Prosthetic valve obstruction is a rare but potentially lethal complication. The most frequent causes are thrombus and pannus formation, in the absence of infectious data. Diagnosis is not always easy using cardiac CT scanning and in 46%–85% of cases thrombus and pannus coexist, complicating the diagnosis. A rapid diagnosis is essential to avoid a fatal outcome of this pathology whose mortality, despite correct treatment, is high.
La obstrucción de una válvula protésica es una complicación rara pero que puede ser letal. Las causas más frecuentes son la formación de trombos y pannus, en ausencia de datos infecciosos. El diagnóstico no siempre es sencillo recurriendo a la realización de tomografía computarizada (TC) cardiaca, y en el 46–85% de los casos coexisten trombo y pannus, por lo que el diagnóstico se complica. Un diagnóstico rápido es esencial para evitar un desenlace fatal de esta patología, cuya mortalidad, a pesar de un tratamiento correcto, es elevada.
The incidence of prosthetic heart valve obstruction is rare (0.1%–4% per year).1 In the absence of infectious data, the most frequent cause is the formation of thrombus (0.3%–8%), being more prevalent in the first postoperative year,2 and of pannus3 (0.2%–4.5%). The cause of thrombus formation is usually inadequate anticoagulation. Pannus is a chronic non-immunological inflammatory reaction that grows in the periannular region of cardiac prostheses. Overgrowth of this tissue can lead to prosthetic dysfunction and thrombus formation.4 Diagnosis requires imaging techniques for morphological and functional assessment of the prosthesis in multiple planes, with transthoracic echocardiography (TTE) being the technique of choice. Transoesophageal echocardiogram (TOE) is recommended in case of suspected/confirmed dysfunction. Fluoroscopy and cardiac CT with electrocardiogram (ECG) synchronisation are complementary techniques. In addition, CT scans can be used to assess for other complications.
The correct diagnosis is crucial for the therapeutic approach.
Case reportThis was a 58-year-old patient with a mechanical mitral prosthesis and a history of controlled atrial fibrillation with optimal anticoagulant treatment. The last echocardiogram, performed one year ago, showed a preserved left ventricular ejection fraction (LVEF) without significant mitral prosthesis dysfunction.
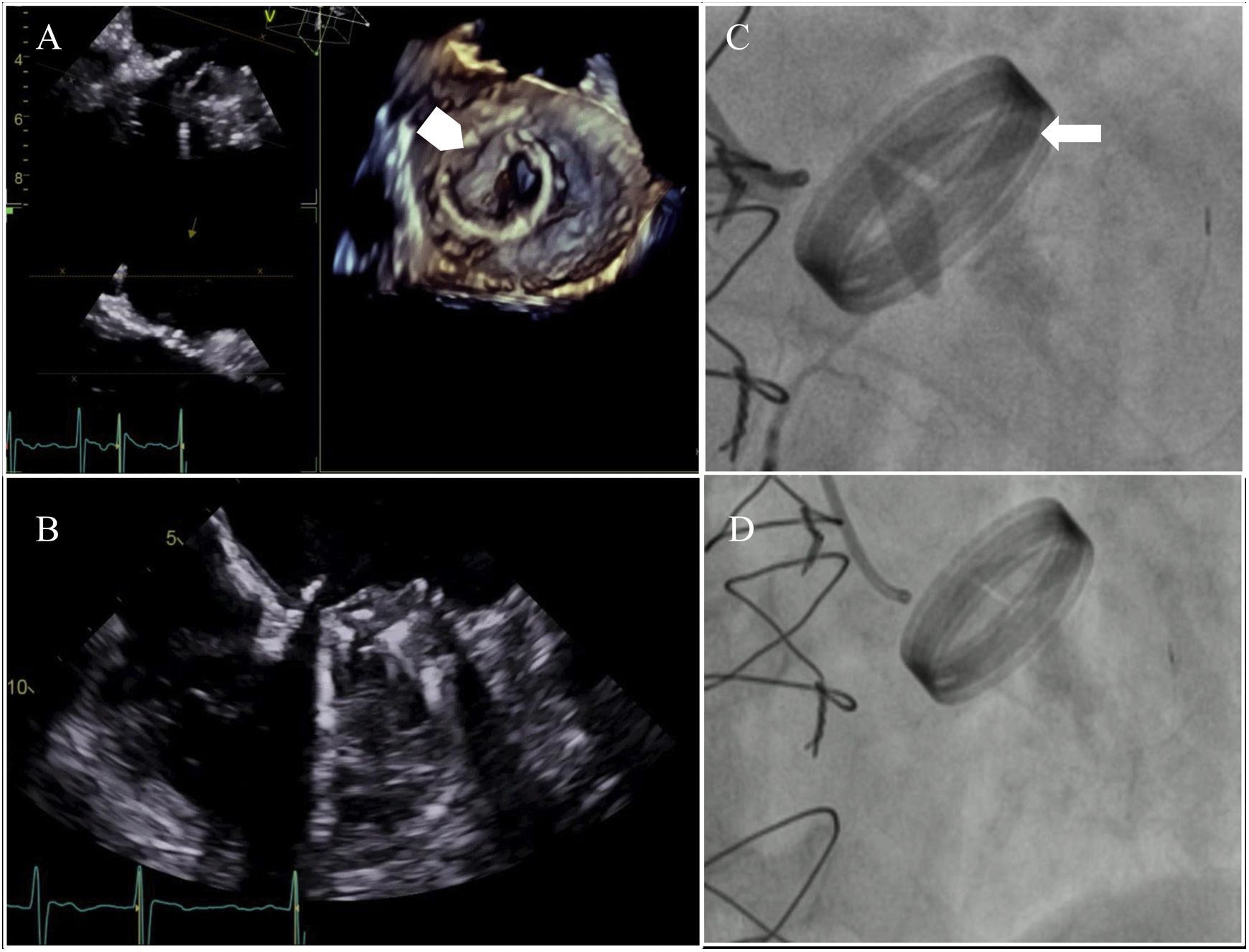
The patient consulted his doctor for dyspnoea on exertion and an echocardiogram was performed, which revealed an isoechoic lesion with the myocardium on the anterolateral disc of the mechanical mitral prosthesis, leading to dysfunction due to obstruction in the closed position of one of the discs (Fig. 1), a finding that was confirmed by fluoroscopy (Fig. 1).
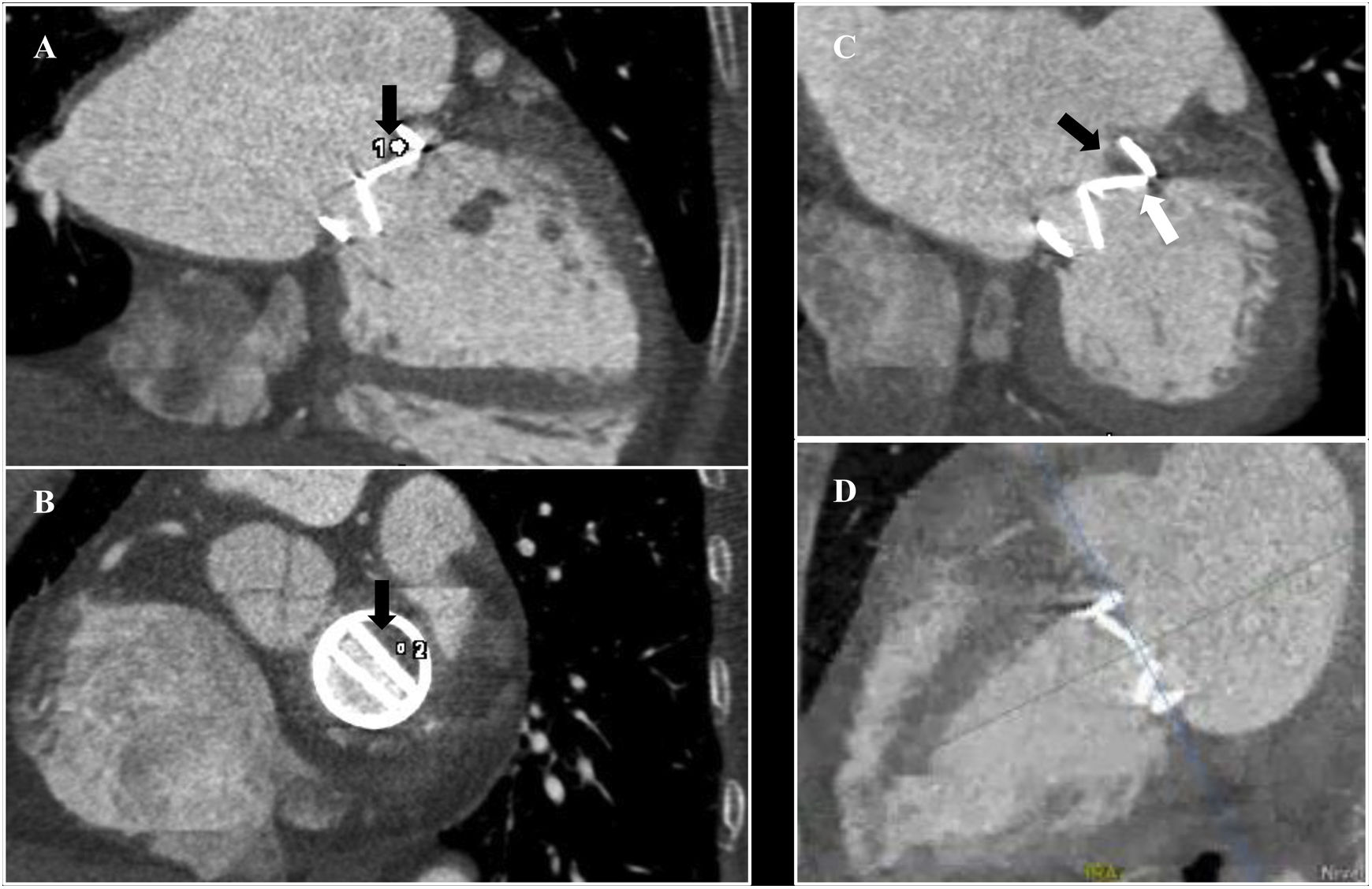
These imaging techniques failed to distinguish between thrombus and pannus, so cardiac CT was performed with ECG synchronisation (retrospective acquisition), intravenous contrast (dose calculated by computer software), 60%–70% R–R interval reconstructions (due to his heart rate) and multiplanar reconstructions. A hypodense lesion was observed on the atrial aspect of the anterolateral disc, non-calcified, with small areas with 90 Hounsfield units (HU) and others with 180 HU. This lesion led to an obstruction in the closed position of the disc (Fig. 2). Due to the presence of areas with 90 HU measured at different phases of the cardiac cycle, the characteristics of the lesion, and taking into account the possible low attenuation and blooming artifacts produced by the mechanical prosthesis, thrombus was the most likely diagnosis.
Hypodense lesion (black arrow) on the atrial side of the anterolateral disc resulting in obstruction of the disc in the closed position. Cardiac CT with ECG synchronisation, retrospective acquisition. (A) Two-chamber long axis view. ROI 1: 90 HU. (B) Mitral valve plane. ROI 2: 180 HU. (C) Two-chamber long axis view in diastole. Disc obstructed in closed position (white arrow). (D) Video. Two-chamber long-axis view in diastole showing the obstruction of the anterolateral disc in closed position.
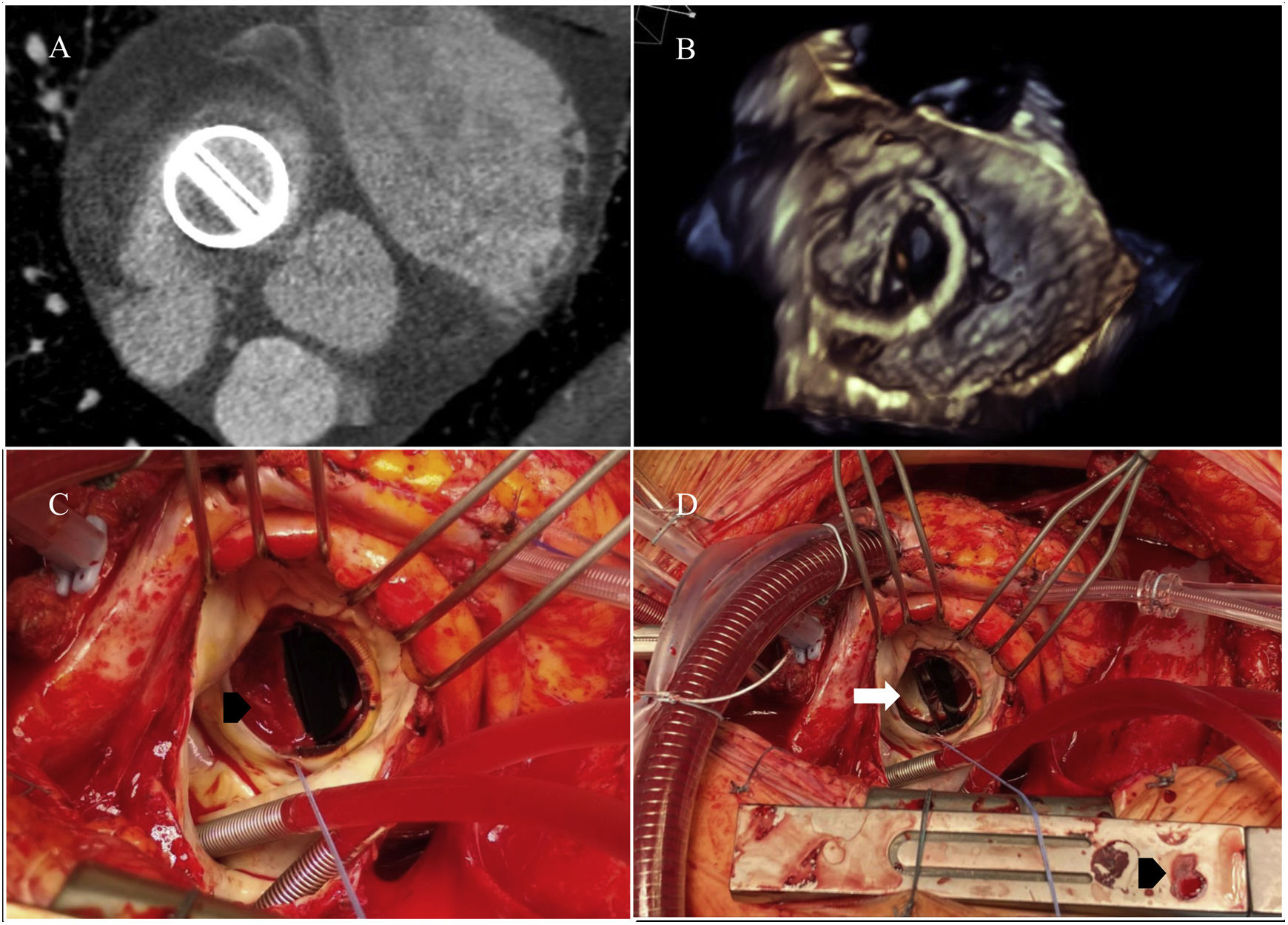
Finally, cardiac surgery revealed the presence of pannus obstructing the disc and a fresh thrombus on top of it (Fig. 3).
Pannus over the atrial side of the anterolateral disc of the mechanical mitral prosthesis with thrombus on top of the pannus. Mitral valve plane. (A) Cardiac CT. (B) 3D transoesophageal echocardiography. (C) View of the atrial side of the mitral plane in surgery with thrombus (black arrowhead) over pannus in the obstructed anterolateral disc in the closed position. (D) Removal of thrombus (black arrowhead) and view of the pannus (white arrow) over the anterolateral disc.
The diagnosis of mechanical prosthetic valve obstruction is made by transthoracic/transoesophageal echocardiography and fluoroscopy. The indication for cardiac CT is the differential diagnosis between thrombus and pannus, being especially useful in patients with double left mechanical prostheses due to the acoustic shadow they cause5 on echocardiography.
Prosthetic valve thrombosis can be obstructive or non-obstructive, with the latter being more common.6 Prosthetic thrombosis is more prevalent in mechanical valves than in biological valves, on the right side more than on the left, and in the mitral position more than in the aortic.7
On CT, a thrombus is visualised as a hypodense supra- or infravalvular lesion anchored to the disc or valve leaflets. It measures less than 90 HU7 and is usually irregular in morphology, mobile and does not calcify.2
A pannus is visualised as a hypodense lesion with a semicircular configuration around the valvular annulus8 and over the disc. It measures more than 145 HU and may calcify. It is equally common in mechanical and biological valves and three times more common in the mitral position. It can appear within one to 12 months of surgery (early pannus) and, more frequently, after five years.
To obtain adequate HU measurements, regions of interest (ROI) must be small in size and reproduced at various stages of the cardiac cycle, discarding measurements of areas that may suffer from heartbeat artifacts, as well as low-density and blooming artifacts caused by the mechanical prosthesis. An adequate acquisition technique must be performed, correctly opacifying the left cavities.
The difficulty in this case lies in the coexistence of thrombus and pannus on the atrial side of the disc, which causes the existence of areas with 90 HU and areas with more than 145 HU, with 145 HU considered as the cut-off point according to some authors. In addition, due to the ECG-based tube current modulation acquisition technique (maximum radiation dose is delivered in certain phases of the cardiac cycle and the dose is reduced to 4% or 20% of the nominal tube dose in the rest of the R–R interval), motion and prosthesis artifacts are more conspicuous.
Regarding patient management, in case of obstructive thrombosis in critically ill patients without contraindications for surgery, urgent valve replacement is recommended. Surgery should be considered for thrombi larger than 10 mm that do not lead to valvular obstruction and present embolic complications and/or do not disappear despite optimal anticoagulation therapy.
Fibrinolysis is advised if surgery is not indicated, or if treatment of right prosthetic valve thrombosis is high risk, but it carries a risk of bleeding and thromboembolism.9
Both in the case of pannus and in the case of coexisting thrombus, valve replacement is indicated.
In our case, the prosthetic dysfunction was caused by the pannus, on which a thrombus subsequently formed. The presence of pannus and other factors, such as turbulent flow, recirculation zones and transprosthetic flow conditions, favour thrombus formation.
We have not found in the literature a CT description of the coexistence of pannus and thrombus on the same side of the prosthetic disc. Cases of thrombus on the atrial side and pannus on the ventricular side of the prosthesis have been reported,10 which facilitates diagnosis. Cases of early thrombosis followed by pannus dysfunction (on different sides of the disc and not coexisting) have also been reported. According to the authors, this supports the hypothesis that a thrombus may precede pannus formation.4 Therefore, we assume that the fact of finding areas with such disparate HU measurements (≤90 and >145 HU) should lead us to suspect the coexistence of both conditions.
In conclusion, the diagnosis of mechanical prosthetic valve obstruction in the absence of infection requires a rapid differential diagnosis between thrombus and pannus, due to their high mortality and different therapeutic management. The coexistence of the two conditions further complicates the diagnosis, so it is necessary to understand the characteristics associated with each of them for a better diagnostic approach.
FundingThe authors declare that they have not received any funding to carry out this study.
Author’s contributions- •
Responsible for the integrity of the study: AIBA.
- •
Study conception: AIBA, RYLS.
- •
Study design: AIBA, RYLS, ERG.
- •
Data acquisition: AIBA, ERG, RAC.
- •
Data analysis and interpretation: RYLS, ERG.
- •
Statistical processing: AIBA, ERG, RAC
- •
Literature search: RYLS, ERG.
- •
Drafting of the manuscript: AIBA, RYLS.
- •
Critical review of the manuscript with intellectually relevant contributions: RYLS, ERG, RAC.
- •
Approval of the final version: AIBA, RYLS, ERG, RAC.
The authors declare that they have no conflicts of interest.