To evaluate the safety and efficacy of the embolization of bronchial arteries and nonbronchial systemic arteries with n-butyl-cyanoacrylate (NBCA) in patients with hemoptysis.
MethodsWe analyzed a total of 55 consecutive patients with hemoptysis (14 mild, 31 moderate, and 10 massive) treated with the embolization of bronchial arteries and nonbronchial systemic arteries with n-butyl-cyanoacrylate between November 2013 and January 2020. The main variables analyzed were the rates of technical success, of clinical success, of recurrence, and of complications. Statistics included a descriptive analysis and Kaplan-Meier survival curves.
ResultsEmbolization was a technical success in 55 (100%) and a clinical success in 54 (98.2%). During follow-up (mean, 23.8 months; interquartile range, 9.7–38.2 months), hemoptysis recurred in 5 (9.3%) patients. The nonrecurrence rate was 91.9% one year after the initial procedure and 88.7% two years and four years after the initial procedure. Minor complications related with the procedure occurred in 6 (10.9%); no major complications occurred.
ConclusionsThe embolization of bronchial arteries and nonbronchial systemic arteries with n-butyl-cyanoacrylate is safe and efficacious for controlling hemoptysis, resulting in low recurrence rates.
Evaluar la seguridad y la eficacia de la embolización de arterias bronquiales (AB) y arterias sistémicas no bronquiales (ASNB) con n-butil-cianoacrilato (NBCA) en pacientes con hemoptisis.
MétodosSe han analizado un total de 55 pacientes consecutivos con hemoptisis (14 leves, 31 moderadas y 10 masivas) tratados mediante embolización de arterias bronquiales y arterias sistémicas no bronquiales con n-butil-cianoacrilato entre noviembre de 2013 y enero de 2020. Las variables principales estudiadas son tasa de éxito técnico, tasa de éxito clínico, tasas de recurrencia y complicaciones. Se ha realizado un análisis estadístico descriptivo y un análisis de supervivencia mediante el método de Kaplan-Meier.
ResultadosEn 55 (100%) pacientes se ha realizado la embolización con éxito técnico y en 54 (98,2%), con éxito clínico. Durante el seguimiento (media, 23,8 meses; rango intercuartílico, 9,7–38,2) ha recurrido en 5 de los 54 (9,3%) pacientes. La tasa de no recurrencia al año ha sido del 91,9%, y a los 2 y 4 años, del 88,7% después del procedimiento inicial. Ha habido 6 (10,9%) complicaciones menores relacionadas con el procedimiento y ninguna mayor.
ConclusionesLa embolización de arterias bronquiales y arterias sistémicas no bronquiales con n-butil-cianoacrilato es segura y eficaz para controlar la hemoptisis con tasas de recurrencia bajas.
Haemoptysis is a life-threatening medical emergency with mortality rates greater than 50% in patients not treated correctly.1 In 90% of cases, the origin of haemoptysis resides in the bronchial arteries (BA), while the remaining 10% depends on non-bronchial systemic arteries (NBSA) and pulmonary circulation.2 In all settings, transcatheter embolisation plays a prominent role.1–5
The main embolising materials used for BA and NBSA embolisation are polyvinyl alcohol (PVA) particles and a gelatin sponge.4,6 Traditionally, the use of n-butyl-cyanoacrylate (NBCA) has been avoided in bronchial embolisations for fear of its possible complications, mainly tissue necrosis and unwanted embolisations due to uncontrolled reflux.2,6 However, in the last decade, interest in its use has grown, since it enables rapid, complete embolisations with low recurrence rates.7–12 Regarding the action mechanism, when NBCA comes into contact with blood plasma, it pomlymerises and causes embolisation of the vessel through three mechanisms: formation of thrombotic material, adhesion of NBCA to the intima of the vessel, and damage to the endothelium. NBCA began to be used in neurointerventions in the 1980s for the embolisation of arteriovenous malformations, with Histoacryl (n-butyl-2-cyanoacrylate) (Braun, Germany) being the most widely used cyanoacrylate. At the beginning of the 21st century, a new NBCA entered the market, Glubran 2 (Gem, Italy), which differs from Histoacryl in composition (it adds GEM’s proprietary monomer to n-butyl-2-cyanoacrylate) and in that, unlike Histoacryl, it is expressly authorised for endovascular use. The aim of this study is to retrospectively analyse the safety and efficacy of BA and NBSA embolisation with NBCA in patients with haemoptysis.
MethodsPatientsA retrospective and monocentric study was conducted after carrying out consecutive sampling between November 2013 and January 2020, recruiting 67 patients. The number of cases at our centre during the study period determined the size of the sample.
Patients older than 18 years with haemoptysis treated via BA or NBSA embolisation with NBCA were included in the study. Patients in whom an embolising material other than NBCA was used (6) and those cases whose medical records did not include all the variables analysed (2) were excluded. The final sample analysed was 55 patients.
As this was a retrospective study, authorisation by the ethics committee of our centre was not required. All patients, or their legal representatives, signed the informed consent form.
ProcedureAll patients underwent computed tomography (CT) angiography prior to embolisation to locate the origin of the haemoptysis and assess the cause of the bleeding.13 Bronchoscopy was not routinely performed in all cases.
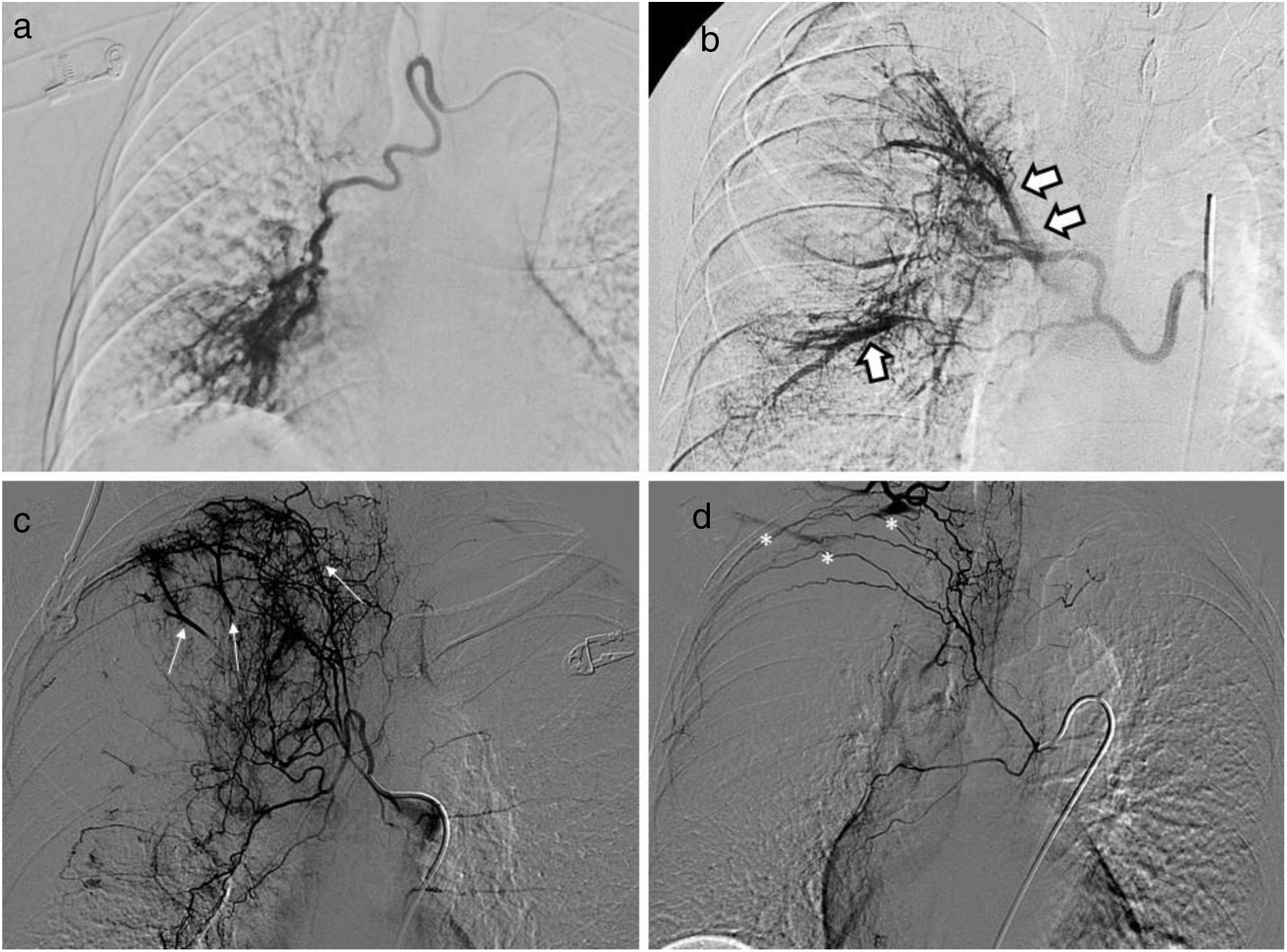
All procedures were performed or supervised by vascular radiologists experienced in endovascular techniques (with between 5 and 30 years of experience). The procedures were carried out via the femoral artery, using a 5 Fr ×11cm introducer. Different 4 Fr angiographic catheters were used to catheterise the BAs and NBSAs: Visceral RLG (Bioteque Corporation, Taiwan), Simmons 1 (Radifocus Glidecath, Terumo, Japan) and Cobra 2 (Radifocus Glidecath, Terumo, Japan). In all cases, supraselective microcatheterisations were performed, using a 2.7 Fr (Progreat, Terumo, Japan) or 2.4 Fr (Direxion, Boston Scientific, Natick, MA) coaxial microcatheter. Angiographic findings considered pathological were: BA or NBSA hypertrophy (>3mm), tortuous Bas or NBSAs, aneurysms, parenchymal hypervascularisation, BA- and NBSA-pulmonary artery shunts, BA- and NBSA-pulmonary vein shunts, and contrast extravasation (Fig. 1).2,14 All pathological BAs and NBSAs were embolised, paying special attention to findings that could contraindicate intervention, such as filling of the anterior spinal artery or BA-systemic artery shunts.4,15 For embolisation, a dilution of NBCA (Histoacryl [Braun, Germany] or Glubran 2 [Gem, Italy]) with Lipiodol (Guerbert, France) was used in a ratio from 1: 2 to 1: 5, according to the radiologist's criteria. To avoid polymerisation and blockage of the microcatheter, 5% dextrose was used. After the corresponding embolisation, follow-up serial angiography studies were performed. As per our standard practice, not all contralateral BAs and NBSAs were explored, nor was the pulmonary artery.
Pathological angiographic findings: a) Hypertrophic (>3mm) and tortuous right bronchial artery with parenchymal hypervascularisation. b) Hypertrophic right bronchial artery-pulmonary vein shunt (arrows). c) Intercostobronchial trunk and hypertrophic branches with pulmonary artery shunt (thin white arrows) and parenchymal hypervascularisation. d) Right intercostobronchial trunk and branches with normal calibre with right subclavian artery shunt (asterisks).gr1
Demographic variables (age and sex), variables related to haemoptysis, details of the procedure, and variables related to follow-up were analysed after reviewing the digital medical records and the images and reports of the procedure.
Regarding haemoptysis, the degree and cause were analysed. There is no consensus on the different degrees of haemoptysis based on the volume and frequency of episodes.1,3–5 In this study, patients were classified into three categories: mild haemoptysis if it was less than 100ml/day, moderate haemoptysis if it was between 100 and 300ml/day, and massive haemoptysis if it exceeded 300ml/day or haemoptysis of any volume that led to a fall in haemoglobin greater than 1g/dl, a fall in haematocrit greater than 5%, respiratory failure or hypotension with a fall in systolic pressure below 90mmHg.4
Regarding the technique, the number and type of embolised arteries (BAs or NBSAs) were assessed. Technical success was defined as complete embolisation of all treated arteries, and clinical success as cessation of haemoptysis within 24h after embolisation.7 Major complications were classified as those that prolonged hospital stay, required an advanced level of care, or led to permanent sequelae or death.16 All other complications were classified as minor.
After hospital discharge, the patients were periodically evaluated as outpatients to monitor the underlying cause and the haemoptysis itself. If haemoptysis recurred, patients were told to go to the emergency department immediately. Recurrence was defined as those cases with a new episode of haemoptysis that required bronchoscopy, repeat embolisation or any invasive intervention.17 Patients who underwent a second embolisation were classified according to the cause of recurrence: re-permeabilisation of the previously treated artery, incomplete previous embolisation due to failure to identify the culprit vessel, or creation of new collateral circulation.10 Patients were followed-up time until the last hospital visit or death.
Statistical analysisQuantitative variables have been expressed as mean and interquartile range (IQR). Qualitative variables have been expressed as the number of patients (n) and the percentage.
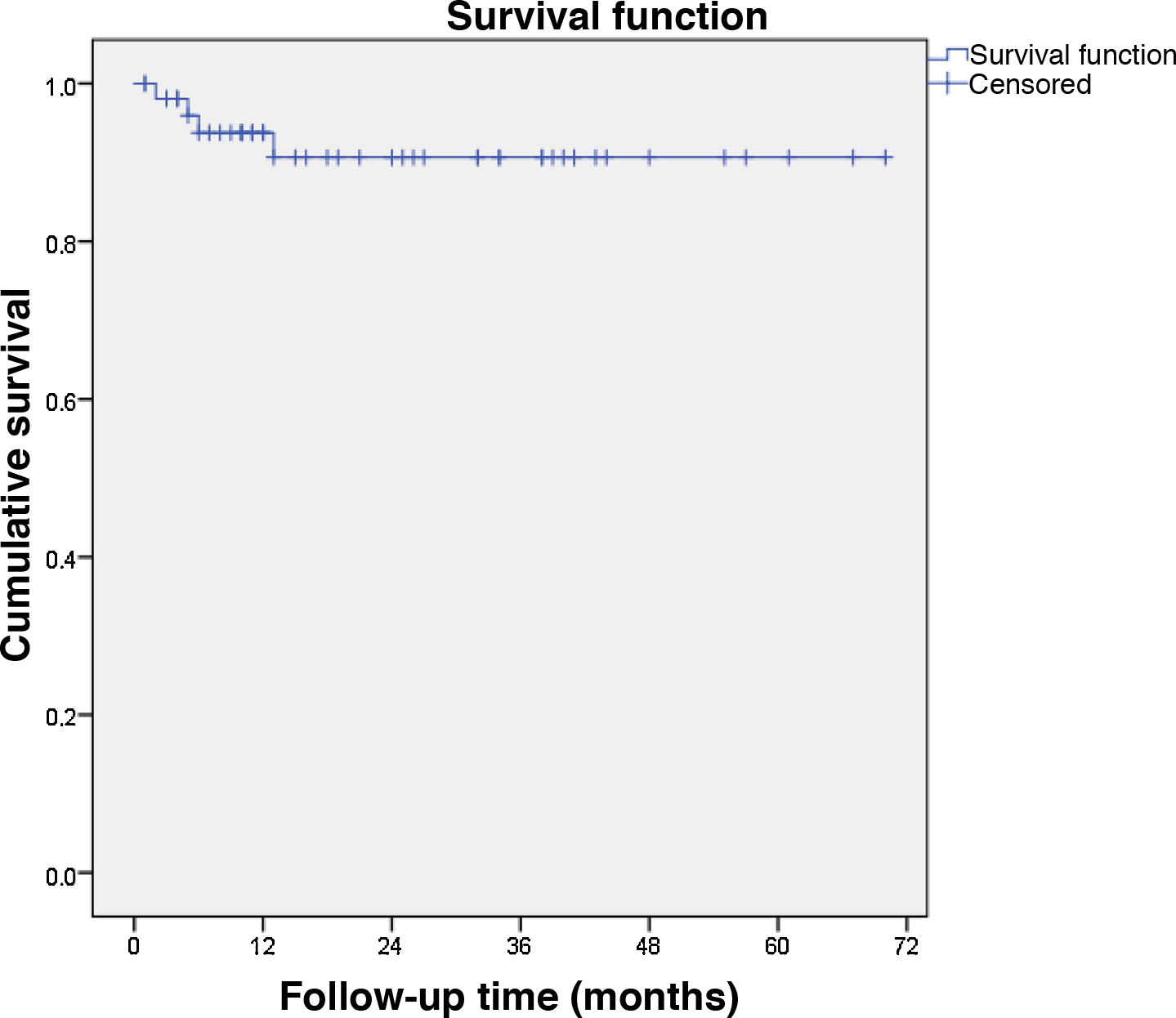
The haemoptysis recurrence rate was estimated according to the Kaplan-Meier method.
The SPSS 23 package for Windows was used to carry out this analysis.
ResultsThe baseline characteristics of the patients are shown in Table 1.
Baseline characteristics of the 55 patients treated with embolisation of bronchial arteries and non-bronchial systemic arteries with n-butyl cyanoacrylate.
| Variables | Value |
|---|---|
| Gender | |
| Male n (%) | 35 (63.6) |
| Female n (%) | 20 (36.4) |
| Age | |
| Mean (IQR) | 63 (53–77) |
| Degree of haemoptysis | |
| <100ml/day n (%) | 14 (25.5) |
| 100-300ml/day n (%) | 31 (56.4) |
| Massive n (%) | 10 (18.2) |
| Cause of haemoptysis | |
| Bronchiectasis n (%) | 20 (36.4) |
| Cryptogenic n (%) | 17 (30.9) |
| Lung cancer n (%) | 6 (10.9) |
| Non-TB infection n (%) | 5 (9.1) |
| TB sequelae n (%) | 3 (5.5) |
| Active TB n (%) | 1 (1.8) |
| Aspergilloma n (%) | 1 (1.8) |
| Other n (%) | 2 (3.6) |
| Number of affected lobes | |
| Mean (IQR) | 1.5 (1-2) |
| Location | |
| RUL n (%) | 24 (43.6) |
| ML n (%) | 13 (23.6) |
| RLL n (%) | 17 (30.9) |
| LUL (not lingula) n (%) | 14 (25.5) |
| LUL (lingula) n (%) | 9 (16.4) |
| LLL n (%) | 12 (21.8) |
IQR: interquartile range; LLL: left lower lobe; LUL: left upper lobe; ML: middle lobe; RLL: right lower lobe; RUL: right upper lobe; n: number of patients; TB: tuberculosis.
The details and results of embolisations are summarised in Table 2. A total of 95 arteries were embolised, 76 BAs (52 right, 24 left) and 19 NBSAs (16 intercostal arteries, 3 branches of the internal mammary artery) in 55 patients. All the procedures were technically successful. In all cases, immediate control of haemoptysis was achieved, except in one patient with lung cancer, in whom, despite successful embolisation, haemoptysis did not cease in the first 24h. There were no major complications or mortality related to the embolisations. Six minor complications were recorded: 2 self-limiting post-embolisation syndromes (3.6%), 2 BA dissections without repercussions (3.6%), 1 transient ischaemic attack lasting a few minutes that resolved spontaneously (1.8%) and 1 mild adverse reaction to iodinated contrast (1.8%).
Details and results of embolisations.
| Variables | Value |
|---|---|
| Embolised arteries | |
| Mean (IQR) | 1.7 (1–2) |
| Embolised right bronchial arteries | |
| Mean (IQR) | 1 (1–1) |
| Embolised left bronchial arteries | |
| Mean (IQR) | 0.4 (0–1) |
| Embolised non-bronchial systemic arteries | |
| Mean (IQR) | 0.3 (0–1) |
| Angiographic findings | |
| Arterial hypertrophy n (%) | 52 (94.5) |
| Arterial tortuosity n (%) | 46 (83.6) |
| Parenchymal hypervascularisation, n (%) | 41 (74.5) |
| Pulmonary artery-to-artery shunts n (%) | 5 (9.1) |
| Pulmonary artery-to-vein shunts n (%) | 4 (7.3) |
| Contrast extravasation n (%) | 1 (1.8) |
| Technical success | |
| n (%) | 55 (100) |
| Clinical success | |
| n (%) | 54 (98.2) |
| Complications | |
| Minors n (%) | 6 (10.9) |
| Adults n (%) | 0 (0) |
IQR: interquartile range; n: number of patients.
The mean follow-up time was 23.8 months (IQR: 9.7–38.2). Of the 54 patients in whom embolisation was clinically successful, 5 (9.3%) presented recurrence, with no recurrence-related deaths: 2 early (<3 months) and 3 late (>3 months). The non-recurrence rate at 6 months and one year was 91.9%; and 88.7% at 2, 3 and 4 years (Fig. 2). Regarding the degree of haemoptysis, 3/10 (30%) of mild haemoptysis, 2/29 (6.9%) of moderate haemoptysis, and 0/10 (0%) of massive haemoptysis recurred. The aetiology of recurrent haemoptysis was bronchiectasis (1/20, 5%) cryptogenic (2/17, 11.8%), lung cancer (1/5, 20%) and aspergillosis (1/1, 100%).
Of the 5 patients with recurrence, arteriography was repeated in 4 cases, and 1 underwent surgery. One of the patients in whom the arteriography was repeated was not treated, since no pathological angiographic findings were observed. The other 3 patients were embolised, since 2 (3.7%) presented non-embolised pathological vessels in the first procedure and 1 (1.8%) presented partial recanalisation of the embolised vessel. In no case was neoangiogenesis observed.
DiscussionEfficacy and recurrenceThis monocentric study shows that BA and NBSA embolisation with NBCA can be performed with high clinical success rates (98.2%) and with low recurrence rates (8.1% at 6 months and at 1year; 11.3% at 2, 3 and 4 years). These results are in line with previous studies, which analysed NBCA as a material for bronchial embolisations.7–11 The clinical success rates of these studies range between 96.5% and 100%, and recurrence rates range between 4% and 20%.
PVA particles are the most widely used material for bronchial embolisations.4 However, as Yoo et al. and Razavi and Murphy pointed out, PVA particles have several drawbacks: visualisation is not optimal, procedures are long, they can be associated with incomplete embolisations, and there is a high rate of recanalisation of embolised vessels.7,10 Clinical success rates for embolisations performed with PVA particles range from 85% to 99%, while recurrence rates range from 28% to 37%.8,10,18–20
Different mechanisms involved in recurrences have been established. Early recurrences (<3 months) are usually secondary to inadequate or incomplete embolisation due to the failure to search for all the vessels involved or the inability to embolise all the arteries in the first session.4 Late recurrences (>3 months) are attributed to recanalisation of previously embolised arteries or neoangiogenesis due to progression of the underlying disease.18,21,22 This mechanism is an inherent limitation of embolisation, as it does not act on the underlying cause, and cannot be avoided. Incomplete or inadequate embolisations can be avoided by performing the procedure correctly and systematically, and vascular recanalisations could also be minimised by choosing the right embolising material. Woo et al. report a significant difference in terms of recanalisation of the embolised vessel when comparing NBCA (1.8%) with PVA particles (21.5%),8 which would explain the unequal rates of recurrence in embolisations with NBCA and with PVA particles. In our experience, the main mechanism of recurrence has been the presence of pathological vessels not treated in the first procedure. This could be due to the fact that the embolisations carried out were not sufficiently distal, allowing the underlying cause to promote vascularisation from these vessels. However, it could also be secondary to a satisfaction bias on the part of the operator who, after identifying the main vessel involved, does not look for other pathological vessels.
Safety and complicationsIn our study, the rate of major complications was 0% and that of minor complications was 10.9%. The severity of the possible complications associated with bronchial embolisations with NBCA is the main argument against this technique. The most feared complications are tissue necrosis and complications derived from unwanted and inadvertent embolisations, either due to uncontrolled reflux or through shunts.2,6,10 However, recently published studies show that it is a safe material with a major complication rate of 0%.7–11
Girard et al. reported in 1990 a case of bronchial stenosis secondary to ischaemia after a bronchial embolisation with NBCA,23 although no new cases with ischaemic complications have been published.7–11 Ikoma et al. histologically evaluated the lung of a patient who had undergone a bronchial embolisation with NBCA and showed that there was no ischaemic damage to the bronchial walls or the lung parenchyma.24 Tanaka et al. assessed the efficacy and safety of NBCA in bronchial embolisations with pigs, observing no damage to the bronchial walls or the lung parenchyma.25
To avoid unwanted embolisations, it is recommended to perform supraselective catheterisations4 and pay special attention to possible shunts. It is also useful to adjust the concentrations of NBCA and Lipiodol (Guerbert, France) according to the characteristics of the vessel to be embolised.7 In large vessels with rapid blood flow and those associated with major bronchopulmonary shunts, a 1: 2 or 1: 3 ratio can be used for faster polymerisation. In smaller arteries with lower flow, 1: 4 or 1: 5 dilutions can be used for slower polymerisation.
BA and NBSA embolisation with NBCA should only be performed by experienced radiologists, as it has a slow learning curve. Interventionist must become familiar with its use in territories with a low risk of complications before using it in such demanding embolisations, in which both proximal, but primarily distal, embolisation is required. The success of the embolisation will depend on the ability of the interventionist to choose the best NBCA-to-Lipiodol (Guerbert, France) ratio, injection speed, and volume for the calibre and flow of the vessel to be treated.
Regarding the different presentations of NBCA, the two types most used in interventional vascular radiology are Histoacryl (Braun, Germany) and Glubran 2 (Gem, Italy). When considering which one to choose, it should be borne in mind that Glubran 2, unlike Histoacryl, is authorised for endovascular use, although Histoacryl is more widely used and has been evaluated in numerous scientific studies. Meanwhile, a new presentation of cyanoacrylate, Magic Glue (Balt International, France), which consists of n-hexyl-cyanoacrylate monomers, has recently come onto the market. This new formulation shows the same short and long term occlusive efficacy as NBCA, but may have certain advantages, such as reduced adhesive strength to the catheter and longer time of injection.
LimitationsThis study has several limitations. First, it is a retrospective study and lacks data that would be useful to analyse, such as follow-up bronchoscopy after embolisation, duration and radiation of the procedure. Second, there is no control group treated with another embolising material with which to compare NBCA and show its possible advantages and disadvantages. Third, the sample is heterogeneous (various degrees of haemoptysis, different causes, and use of two types of NBCA). This, together with the methodological heterogeneity of the published scientific literature, calls for caution when interpreting and generalising our results.
ConclusionBA and NBSA embolisation with NBCA is a safe and effective treatment to control haemoptysis. Our study shows that bronchial embolisations with NBCA have a high clinical success rate, low recurrence rates and an absence of major complications.
Authorship- 1
Responsible for the integrity of the study: PBGJ.
- 2
Study concept: PBGJ, MEPM, SLG, JJEH.
- 3
Study design: PBGJ, MEPM, SLG, JJEH.
- 4
Data collection: PBGJ, MEPM, MEC, JGR.
- 5
Data analysis and interpretation: PBGJ, MEPM, SLG, MEC, JGR, JJEH.
- 6
Statistical processing: PBGJ
- 7
Bibliographic search: PBGJ, MEPM, SLG, MEC, JGR, JJEH.
- 8
Drafting of the article: PBGJ, MEPM.
- 9
Critical review of the manuscript with intellectually relevant contributions: MEPM, SLG, MEC, JGR, JJEH.
- 10
Approval of the final version: PBGJ, MEPM, SLG, MEC, JGR, JJEH.
The authors declare that they have no conflicts of interest.
In memory of Dr. Luis J Zurera Tendero, our mentor and colleague, a precursor of bronchial embolisation with n-butyl-cyanoacrylate at our hospital.