To evaluate the added value of administering intravenous contrast (IVC) routinely to the MRI of patients with audiovestibular symptoms in the assessment of a neuroradiologist and a resident.
Materials and methodsRetrospective study including patients who had an inner ear MRI for two months. Two radiologists reviewed independently and blinded the images. A first assessment was made analyzing just the sequences acquired without contrast and then a second evaluation of all the sequences, including post-contrast T1 sequences. The interobserver correlation and the correlation between MRI findings and the reason for requesting the study were calculated.
Results40 patients were included. The range age was 36–80 years. The most frequent reason for request the MRI was hearing loss (52.5%). Neuroradiologist without IVC found 82.5% of extraotic pathology and 17.5% of otic pathology, highlighting the neurinoma of the VIII pair (7.5%); ossifying labyrinthitis, retrofenestrated otosclerosis and cholesteatoma. After IVC administration, findings were similar. The resident identified otic pathology in 5% in baseline sequences and 20% using CIV. The interobserver correlation using IVC was excellent (0.97), but weak without IVC (0.52). There was a correlation between the reasons for request the MRI and the findings in the ears, both in protocols without IVC (p=0.004) and in protocols with IVC (p=0.002).
ConclusionInner ear MRI without contrast gives relevant information to assess audiovestibular symptoms. The use of IVC increases the degree of confidence in a novel radiologist, while in the expert its use is less relevant. A protocol should be proposed in which gadolinium is used in selected patients.
Evaluar el valor añadido que aporta administrar contraste intravenoso (CIV) rutinariamente en las resonancias magnéticas (RM) de pacientes con síntomas audiovestibulares en la lectura de un neurorradiólogo y un residente.
Material y métodosEstudio retrospectivo que incluía pacientes que durante 2 meses se realizaron una RM de oídos. Dos radiólogos revisaron las imágenes de forma independiente y cegada. Se realizó una lectura analizando las secuencias adquiridas sin contraste, y posteriormente una segunda lectura analizando todas las secuencias, incluidas las secuencias T1-poscontraste. Se calculó la correlación interobservador y la correlación entre los hallazgos en RM y el motivo de solicitud.
ResultadosSe incluyeron 40 pacientes. El rango de edad fue de 36-80 años. El motivo de solicitud más frecuente fue hipoacusia (52,5%). El neurorradiólogo sin CIV encontró un 82,5% de patología extraótica y un 17,5% de patología ótica, entre las que destacaba un neurinoma del VIII par (7,5%); también laberintitis osificante, otosclerosis retrofenestrada y colesteatoma. Tras la administración de CIV, los hallazgos fueron similares. El residente identificó patología ótica en el 5% en las secuencias basales y un 20% usando CIV. La correlación interobservador usando CIV fue excelente (0,97), pero débil sin CIV (0,52). Existió correlación entre los motivos de solicitud y los hallazgos en los oídos, tanto en los protocolos sin CIV (p = 0,004) como en los protocolos con CIV (p = 0,002).
ConclusionesLa RM de oídos sin contraste da información relevante para valorar síntomas audiovestibulares. El uso de CIV aumenta el grado de confianza en un radiólogo novel, mientras que en el experto su uso es menos relevante. Se debería plantear un protocolo en el que se use gadolinio en pacientes seleccionados.
Audiovestibular symptoms (hearing loss, vertigo, tinnitus, etc.) are of high prevalence and affect more than 360 million people in the world.1 The pathology of the inner ear is, therefore, a common reason for conducting neuroimaging studies. The striking thing is that many of these tests turn out to be normal, with incidental findings in up to 47.5% of patients that have nothing to do with the ear, and only 1.7% of clinically relevant pathology.2 This results in unnecessary consumption of resources, including radiologist time, machine time and use of intravenous contrast (IVC).3 If the study time is prolonged (when using IVC one more sequence would be necessary), there is more exposure to noise and a greater risk of cochlear function, especially in the T1 sequence, which is especially noisy.4,5
In addition, there is a growing concern in the scientific community warning of gadolinium deposition in the brain6 and its kidney effects7 (although the latter are increasingly questioned), which forces us to consider a more restrictive use of it.
Over time, there has been a change in the need to use IVC. It has gone from being indispensable in the diagnosis of ear pathology,8 to being more and more dispensable. In specific situations, such as in the screening of acoustic tumours,9–11 and mainly in the diagnosis of small schwannomas,12–14 the use of IVC could be justified. Also in the postoperative control of the middle ear.15 In the study of sensorineural hearing loss, IVC went from being used always16,17 to showing that the T2 sequence without IVC may be the most cost effective,18,19 just as in enlarged vestibular aqueduct syndrome.20
Therefore, the radiologist must question whether it is necessary to use IVC in MRI studies of the ears and assess whether protocols could be created in which IVC is used taking into account individually the pathology of each patient. In addition, the assessment of ear studies has a learning curve, so a radiologist in training may more often need the additional information provided by the contrast medium.
The objectives of this study are: to make a descriptive study of the findings visualized in MRIs of the ears, assessing the sequences without and with contrast between a neuroradiologist and a resident, calculating the correlation coefficient between both readings, and describing the added value provided by the routine administration of IVC.
Materials and methodsThe research ethics committee of Galicia approved this study, and it was not considered necessary to request informed consent from the patients included.
Study designIt is a retrospective study in the hospital setting. During a period of two months (May and June 2018), all patients whose only inclusion criterion was to have an MRI of the ears during that period were included. In this group of patients, demographic data and the reason for requesting the study were collected.
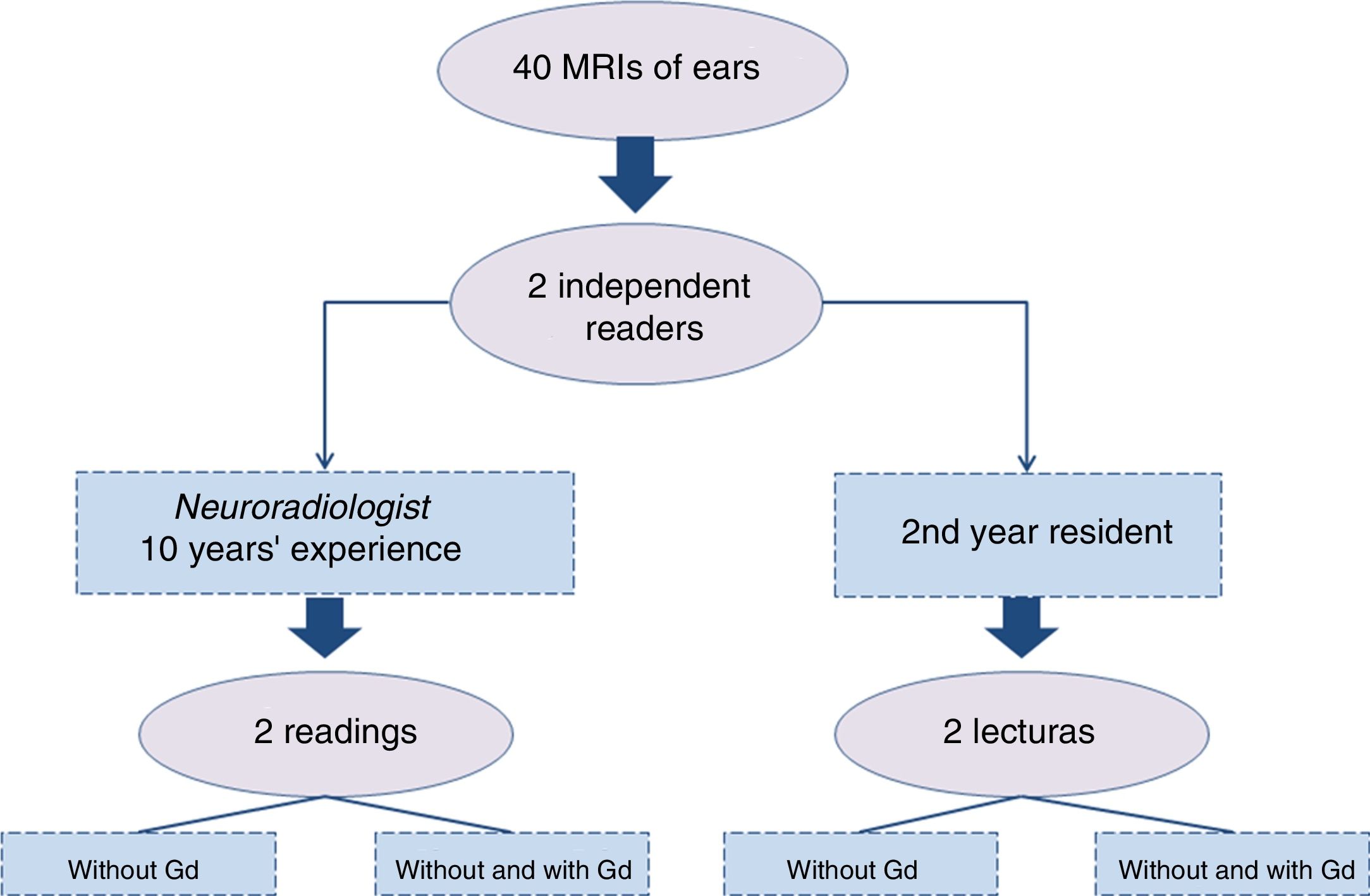
The 40 MRIs of ears obtained were interpreted by two readers, a neuroradiologist and a radiology resident. Both conducted independent readings, blinded with respect to clinical information, anonymised and randomized (Fig. 1).
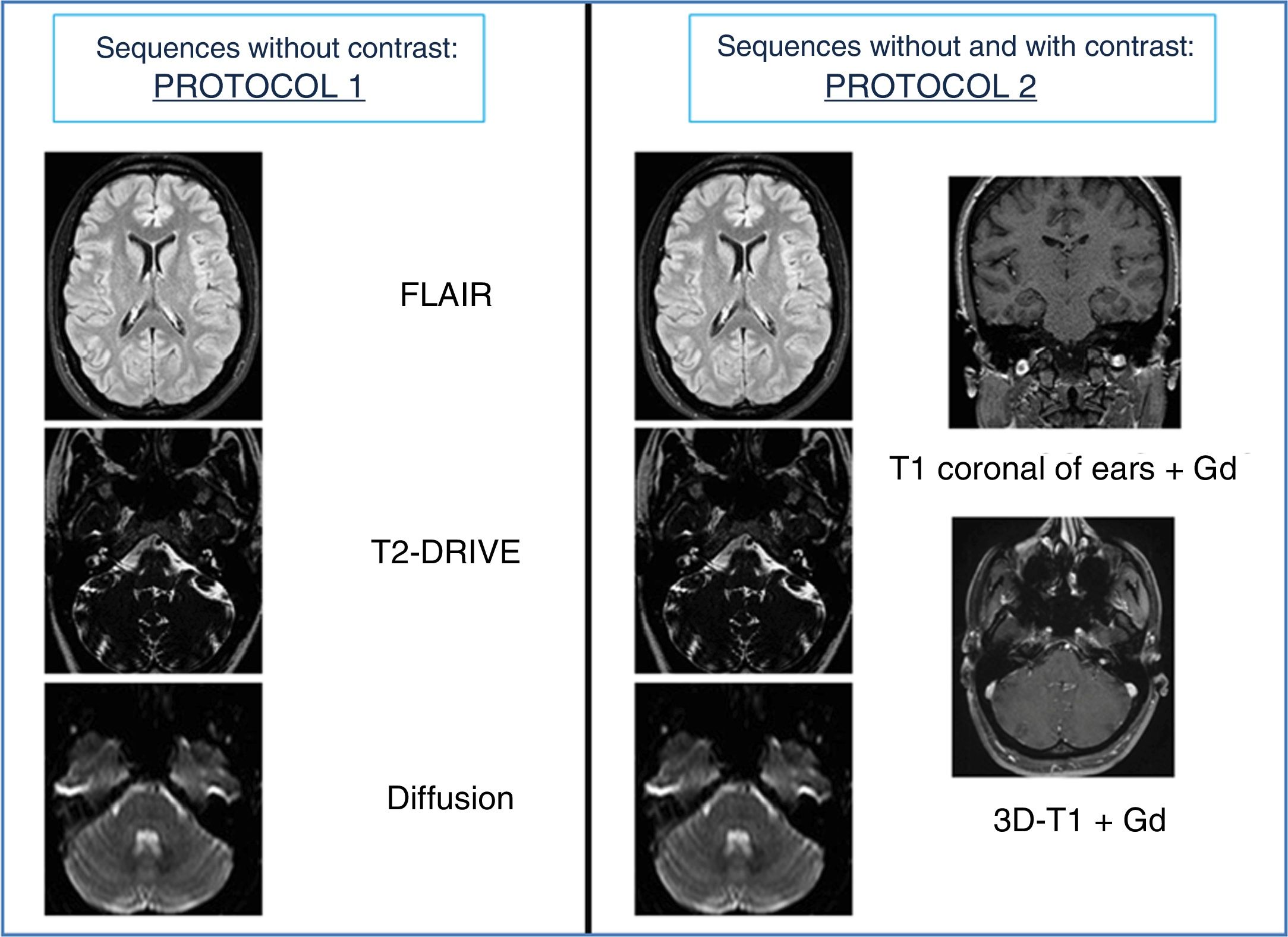
Sequence reading without IVC was called “protocol 1”, and sequences without and with IVC, “protocol 2” (Fig. 2).
All studies were acquired in two MRI scanners, 1.5T: Philips Achieva and Philips Ingenia (Philips® Healthcare, Best, The Netherlands).
The findings were grouped into two categories: findings in the ears and findings outside the ears, which, in turn, were subdivided into cerebral findings and extracerebral findings.
The findings were compared between both protocols and both readers, and an inter-observer correlation was performed.
Statistical analysisThe statistical program with which the data was interpreted was SPSS® (IBM, Chicago, Illinois) version 15.
Categorical variables are described as numbers and percentages.
The χ2 test was conducted to study the association between the reason for the request and the findings in the imaging tests.
Pearson's rho correlation was calculated to assess the discrepancy between both readers and to study the qualitative variables, and the kappa coefficient as a measure of concordance.
The accepted statistical significance threshold (p<0.05) was used.
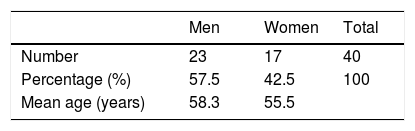
ResultsThe general characteristics of the population are summarized in Table 1. The age range was 36–80, and the median age was 57. There was a slight predominance of the male population (57.5%).
Regarding the reasons for requesting MRI of the ears, hearing loss was the cause of more than half of the requests (52%). Other common reasons for request were: vertigo, control of known schwannoma and tinnitus.
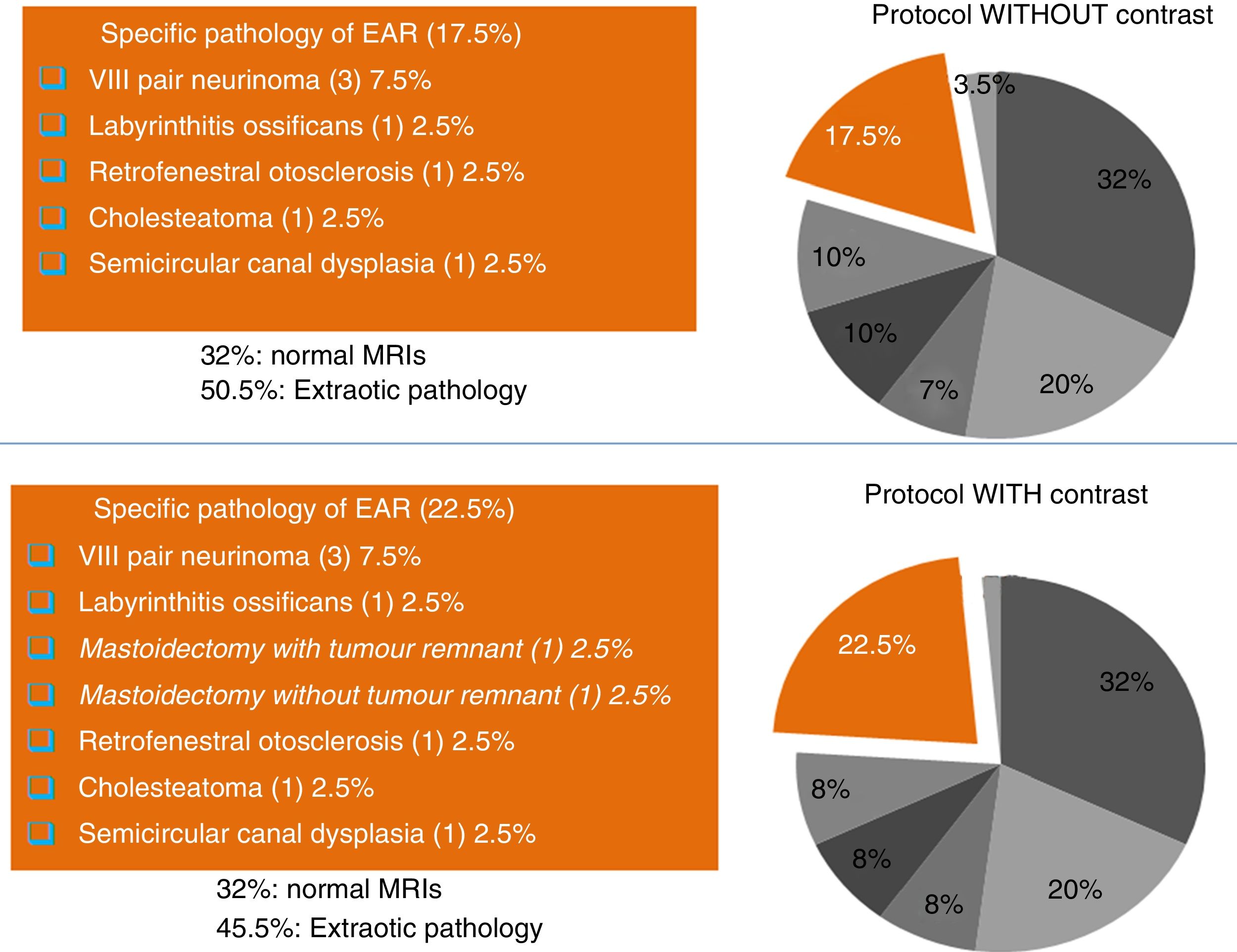
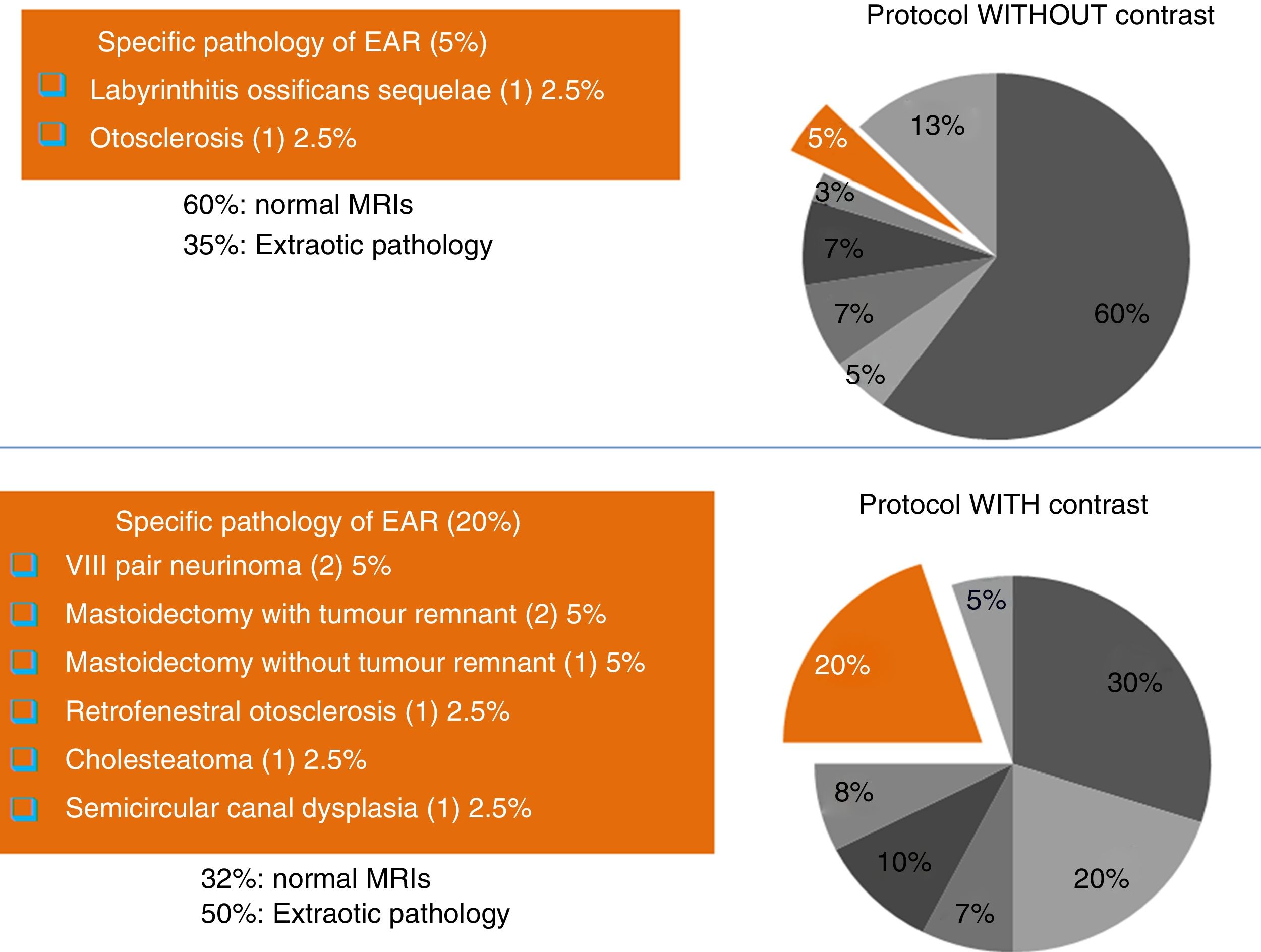
Reading of the protocolsIn the reading made by the neuroradiologist of the studies without IVC, he found no alteration in 32% of the studies, and documented 17.5% of pathology of the ear and 50% of extraotic pathology (Fig. 3). On the other hand, in the reading of the protocols with IVC, there were no substantial changes when comparing the results with the reading of the protocols without IVC. He found 22.5% of otic pathology with the same diagnostic spectrum as the protocol without IVC, plus two post-surgical changes after mastoidectomies, one with tumor remnant and one without tumor remnant.
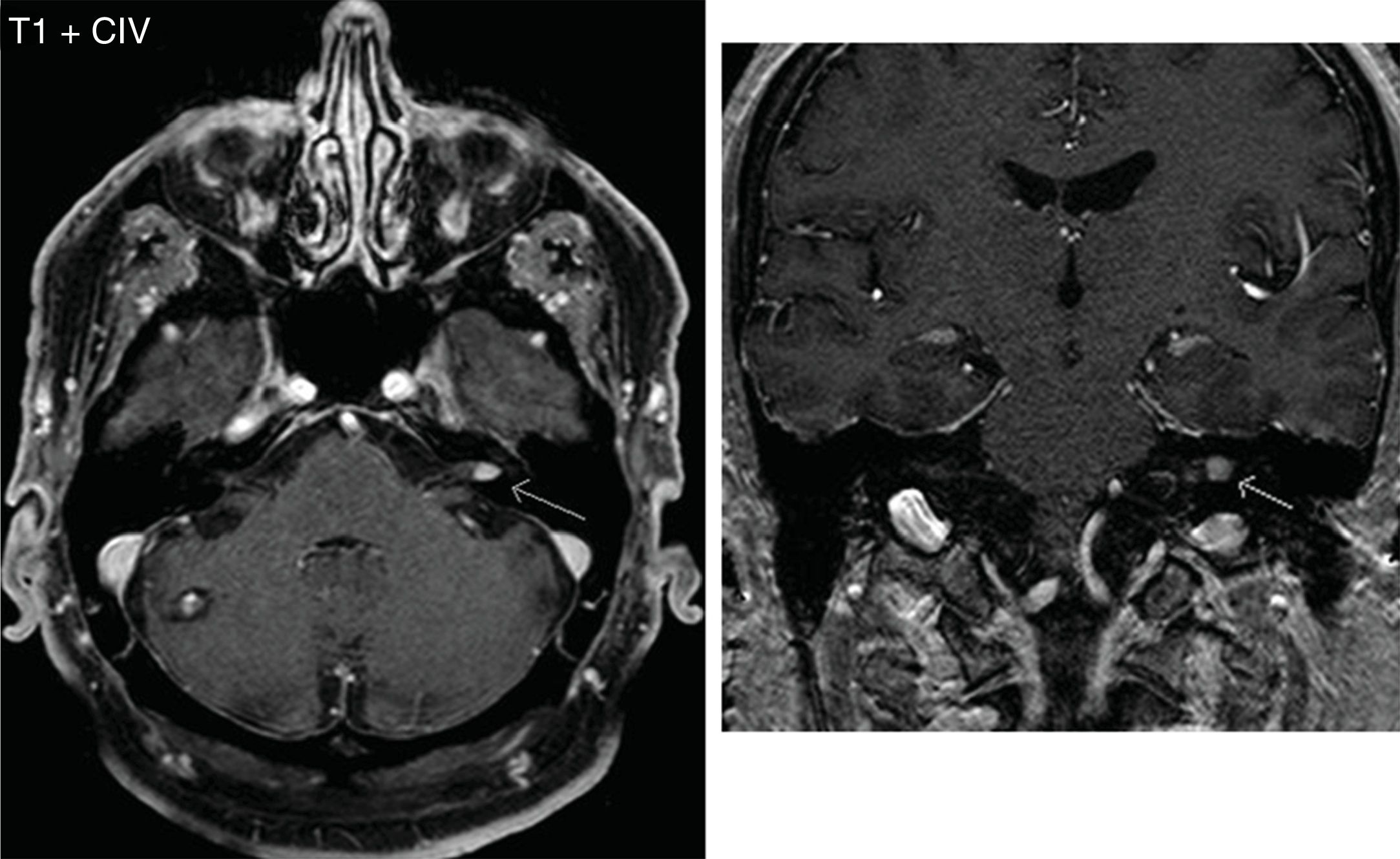
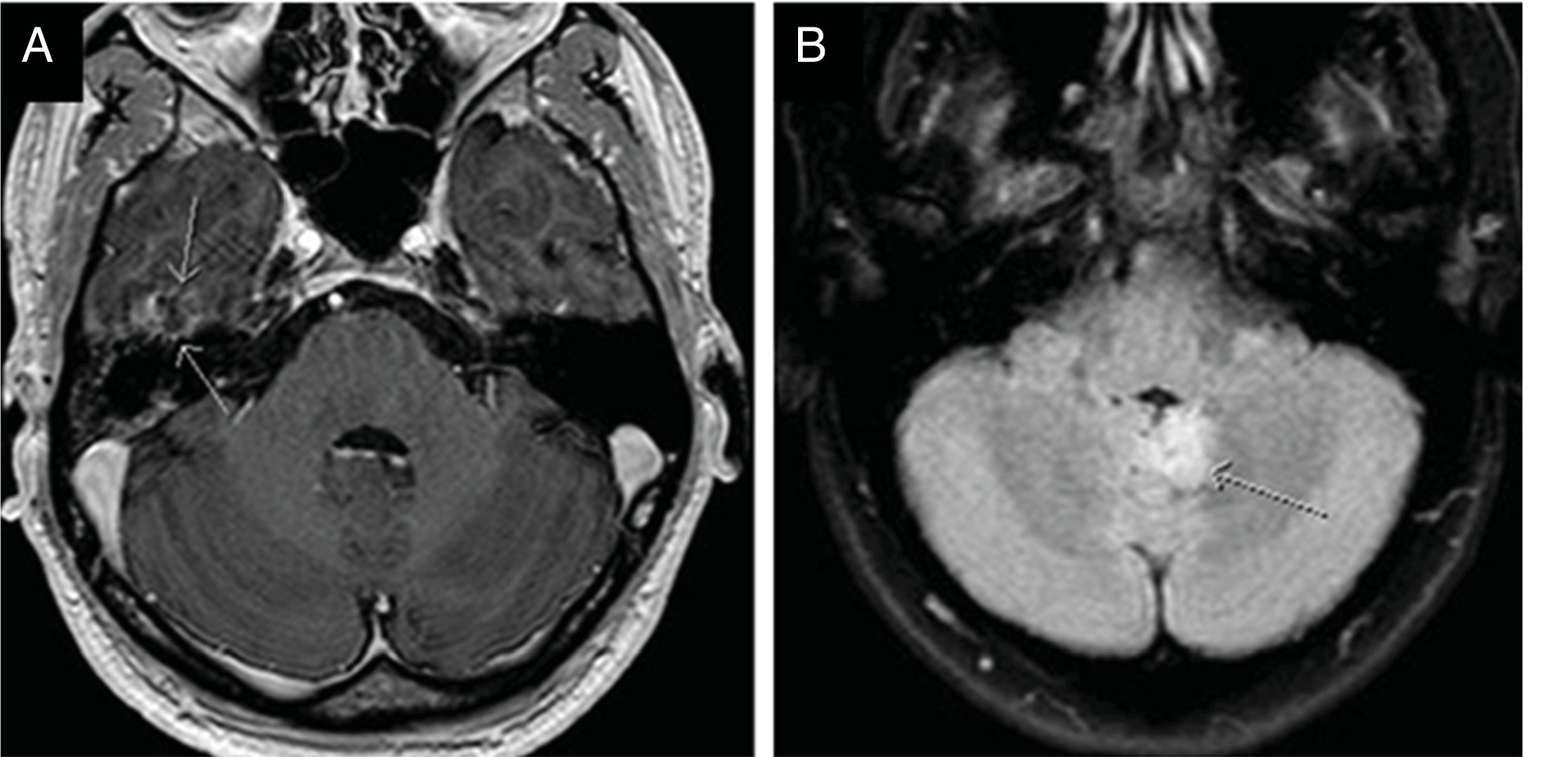
The pathology identified in the ear was schwannomas (Fig. 4), labyrinthitis ossificans, suspicion of retrofenestral otosclerosis, cholesteatoma and semicircular canal dysplasia. Among the extraotic pathology found, in addition to the cavernoma shown in Fig. 4, a low-grade glioma in the cerebellar vermis and a control of a temporobasal brain abscess already practically in resolution stand out (Fig. 5), as well as other alterations of less relevance (ischemic lesions in the brain parenchyma, inflammatory sinusopathy, etc.).
On the other hand, the resident did not find pathology when reading the protocols without IVC in 60% of the studies, and only found otic pathology in 5% of the cases. But when reading the images with IVC, he identified 20% of ear pathology, with diagnoses very similar to those found by the neuroradiologist (Fig. 6). He also found 50% of extraotic findings, and 30% of studies were normal (values also similar to those of the neuroradiologist when using IVC).
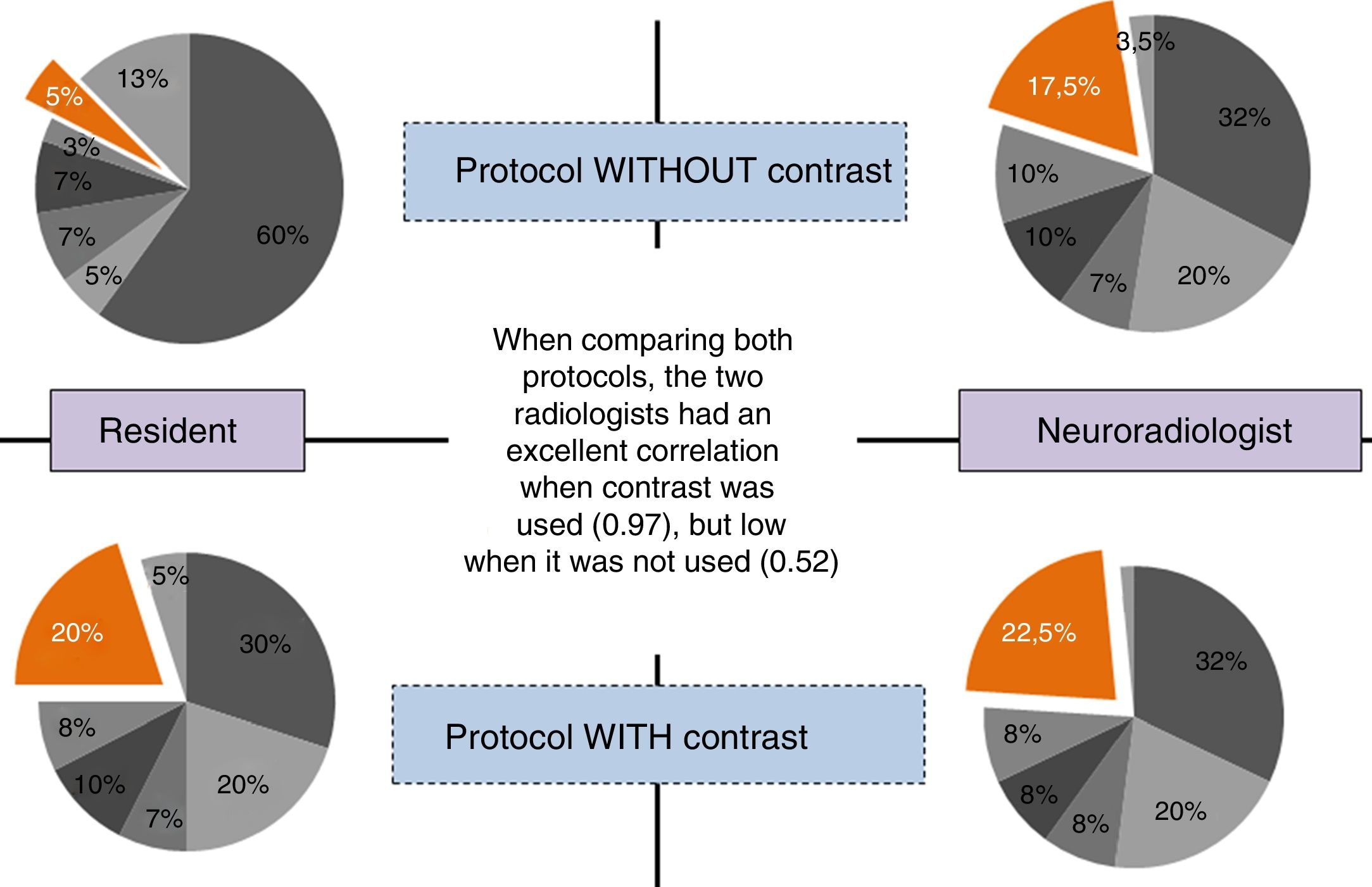
When comparing both protocols (without and with gadolinium) and seeking to coincide in the same diagnosis, the two radiologists had an excellent correlation when assessing the images with IVC (kappa 0.97), and only moderate when baseline sequences were assessed (kappa 0.52) (Fig. 7).
Likewise, when comparing the reason for requesting the study and the findings in the MRI of the ears, there was a correlation. If the patient's symptoms were non-specific (non-specific vertigo, mixed hearing loss, subjective tinnitus, etc.), the most common was to find normal ears. However, if the reason for the request was more specific (control of known schwannoma or objective pulsatile tinnitus), the probability of finding auditory pathology in the studies was higher. These findings were statistically significant, both in protocols without IVC (p=0.004) and in protocols with IVC (p=0.002).
DiscussionWhen reading the protocols without and with gadolinium, no striking differences were found in the results obtained by the neuroradiologist, because in the protocol without IVC a 17.5% specific pathology of ears was found compared to 22.5% after administering IVC. The pathology that was found was very similar, adding only in the protocols with IVC the finding of two patients with mastoidectomies. It is important to note that the FLAIR sequence is acquired with fat suppression and it is difficult to assess bone structures, while in the post-contract sequences one of the 3D sequences is acquired without fat suppression, which allows better evaluation of bone structures and therefore the mastoid. If a protocol is sought to be conducted without contrast, this issue should be taken into account, and a 3D-T1 weighted MRI without fat suppression for mastoid assessment should be considered.
On the other hand, the results obtained by the resident showed striking differences. When reading the protocol without IVC, he only found 5% of specific ear pathology, considering 60% of the studies as “normal”. But after administering IVC, he found a 20% ear-specific pathology, values similar to those found by the neuroradiologist (similar in both the number and the type of pathology).
Of the 40 patients included, 68% consulted for non-specific symptoms, while in 32% the test request had a more precise approach (sudden hearing loss, pulsatile tinnitus, vestibular neuronitis, schwannoma control, otogenic brain abscess and vertigo).
These facts allow us to interpret several things. On the one hand, an expert radiologist finds practically the same findings in protocols without and with gadolinium, except in tumor pathology, where using IVC can help to assess it better. This assertion is consistent with what was found in the scientific literature, both for schwannomas21–24 and for other types of ear tumors.25–28 Despite the evidence, this information should be taken with caution, because even now there are already authors who propose the monitoring of a schwannoma without needing to use IVC, since the cerebrospinal fluid works as a natural contrast medium that makes it possible to distinguish tumor growth.29 That is, even in cases of tumor pathology, the use of IVC is likely to be increasingly restricted.
On the other hand, when the radiologist has less experience, he benefits from using IVC, hence the differences found in the kappa coefficient between them (excellent [0.97] when IVC was used and moderate [0.52] when it was not was used). IVC helps the resident find the ear pathology, while doing the experience curve.
Finally, a correlation was found between the reason for the study request and the findings found in the MRI of the ears with statistically significant values, both in protocols without IVC, and in protocols with IVC. Thus, if there were non-specific symptoms, the most common was to find normal ears. However, if the reason for the request was specific, the probability of finding auditory pathology in the studies was higher.
These results highlight the need to create personalized protocols for each patient and pathology to improve equipment performance and MRI times.
Some limitations are noted. First, the study was done with two radiologists, one of them in the process of training. After analysing the results, this fact, far from being a limitation, was taken as a benefit, as it was what allowed us to demonstrate the impact of IVC when there is no experience. And, second, the same protocol was applied to all patients regardless of symptoms or pathology. No specific MRI protocol was carried out for the study of Ménière's disease, since the available machines did not allow for their acquisition.
It would be ideal to conduct a study using IVC by groups of pathologies (tumor, infectious, traumatic, etc.), in order to know exactly in which pathologies it would be cost-effective to use IVC and in which it would not be cost-effective.
In conclusion, when assessing the MRIs of the ears due to vestibulocochlear symptoms, IVC increases the degree of confidence in the interpretation in a novice radiologist, while in an expert radiologist its use is less relevant. Defining specific protocols for each patient makes it possible to determine who should be administered IVC for a correct assessment of their pathology.
Authorship- 1.
Responsible for the integrity of the study: CASV, ESA, EUP, CJB, MNF and SCE.
- 2.
Study conception: CASV, ESA, EUP, CJB, MNF and SCE.
- 3.
Study design: CASV, ESA, EUP, CJB, MNF and SCE.
- 4.
Data collection: Not applicable.
- 5.
Data analysis and interpretation: Not applicable.
- 6.
Statistical processing: Not applicable.
- 7.
Literature search: CASV, ESA, EUP, CJB, MNF and SCE.
- 8.
Drafting of the article: CASV, ESA, EUP, CJB, MNF and SCE.
- 9.
Critical review of the manuscript with intellectually relevant contributions: CASV, ESA, EUP, CJB, MNF and SCE.
- 10.
Approval of the final version: CASV, ESA, EUP, CJB, MNF and SCE.
The authors declare that they have no conflicts of interest.
Please cite this article as: Sepúlveda Villegas CA, Santos Armentia E, Utrera Pérez E, Jurado Basildo C, Novoa Ferro M, Del Campo Estepar S. Resonancia magnética de conducto auditivo interno: ¿es siempre útil administrar contraste intravenoso?. Radiología. 2020;62:376–383.