Oropharyngeal neuroglial choristomas are exceptionally rare head and neck tumours that contain mature neuroglial tissue. We report a case of neuroglial choristoma centred in the oropharynx and extending into the parapharyngeal space that, to the best of our knowledge, is the only case whose appearance simulated brain cortical gyri with an apparent differentiation between white and grey matter. We illustrate and detail the magnetic imaging findings of oropharyngeal choristoma that might help to establish a correct preoperative diagnosis.
Los coristomas neurogliales orofaríngeos son tumores de cabeza y cuello excepcionalmente raros que contienen tejido neuroglial maduro. Presentamos un caso de coristoma neuroglial centrado en la orofaringe y con extensión al espacio parafaríngeo que, hasta donde sabemos, es el único caso cuya apariencia simulaba circunvoluciones corticales cerebrales con una aparente diferenciación entre sustancia blanca y gris. Ilustramos y detallamos los hallazgos de imágenes por resonancia magnética del coristoma orofaríngeo que podrían ayudar a establecer un diagnóstico preoperatorio correcto.
Neuroglial choristoma (or heterotopic brain) consists in a developmental lesion composed by histologically mature neuroglial tissue, isolated from the central nervous system.1,2 These lesions may be also described as glioneural hamartoma, brain heterotopia, heterotopic brain and ectopic brain and are divided into nasal (also known as nasal gliomas, although inappropriate, as they are not true neoplasms) and non-nasal heterotopias.3,4 Nasal glial choristomas are not uncommon and have an estimated incidence of 1 per 20,000 to 40,000 live births; however, few cases of non-nasal glial choristomas have been reported, the majority of which being of the parapharynx (12% of non-nasal heterotopias), palate (11%), mastoid (9%), tongue (9%), scalp (8%) and nasopharynx (5%).5 Neuroglial choristoma usually affect midline structures and off-midline lesions are rare.6 We report a case of neuroglial choristoma centred in the oropharynx and extending into the parapharyngeal space in a newborn. This study complied with the Declaration of Helsinki and the Resolution 196/96 of the Brazilian National Council of Health regarding research involving humans. Due to the retrospective nature of this study, the need for informed consent was waived.
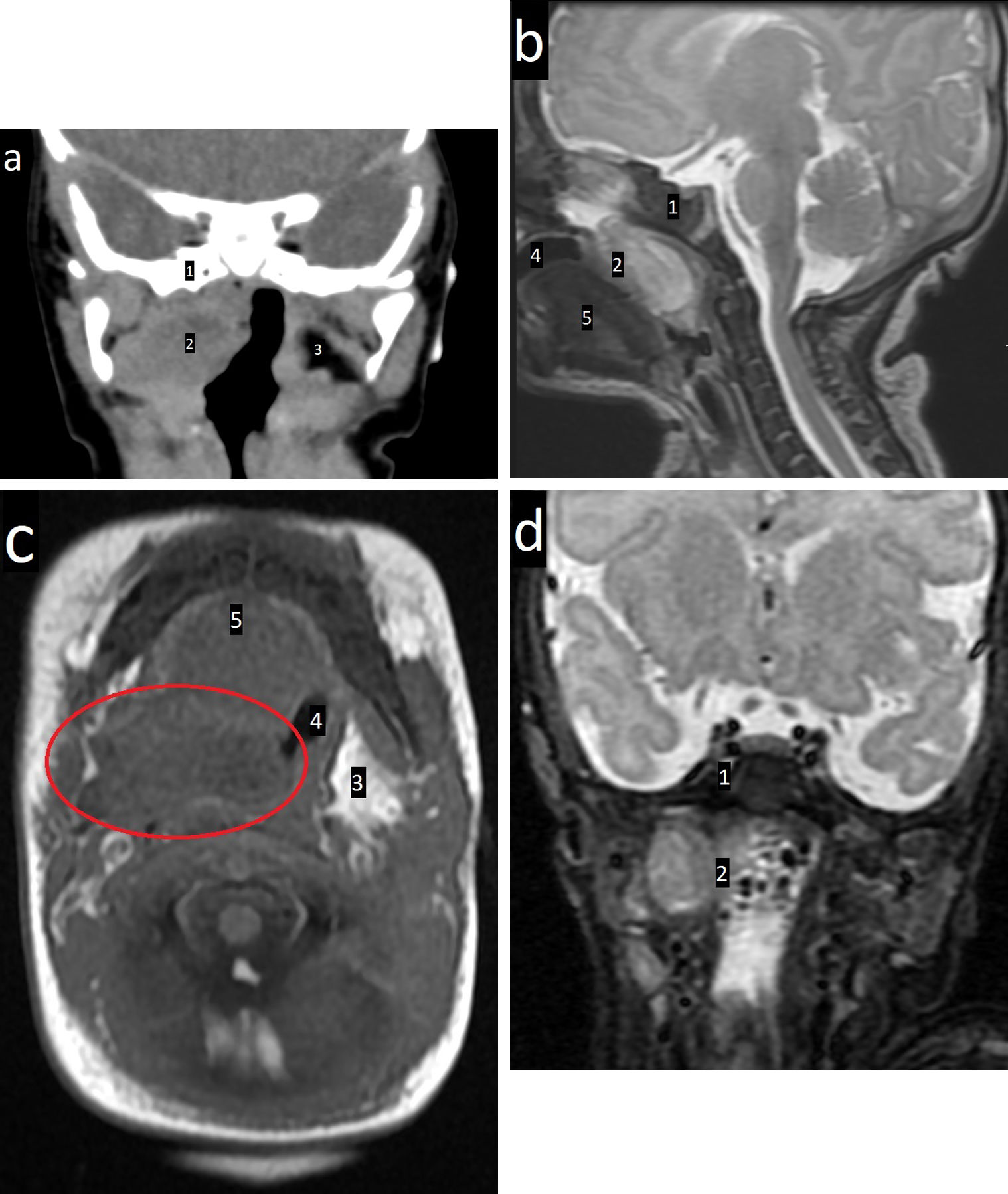
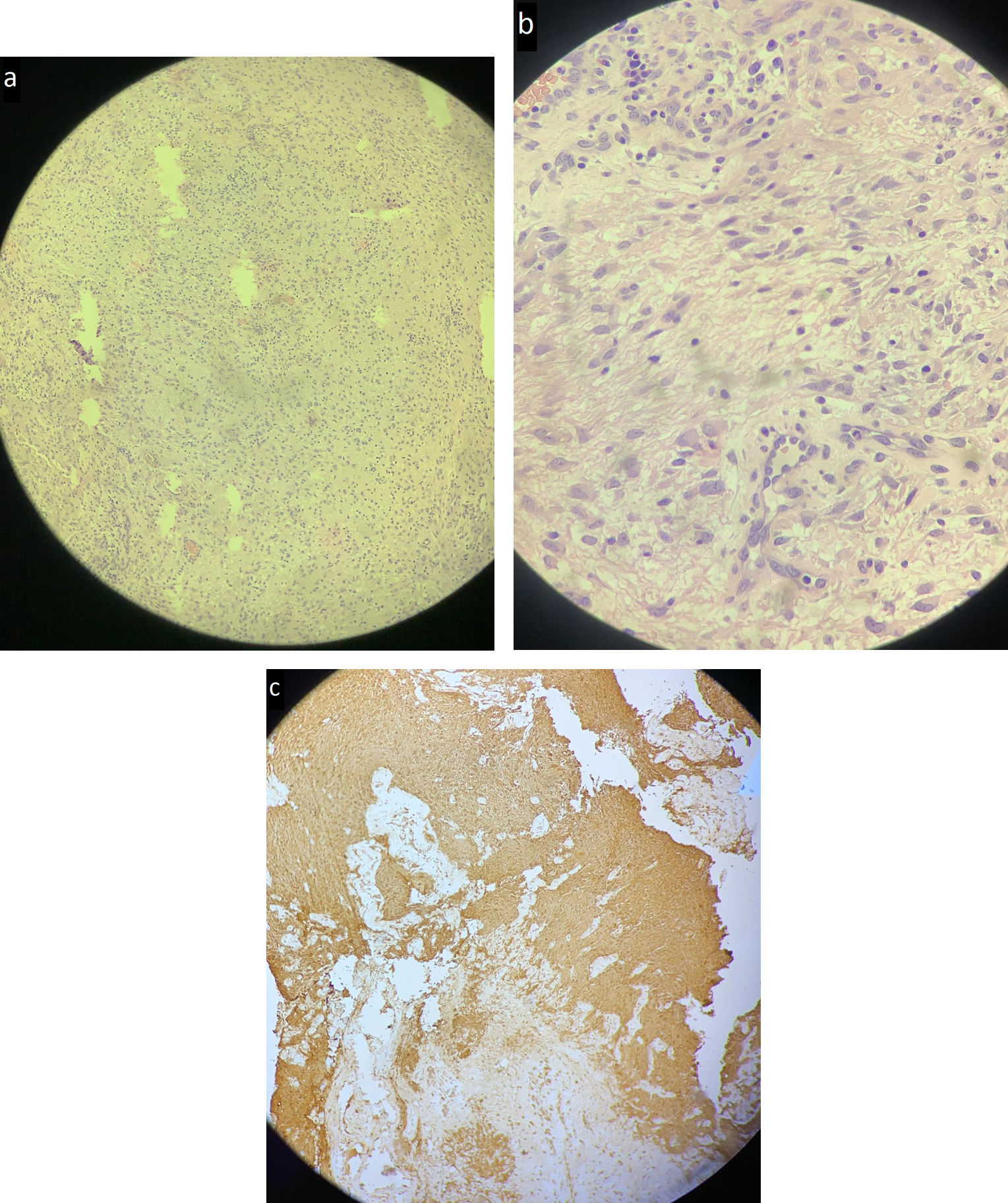
Case reportFemale term neonate presented respiratory distress since birth requiring mechanical ventilation. Computed tomography (CT) and magnetic resonance imaging (MRI) performed with 11 days of life depicted a mass centred in the oropharynx and extending into the parapharyngeal space with similar morphology and signal intensity to the brain, without communication with the central nervous system, suggestive of a neuroglial choristoma (Fig. 1). She underwent partial resection by an oral approach to collect material for pathology. Pathology showed glial tissue positive for S100 and glial fibrillary acid protein, confirming the diagnosis of neuroglial choristoma (Fig. 2).
Non-enhanced face computed tomography in the coronal plane, perpendicular to the hard palate (a) and magnetic resonance imaging of the neck in sagittal T2 (b), axial T1 (c) and coronal STIR (d) sequences. Integrity of the bony structures at the base of the skull is observed (1). There is a mass (2 and red circle) centred in the oropharynx with extension into the right parapharyngeal space (compare with the contralateral space, 3). Note the reduction of the oral cavity (4) and oropharyngeal patency (the mass reaches up to the body of the tongue, 5); and the brain-like appearance of the mass with a morphology that resembles cortical gyri, hypointense grey matter and hyperintense unmyelinated white matter in STIR sequence (d).
Oropharyngeal neuroglial choristomas are exceptionally rare lesions, with less than 10 cases reported in the literature.5 To our best knowledge, this is the only case of neuroglial choristoma whose appearance simulated brain gyrus with an apparent differentiation between white and grey matter in MRI. Regarding the aetiology of brain heterotopias, some argue that they derive from an encephalocele with loss of the central nervous system connection1; however, others claim an origin from the neural crest cells, which are also capable of undergoing neuroglial differentiation.1 Histopathology usually shows mature glial tissue (astrocytes with single or multiple basophilic nucleus and eosinophilic fibrillar cytoplasm), with sparse fibrous or muscular tissue, oligodendrocytes (arranged in a row or grouped), liquid content similar to cerebrospinal fluid produced by a choroid plexus, and immunohistochemistry is usually highly positive for S100 and glial fibrillary acid protein.6
Pharyngeal neuroglial ectopia usually presents at birth or early childhood with respiratory distress and is often associated with cleft palate, Pierre Robin syndrome, congenital heart disease, pectus excavatum and micrognathia.1,5,6 Other symptoms may include progressive dyspnoea and dysphagia.6 Imaging exams are essential for lesion localisation, extension assessment, diagnosis and surgical planning.6 CT is particularly useful to rule out anterior fusion defects of the skull and MRI may identify a mass with a signal intensity similar to brain tissue and cystic component with signal intensity similar to intracranial cerebrospinal fluid in T1 and T2 weighted sequences.6,7
The differential diagnosis of oropharyngeal glial choristoma includes encephalocele (associated with a defect usually in the posterior region of the cribriform plate or in the clivus), teratoma (may contain adipose tissue and calcifications), vascular malformations (transpatial multilocular cystic lesions) and, less likely, sarcomas (lesions with diffusion restriction and early contrast enhancement in dynamic imaging).1,3,5–9
The definitive treatment consists of excision through a transoral resection (access to the oropharyngeal component) which can be associated with a lateral transzygomatic incision and transcervical-transparotid approach (access to the parapharyngeal component).4,5 The prognosis is excellent in case of complete resection, but it can recur in up to 10% of incomplete resection cases.1,3,6
ConclusionThe hypothesis of neuroglial choristomas should be considered when an oropharyngeal mass with a similar aspect to the brain is characterised in the absence of anterior skull fusion defects.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
AuthorshipResponsible for the integrity of the study: AV.
Study conception: BMP.
Study design: AV.
Data acquisition: AV.
Analysis and interpretation of the data: AV.
Statistical processing: AV.
Literature search: AV.
Drafting of the manuscript: AV, PBM, BMP.
Critical review of the manuscript with relevant intellectual contributions: AV, PBM, BMP.
Approval of the final version: AV, PBM, BMP.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Vaz A, Bosquirolli Maffezzolli P, Maurício Pedrazzani B. Coristoma neuroglial orofaríngeo con extensión al espacio parafaríngeo. Radiología. 2022;64:270–273.