should be considered in the systematization of upper-limb exercise training, since understanding the effects of posture change on the energetic cost and physiological responses allows a better prescription for the different goals of exercise practitioners.
Conflicts of interestThe authors have no conflicts of interest to declare.