To determine the prevalence of pseudocavitation in lung tumors and whether its presence makes it possible to predict the diagnosis of adenocarcinoma with lepidic growth.
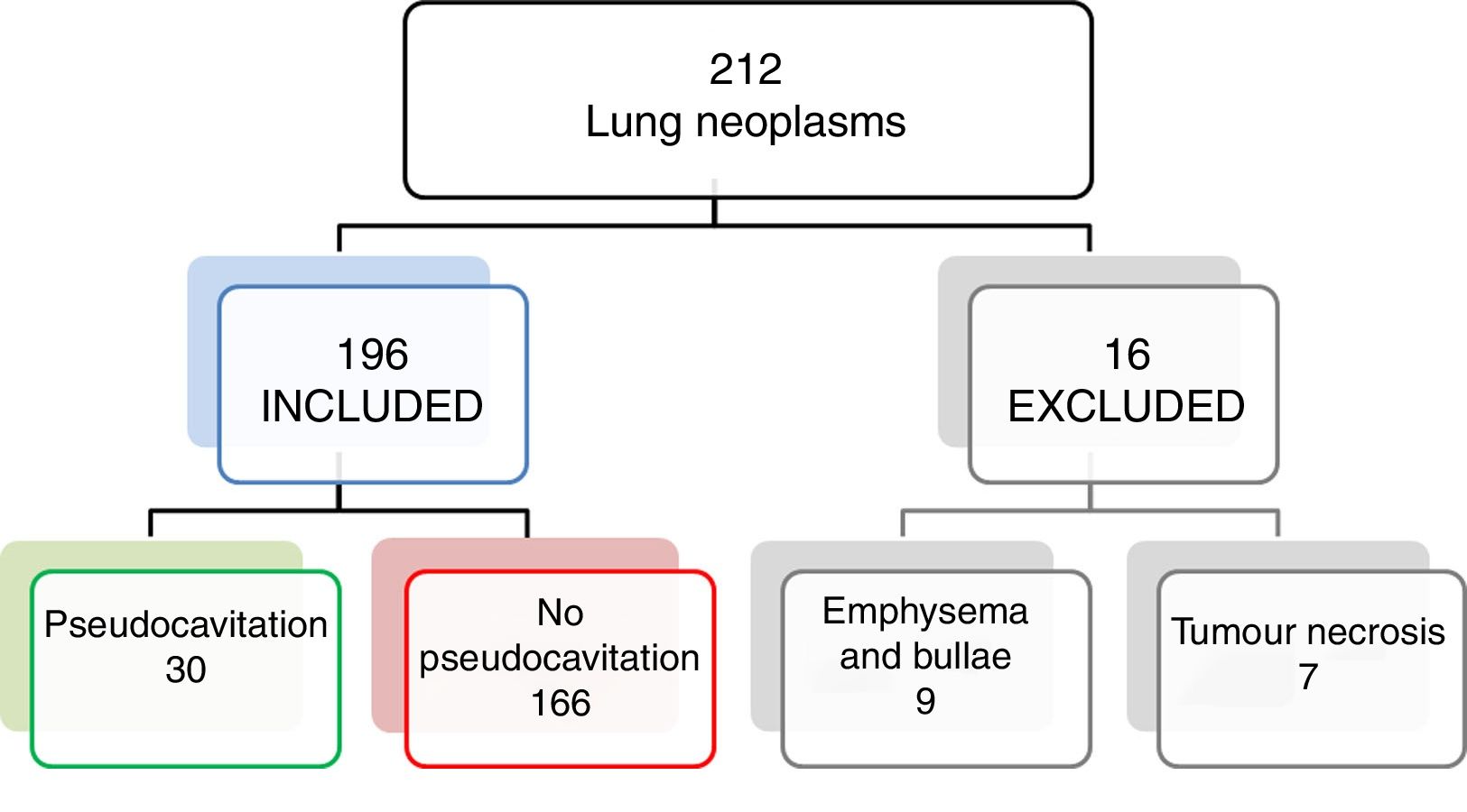
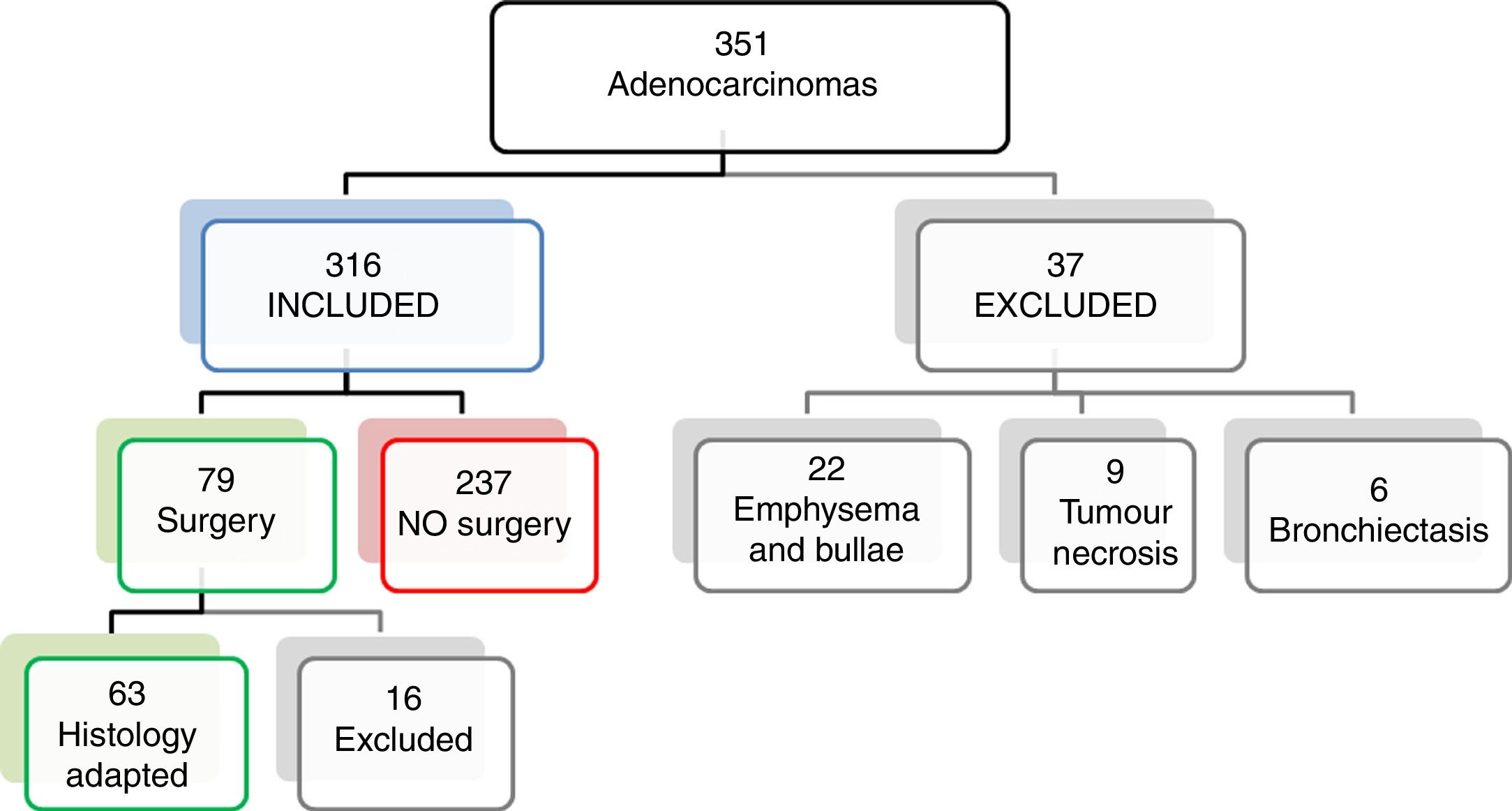
Material and methodsWe retrospectively reviewed chest CT studies for 212 consecutive lung tumors included in a CT perfusion database and for 351 consecutive adenocarcinomas diagnosed between July 2007 and September 2017.
Two radiologists blinded to the pathology report determined whether air cysts were present in the tumors, excluding lesions with necrosis and those surrounded by bullae or emphysema.
We analysed whether the presence of pseudocavitation was associated with the histologic type, size, or EGFR positivity of the tumor as well as with the age or sex of the patient. We also evaluated the relationship with the histologic subtype of the tumor in patients who underwent surgery. We used the chi-square test for categorical variables and logistic regression for continuous variables.
ResultsPseudocavitation was present in 15% of the tumors and was significantly more common in adenocarcinomas (24.1%), p=0.003, although it was also observed in 9.8% of the epidermoid carcinomas and in 3% of the microcytic carcinomas. For the diagnosis of adenocarcinoma, the presence of pseudocavitation yielded 92.4% specificity, 24% sensitivity, 73.3% PPV, 58.4% NPV, and 37.6% accuracy.
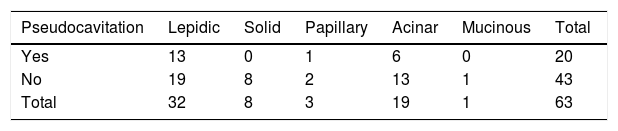
In the resected adenocarcinomas, 65% of the tumors with pseudocavitation had lepidic growth; the prevalence of pseudocavitation was 40.6% in tumors with lepidic growth, 31.5% in those with acinar growth, and 33% in those with papillary growth. Pseudocavitation was significantly more common in women (29%); no differences were found with respect to age, size, or EGFR positivity.
ConclusionsPseudocavitation is more common in adenocarcinomas with lepidic growth and in women.
Evaluar la prevalencia de seudocavitación en las neoplasias de pulmón y si permite predecir el diagnóstico del adenocarcinoma con crecimiento lepídico.
Material y métodosRevisión retrospectiva de las tomografías computarizadas (TC) de tórax de 212 neoplasias de pulmón consecutivas incluidas en una base de datos de perfusión por TC y de 351 adenocarcinomas consecutivos diagnosticados entre julio de 2007 y septiembre de 2017.
Dos radiólogos recogieron la presencia o ausencia de quistes aéreos en el tumor sin conocer los resultados de anatomía patológica, excluyendo las lesiones con necrosis, rodeadas de bullas o enfisema.
Se analizó si la presencia de seudocavitación tenía relación con el tipo histológico, el tamaño de la lesión y la positividad para el receptor del factor de crecimiento epidérmico (EGFR) del tumor, la edad y el sexo del paciente. También se valoró la relación con el subtipo histológico del adenocarcinoma en aquellos pacientes sometidos a cirugía. Se utilizó la prueba de la χ2 para variables cualitativas y el modelo de regresión logística para variables cuantitativas.
ResultadosEl 15% de las neoplasias presentaron seudocavitación, que fue significativamente más frecuente en los adenocarcinomas (24,1%), p=0,003, si bien también se observó en el 9,8% de los carcinomas epidermoides y en el 3% de los carcinomas microcíticos. Presentó una especificidad del 92,4% para predecir el diagnóstico del adenocarcinoma, con una sensibilidad del 24%, un valour predictivo positivo (VPP) del 73,3%, un valour predictivo negativo del 58,4% y una precisión del 37,6%.
En los adenocarcinomas resecados, el 65% de los tumores con seudocavitación presentaron crecimiento lepídico con una prevalencia del 40,6% en lepídicos, 31,5% en acinares y 33% en papilares. Fue significativamente más frecuente en mujeres (29%) y no se encontraron diferencias en función de la edad, tamaño y positividad para EGFR.
ConclusionesLa seudocavitación es más frecuente en los adenocarcinomas con crecimiento lepídico y en mujeres.
Pseudocavitation is defined as a rounded or oval area of low attenuation measuring less than 1cm in diameter, which appears inside nodules, masses, or areas of consolidation. Its appearance on computed tomography (CT) is similar to air bubbles or cysts.1–3
Pseudocavitation or air bubbles inside a lung lesion can be seen in benign lesions, such as infections, but also in lung cancer. Different mechanisms of pathogenesis have been proposed, such as valvular obstruction in the bronchus by tumor cells, disruption of the alveolar wall due to mucus retention, or the formation of air cysts as an intrinsic property of the tumor.4–11
The presence of molecular markers, such as epidermal growth factor receptor (EGFR) or the ALK gene in patients with lung cancer, will determine which cases will benefit from the targeted therapies that are increasingly being used in such situations. There is a growing interest in the radiology literature to identify the radiological signs that suggest the lung cancer histologic type, due to the implications of this factor in therapeutic management. Pseudocavitation, together with ground-glass density or dilatation of the bronchi, could allow radiologists to predict the diagnosis of adenocarcinoma. The new multidisciplinary classification of adenocarcinomas published by the International Association for the Study of Lung Cancer (IASLC), the American Thoracic Society (ATS), and the European Respiratory Society (ERS) in 2011,12 recommends characterising invasive adenocarcinomas by histological subtype, due to the prognostic implications entailed.12–15
The presence of pseudocavitation in a pulmonary tumor lesion has been associated with a high probability of adenocarcinoma with a lepidic growth pattern.1,13,16 However, many of these articles are outdated,5,11 involve small case series, and none, as far as we are aware, correlate lung tumors with the new classification of adenocarcinoma. Moreover, in lung cancer, it is important to differentiate tumor pseudocavitation that develops on a preexisting cystic lesion from cavitation secondary to necrosis due to vascular insufficiency.3 There is some confusion in the scientific literature in this respect, with cases of adenocarcinomas arising on preexisting cystic lesions.9,16
The aim of this study, therefore, is to evaluate the prevalence of pseudocavitation in lung tumors, and to determine whether this sign can predict the diagnosis of adenocarcinoma and lepidic growth in a large sample of cases using the current classification of adenocarcinoma.
Materials and methodsThis is a retrospective study that was approved by the Galician research ethics committee (Regional Government of Galicia, Regional Health Ministry).
We retrospectively reviewed the chest CT scans performed between September 2009 and September 2017 in 212 consecutive patients with lung lesions resulting in a histological diagnosis of lung cancer. We used the database created for a study in CT perfusion parameters in lung cancer17 with the following inclusion criteria: patients older than 18, treatment naive, and with a tumor measuring over 2cm in diameter. We studied the prevalence of pseudocavitation in lung cancer in general, and whether this correlated with the histological type. Following this, and taking into account the higher prevalence of pseudocavitation in adenocarcinomas found in the literature, we performed a retrospective review of chest CTs from 351 consecutive lung adenocarcinomas diagnosed from July 2007 to September 2017. Our aim was to determine the correlation with the adenocarcinoma histological subtype. Figs. 1 and 2 show the flow charts of both databases.
The electronic case histories of the patients were reviewed and the following data were collected: gender, age, smoking habit, reason for consultation, histology, positivity for EGFR or ALK, treatment received, T stage and size of the lesion in each study group.
The chest CTs were performed on three different scanners: Siemens SOMATOM go.Up®, Siemens SOMATOM Definition Flash® and Siemens SOMATOM Emotion 16® (Siemens Healthcare, Forchheim, Germany), using different acquisition protocols that included the following parameters: 100–120kV, tube current modulation (device and computer programme that automatically adjusts the tube current depending on the anatomical and tissue characteristics of the scanned area), soft tissue reconstruction filter, and 2mm-thick slices. The studies were reviewed independently by two radiologists: one third year radiodiagnostics resident, and one specialist in thoracic radiology with 12 years of experience. Discrepancies were resolved by consensus, and both reviewers were blinded to the tumor histological type. Soft tissue window (width 370–400, centre 40–50) and lung (width 1500, centre 500) images were evaluated, and the presence or absence of pseudocavitation inside the tumor was noted.
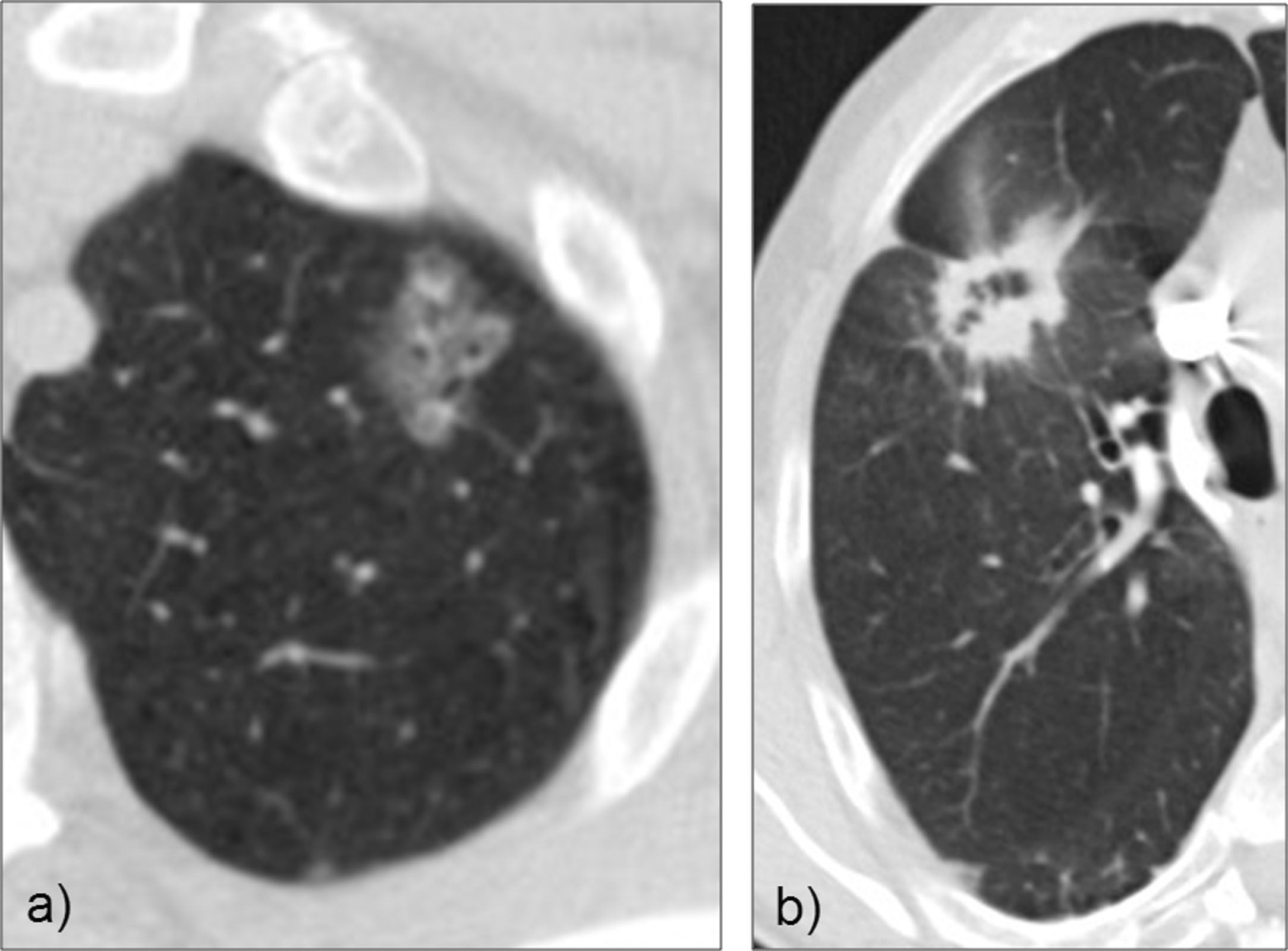
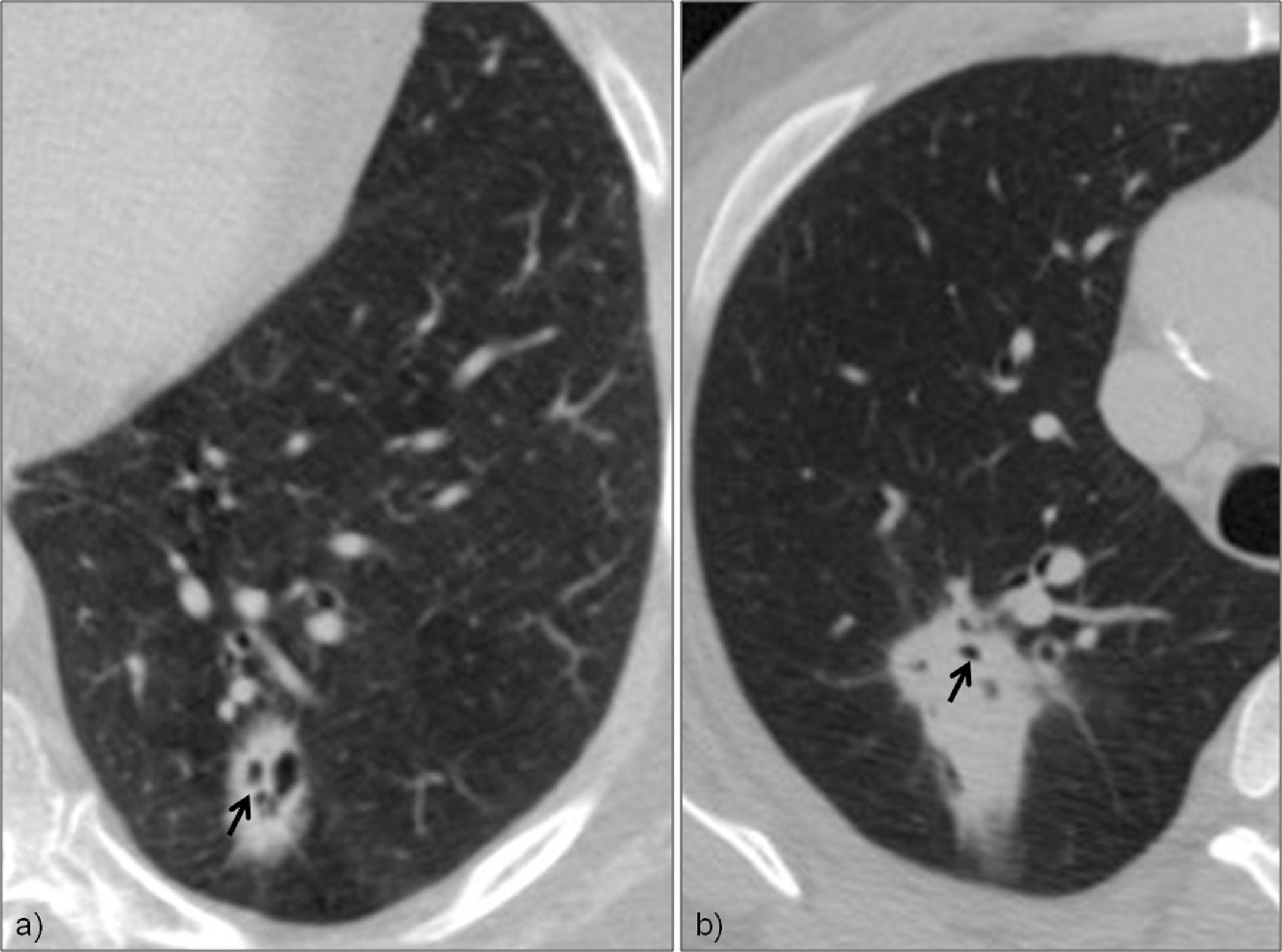
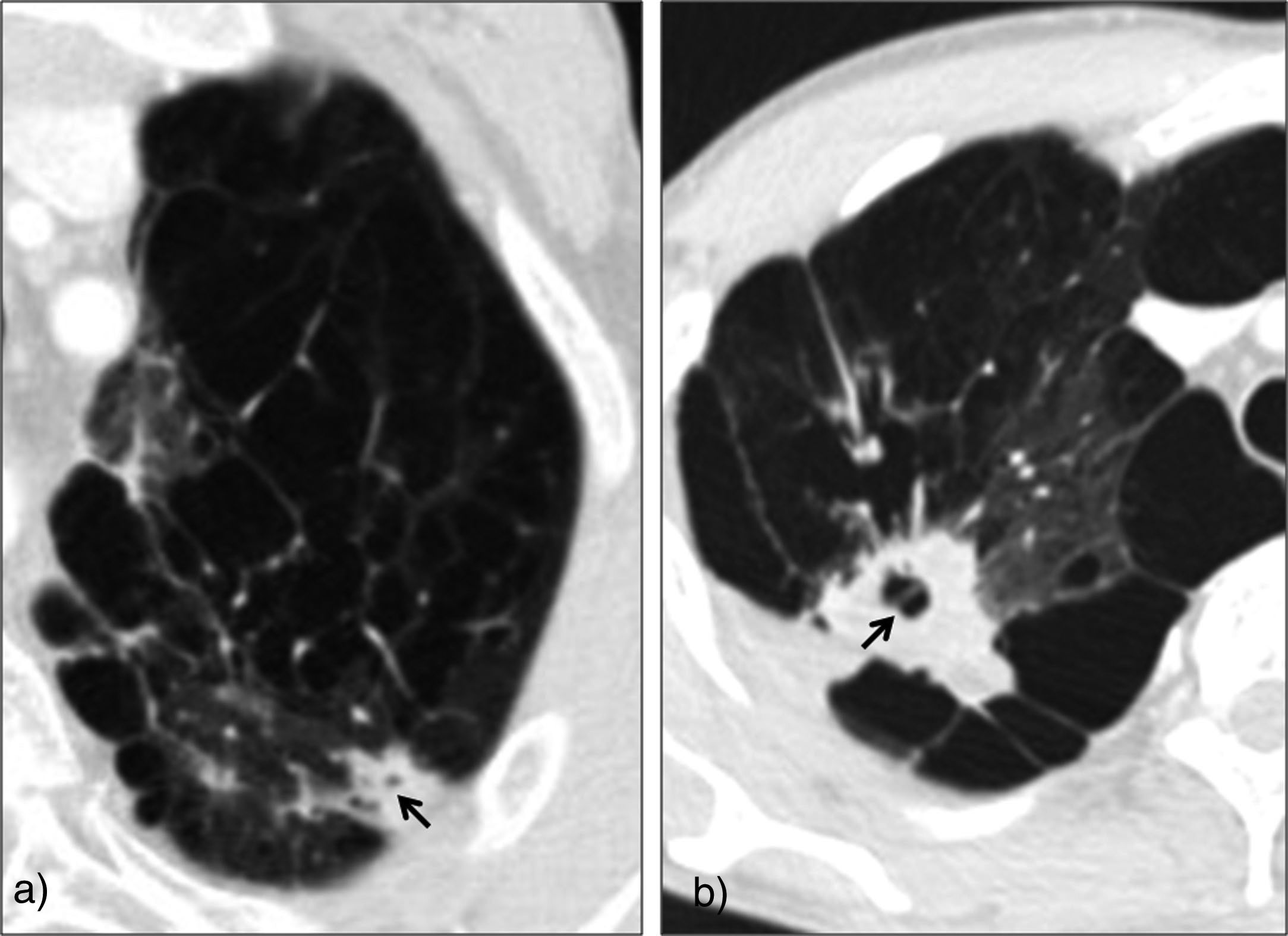
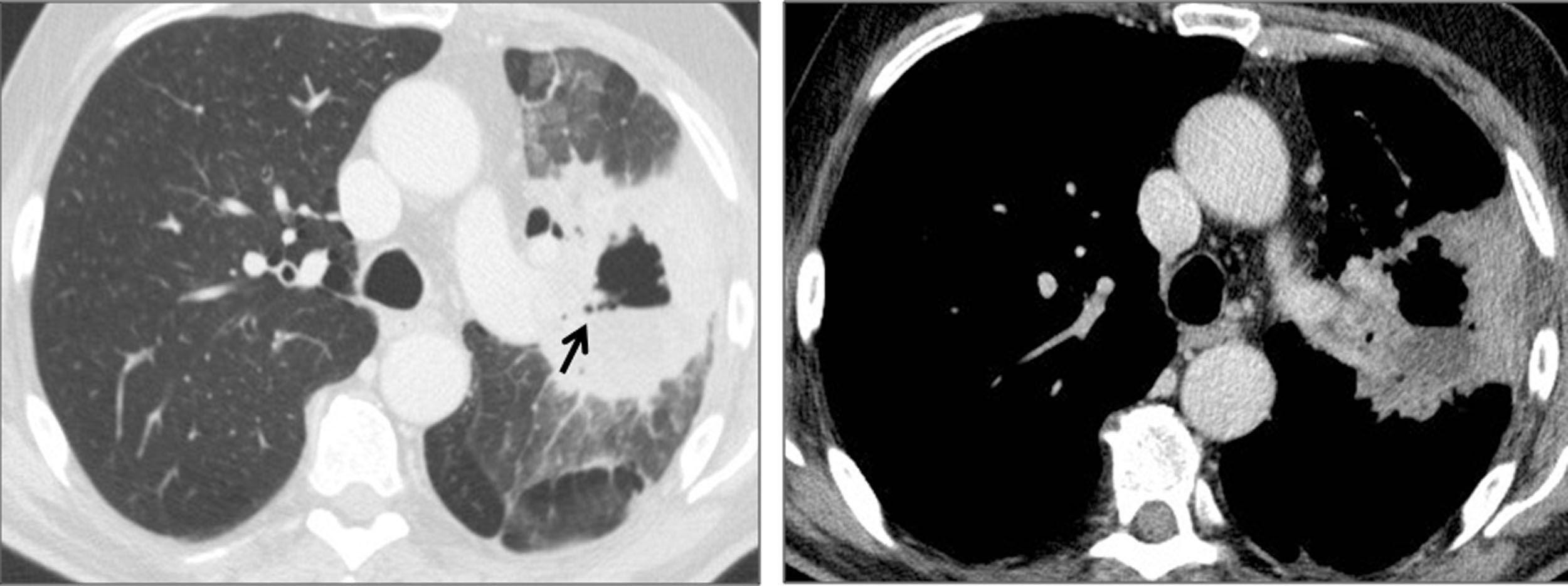
Pseudocavitation was defined as the presence of one or more rounded or oval bubble-like regions measuring less than 1cm inside the lesion (Figs. 3 and 4). Tumors surrounded by bullae or emphysema (Fig. 5), tumors with air bronchogram or necrosis (Fig. 6), and air-filled cysts that communicated with the lung parenchyma surrounding the lesion were excluded.
(a) Patient with severe pulmonary emphysema. The pulmonary neoplasm contains air bubbles, but was excluded from the study because of the possibility that emphysema might be included in the lesion. (b) Solid lesion in the right upper lobe compatible with adenocarcinoma containing pseudocavitation, and surrounded by significant paraseptal and centrilobular emphysema, therefore meeting exclusion criteria.
Lung mass compatible with squamous cell carcinoma affecting the left upper lobe, cavitated, with air-fluid level, and with an area of low attenuation surrounding the cavitation, compatible with necrosis, therefore meeting exclusion criteria.
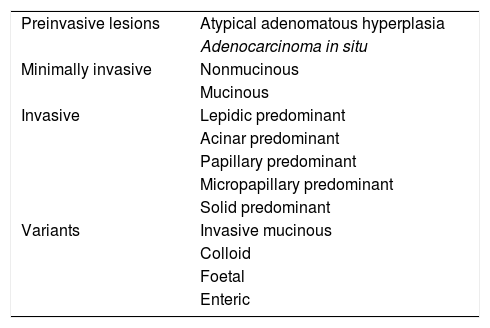
Classification of the International Association for the Study of Lung Cancer, the American Thoracic Society and the European Respiratory Society, 2011.
A thoracic pathologist with eight years’ experience reviewed the pathological reports of the specimens taken from 79 patients with adenocarcinomas treated with complete tumor resection, and adapted the histopathological reports issued prior to 2011 before the new classification of adenocarcinomas. Of these, 16 adenocarcinomas were excluded because the histology report was filed in another hospital and was not available, the histological subtype was not included, or adaptation of the findings to the new classification was inconclusive (Fig. 2).
Statistical analysisThe statistical programme SPSS® (Chicago, IL) version 15 was used for parametric tests. We analysed whether the presence of air cysts inside the mass correlated with the histological type, age, gender, size, and T stage using the χ2 for qualitative variables and logistic regression for quantitative variables.
The χ2 was used to determine whether the presence of pseudocavitation correlated with the adenocarcinoma subtype, and the Student's t-test for independent samples was used to determine the correlation between pseudocavitation and tumor markers.
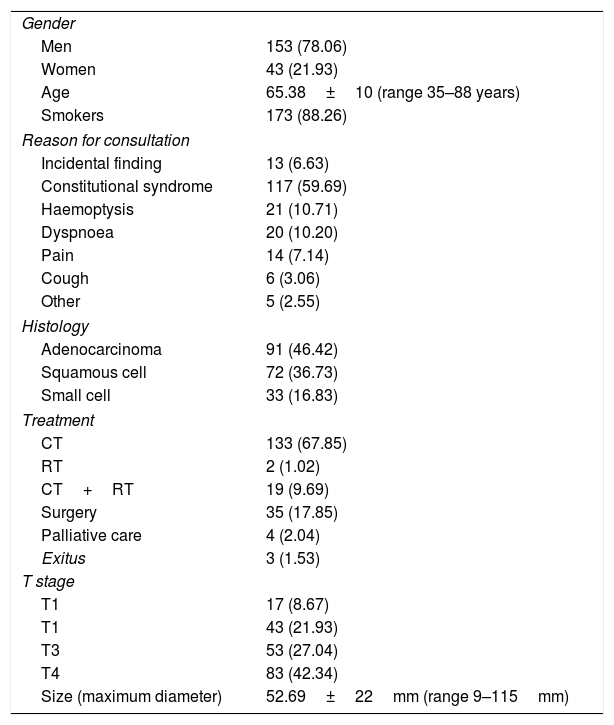
ResultsCorrelation with lung cancerA total of 196 of the 212 patients with lung cancer included in the CT perfusion study database met the inclusion criteria: 153 men and 43 women, with an average age of 65 (range 35–88). Histologically, 91 were adenocarcinomas, 72 squamous cell carcinomas, and 33 small cell carcinomas. Table 1 shows the demographic characteristics of the sample.
Demographic characteristics of patients with lung neoplasms included in a database of CT with tumor perfusion imaging.
| Gender | |
| Men | 153 (78.06) |
| Women | 43 (21.93) |
| Age | 65.38±10 (range 35–88 years) |
| Smokers | 173 (88.26) |
| Reason for consultation | |
| Incidental finding | 13 (6.63) |
| Constitutional syndrome | 117 (59.69) |
| Haemoptysis | 21 (10.71) |
| Dyspnoea | 20 (10.20) |
| Pain | 14 (7.14) |
| Cough | 6 (3.06) |
| Other | 5 (2.55) |
| Histology | |
| Adenocarcinoma | 91 (46.42) |
| Squamous cell | 72 (36.73) |
| Small cell | 33 (16.83) |
| Treatment | |
| CT | 133 (67.85) |
| RT | 2 (1.02) |
| CT+RT | 19 (9.69) |
| Surgery | 35 (17.85) |
| Palliative care | 4 (2.04) |
| Exitus | 3 (1.53) |
| T stage | |
| T1 | 17 (8.67) |
| T1 | 43 (21.93) |
| T3 | 53 (27.04) |
| T4 | 83 (42.34) |
| Size (maximum diameter) | 52.69±22mm (range 9–115mm) |
Percentages are shown in parentheses.
CT: chemotherapy; RT: radiotherapy.
Pseudocavitation was identified in 30 of 196 tumors, giving an overall prevalence of 15.3%. There were significant differences according to the lung cancer histological type, with a predominance of adenocarcinomas p=0.003. The prevalence of adenocarcinomas was 24.1% (22 of 91 tumors), with 9.8% being squamous cell carcinomas (7 of 72 tumors), and 3% being small cell carcinomas (1 of 33 tumors).
The presence of pseudocavitation had a specificity of 92.4% to predict the diagnosis of adenocarcinoma, with a sensitivity of 24%, a positive predictive value (PPV) of 73.3%, a negative predictive value (NPV) of 58.4%, and a diagnostic accuracy of 37.6%.
A significant correlation with gender was found, with a 10% prevalence of pseudocavitation in men and 29% in women (p=0.001).
There was no significant correlation with age (p=0.6), size of the lesion (p=0.85) or T stage (p=0.09).
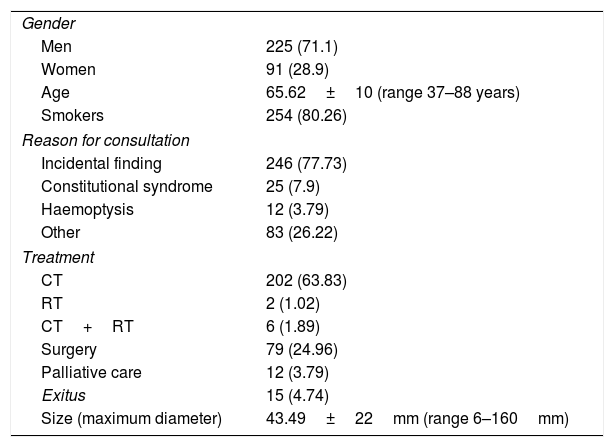
Correlation with adenocarcinomaOf the 351 adenocarcinomas reviewed, 316 met the inclusion criteria, 225 men and 91 women, with an average age of 65 (range 37–88). Table 2 shows the demographic characteristics of this group.
Demographic characteristics of patients with adenocarcinoma.
| Gender | |
| Men | 225 (71.1) |
| Women | 91 (28.9) |
| Age | 65.62±10 (range 37–88 years) |
| Smokers | 254 (80.26) |
| Reason for consultation | |
| Incidental finding | 246 (77.73) |
| Constitutional syndrome | 25 (7.9) |
| Haemoptysis | 12 (3.79) |
| Other | 83 (26.22) |
| Treatment | |
| CT | 202 (63.83) |
| RT | 2 (1.02) |
| CT+RT | 6 (1.89) |
| Surgery | 79 (24.96) |
| Palliative care | 12 (3.79) |
| Exitus | 15 (4.74) |
| Size (maximum diameter) | 43.49±22mm (range 6–160mm) |
Percentages are shown in parentheses.
CT: chemotherapy; RT: radiotherapy.
The presence of pseudocavitation was also significantly more frequent in women (38.7%) than in men (16.6%) in this group, p=0.033. We found no correlation with age (p=0.931), tumor size (p=0.499) or smoking habit (p=0.421).
Information on the adenocarcinoma subtype following the 2011 classification was available in 63 patients treated with complete surgical tumor resection (Table 3). Pseudocavitation was found in 20 tumors (31.7%), of which 13 had a lepidic growth pattern (65%) and seven corresponded to other histological subtypes. The prevalence of pseudocavitation was higher (13 of 32 tumors [40.6%]) in adenocarcinomas that presented lepidic growth. The presence of pseudocavitation had a specificity of 77.4% for predicting lepidic growth, a sensitivity of 40.6%, a PPV of 65%, an NPV of 55.8%, and a diagnostic accuracy of 58.7%, but these differences were not significant (Table 4).
Classification of the International Association for the Study of Lung Cancer, the American Thoracic Society and the European Respiratory Society (2011).
| Preinvasive lesions | Atypical adenomatous hyperplasia |
| Adenocarcinoma in situ | |
| Minimally invasive | Nonmucinous |
| Mucinous | |
| Invasive | Lepidic predominant |
| Acinar predominant | |
| Papillary predominant | |
| Micropapillary predominant | |
| Solid predominant | |
| Variants | Invasive mucinous |
| Colloid | |
| Foetal | |
| Enteric |
The prevalence of pseudocavitation in the remaining histological subtypes was 31.5% (6 of 19) in acinar-predominant adenocarcinomas, 33% (1 of 3) in papillary-predominant adenocarcinoma, and was not observed in any of the eight patients with predominantly solid adenocarcinomas, or in the single case with mucinous adenocarcinoma.
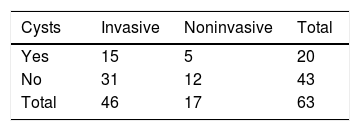
No differences were observed between invasive and non-invasive adenocarcinomas p=0.809 (Table 5).
Mutation studies were requested in 183 patients, 15 of whom were positive for EGFR, six for ALK, and one for ROS; no correlation was found with the presence of pseudocavitation p=0.626.
DiscussionIn our study, we found that 15% of primary lung tumors present pseudocavitation, and this finding is more common in adenocarcinomas and in women. However, although pseudocavitation is more common in adenocarcinomas with lepidic growth, it did not correlate significantly with this histological subtype.
It is important to differentiate pseudocavitation from other cystic lesions associated with lung tumors, such as: tumor necrosis, which is usually central and may contain an air-fluid level, while pseudocavitations are small and usually occur in clusters dispersed inside the tumor; tumors arising in or lying adjacent to an air-filled pulmonary cyst, in which a greater incidence of adenocarcinomas has been described; and bullae or areas of emphysema, which are common in patients with lung cancer. Some published articles describe an association between lung cancer with all these cystic lesions,4,16 which can cause confusion. In our study, we excluded tumors with necrosis, tumors surrounded by bullae or emphysema, and those with air-filled cystic lesions that communicate with the lung parenchyma surrounding the lesion, and only included tumors with cystic appearance or containing small air bubbles.
Different mechanisms of pathogenesis have been proposed to explain the development of pseudocavitations in lung masses. Nambu et al.5 correlated the imaging findings with the pathological specimen in 42 patients with surgically proven adenocarcinomas, and found air-containing spaces in seven cases, cystic spaces surrounded by tumor cells in five cases, mucus-producing cystic airspaces in two cases, and necrosis in three cases. In our study, being retrospective, no pathological correlation was made of the pseudocavitations in the surgical specimens.
It is important to differentiate between lung adenocarcinoma and other histological types, such as squamous cell carcinoma or small cell carcinoma, both from the point of view of prognosis and therapeutic management. This is due to the increasingly frequent use of targeted therapies, which involve the determination of specific tumor markers in the samples obtained for histopathological diagnosis.
Several published studies report that pseudocavitation is a more common sign in adenocarcinoma than in other histological types of lung cancer.1,5,18 However, most scientific studies describe the prevalence of pseudocavitation in adenocarcinoma groups,7,9,19 and few have focussed on its prevalence in lung cancers in general.1,4,20 In our study, we found pseudocavitation in 15% of lung cancers, significantly more frequent in adenocarcinomas (24%), but we also found it in 9% of squamous cell carcinomas and in 3% of small cell tumors. The presence of pseudocavitation showed high specificity (92%) for predicting a diagnosis of adenocarcinoma, but low sensitivity (24%). These results are similar to those of Tailor et al.,1 who found an incidence of 22.1% in adenocarcinomas and 5.6% in other types of non-small cell lung cancers, with a sensitivity of 22% and a specificity of 94%.
Intratumoural cystic airspaces were originally described in variants of bronchioloalveolar carcinoma,11,13 and correspond to lepidic growth in the current classification. In lepidic growth, tumor cells proliferate along the alveolar walls without causing disruption of the pulmonary architecture.1 This growth pattern is associated with a favourable prognosis.1,5,13 Anami et al.13 reported that patients with the mixed subtype of adenocarcinoma who have lepidic growth showed a longer median survival rate than those who do not, and that this is a more reliable prognostic indicator than lymph node stage.13 Tailor et al.1 found that pseudocavitation has a specificity of 85% and a sensitivity of 42% for predicting lepidic growth, similar to that found in our study, where specificity was 77% and sensitivity 40%. The prevalence of pseudocavitation in tumors with lepidic growth was 40.6%, similar to the 41.7% reported by Tailor et al.1 However, the prevalence of other histological subtypes in our study was higher: 22.6% compared to 14.5%.1 In our study, pseudocavitation was found in 31.5% of acinar-predominant adenocarcinomas and in 33% of papillary-predominant adenocarcinomas. No significant relationship was found between pseudocavitation and the type of invasive or non-invasive adenocarcinoma, nor with T stage or size.
A striking finding, after analysing all lung cancers, is that pseudocavitation was significantly more frequent in women, with a prevalence of 29% compared to 10% in men, a finding that could be explained by the higher prevalence of adenocarcinomas in women.21 However, this difference was maintained when we analysed only adenocarcinomas, with a prevalence of 38.7% in women with adenocarcinomas and 16.6% in men with adenocarcinomas. We were unable to find any reference to the correlation between pseudocavitation with gender in any published studies.
The correlation between the morphology of pulmonary tumors on CT and molecular alterations was analysed in 183 patients, eight of which were positive for the EGFR mutation, and none presented pseudocavitation. However, no conclusions can be drawn from this observation, given the small sample size, and larger studies are needed to determine whether pseudocavitation correlates with molecular alterations.
Our study has some limitations: first and foremost, the prevalence of pseudocavitation in lung tumors and their histological types was estimated using data from a group of patients who underwent chest CT with perfusion imaging. Therefore, the sample was restricted by the inclusion criteria of that study, the most important being lesions measuring over 2cm. As we did not find a correlation between pseudocavitation and tumor size, we believe this limitation does not compromise our results. Secondly, this was a retrospective study that includes cases prior to 2011, so histology reports of adenocarcinoma had to be adapted to the current classification. Finally, the chest CTs were performed on three different scanners, which could influence the resolution of the images and the identification of pseudocavitation, although we believe that this impact is minimal or practically nil, since all images were obtained using the same acquisition protocols.
In conclusion, pseudocavitation is more common in women and in adenocarcinomas with lepidic growth.
Authorship- •
Responsible for the integrity of the study: EUP, CTL, FGC, CDSG, AVC, CJB.
- •
Study conception: EUP, CTL.
- •
Study design: EUP, CTL.
- •
Data collection: EUP, CTL, FGC, AVC, CJB.
- •
Data analysis and interpretation: EUP, CTL, FGC.
- •
Statistical processing: EUP, CTL.
- •
Literature search: EUP, CTL, FGC, AVC, CJB.
- •
Drafting of the article: EUP, CTL.
- •
Critical review of the manuscript with intellectually significant contributions: EUP, CTL, FGC, CDSG, AVC, CJB.
- •
Approval of final version: EUP, CTL, FGC, CDSG, AVC, CJB.
The authors declare that they have no conflicts of interest.
Please cite this article as: Utrera Pérez E, Trinidad López C, González Carril F, Delgado Sánchez-Gracián C, Villanueva Campos A, Jurado Basildo C. Seudocavitación en las neoplasias de pulmón. ¿Permite predecir el diagnóstico de adenocarcinoma con crecimiento lepídico? Radiologia. 2019. https://doi.org/10.1016/j.rx.2019.03.004