Transcatheter aortic valve implantation (TAVI) is an alternative to surgical valve replacement in patients with high surgical risk. Although TAVI is becoming more and more common, it is not without complications. Rupture of the aortic root after implantation is an uncommon, but lethal complication; few cases have been described in the literature. Multidetector computed tomography is fundamental before TAVI to evaluate factors that predispose to complications; however, its role after the procedure is still controversial.
El implante transcatéter de válvula aórtica, más conocido por su acrónimo en inglés TAVI (Transcatheter Aortic Valve Implantation) es una alternativa al recambio valvular quirúrgico en pacientes inoperables o con alto riesgo quirúrgico. Sin embargo, es una técnica cada vez más utilizada, que no está exenta de complicaciones. La rotura de la raíz aórtica postimplante es una complicación infrecuente, pero letal, y con pocos casos descritos en la bibliografía. La tomografía computarizada multidetector es fundamental antes del procedimiento TAVI para valorar factores predisponentes a la aparición de complicaciones, mientras que su papel posprocedimiento sigue siendo controvertido.
Transcatheter aortic valve implantation (TAVI) is an alternative to surgical valve replacement in inoperable patients or high-risk surgical patients.
TAVI procedure has its own complications, which have been described by a group of experts and are included in the Valve Academic Research Consortium (VARC) criteria. One of the most feared complications of TAVI is rupture of the aortic root in the fixation areas of the valve device, which is difficult to treat, and can even be life-threatening.1
Multidetector computed tomography (MDCT) plays a fundamental role in selecting suitable candidates based on anatomical and technical criteria, thereby guaranteeing the success of the procedure and avoiding intraoperative complications. It can also be used to evaluate possible procedure-related complications.
Case reportWe present a case of annular and subannular rupture of the aortic root with formation of intracardiac shunt during a TAVI procedure in order to draw attention to the importance of pre-TAVI MDCT in identifying predisposing factors to aortic root rupture and in detecting this complication after surgery.
This was a 79-year-old male patient with hypertension and dyslipidaemia, who was admitted due to syncope. Transthoracic echocardiography (TTE) showed a sclerocalcific tricuspid aortic valve with severely restricted opening and mild regurgitation. The size of the left ventricle was within the upper limit of normal, ejection fraction in the lower limit of normal, and concentric hypertrophy.
The pre-TAVI MDCT confirmed severe aortic stenosis; calcium build-up in the valve was found to be asymmetric, with a greater degree of calcification in the noncoronary leaflet. The following measurements were taken: aortic annulus with a minimum diameter of 20mm, maximum diameter of 25mm, average diameter of 22mm, and 353mm2 in systole, distance from the aortic annulus to the ostium of the right coronary artery 10mm, and to the left coronary artery 12mm. Width of right coronary sinus 23mm, height 16mm, width of left coronary sinus 24mm and height 15mm, and width of non-coronary sinus 25mm and height 17mm. Calcification of the aortic root according to the Agatston score was 3202, without extending to the left ventricular outflow tract or to the annulus.
A 26mm Edwards Sapiens 3 (Edwards Lifesciences, Irvine, CA) balloon-expandable valve, which was post-dilated due to the presence of a paravalvular leak, was implanted directly into the patient. We decided to place the Edwards Sapiens 3 prosthesis and not the CoreValve due to the small dimensions of the sinuses of Valsalva. The device size/mean aortic annulus diameter ratio on MDCT was 1.1. After the procedure, the patient remained asymptomatic and haemodynamically stable.
In the follow-up TTE performed 24h after the procedure, the prosthesis showed thin leaflets with normal opening and mild periprosthetic regurgitation. Two ruptures were detected, one below the valve (very small, in the membranous septum) and another between the right coronary sinus and the right ventricle. The size of the right ventricle was at the upper limit of normal, with normal function and a Qp/Qs index of 1.5.
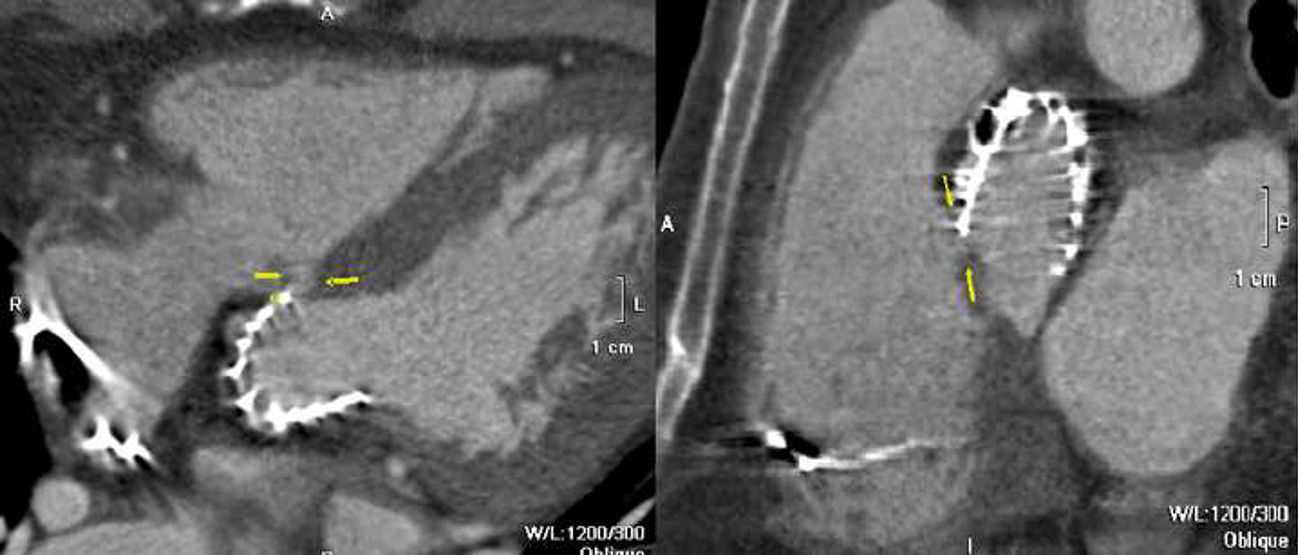
MDCT confirmed the presence of an annular communication between the aortic root and the right ventricle, just below the coronary sinus (Fig. 1), together with a subannular defect in the membranous interventricular septum (intracardiac shunt) (Fig. 2). The subannular defect measured 5mm, and the communication between the aortic root and the right ventricle was 10mm wide and 7mm deep.
Given these findings, the case was discussed during the medical–surgical meeting, and a conservative approach was decided, with close clinical follow-up due to the absence of symptoms and the high surgical risk of the patient. Surgery would be considered if the patient developed symptoms or TTE showed right ventricular dysfunction.
To date, the patient is still under follow-up, asymptomatic, and follow-up TTE has shown persistence of the immediate postoperative findings.
DiscussionRupture of the aortic root in the fixation areas of the prosthesis is a rare and potentially life-threatening complication, with an incidence of 1%. It is an umbrella term for intraoperative lesions in the region of the aortic root and in the left ventricular outflow tract, and is classified as supra-annular, intra-annular, sub-annular and combined rupture, depending on the anatomical location.2 Sub-annular ruptures include injuries to the left ventricular free wall, either below the noncoronary sinus or in the interventricular septum. It can occur during valve replacement surgery, prosthesis delivery, or postdilation due to paravalvular leak. It is more common with balloon-expandable valves, but has also been described with the self-expandable valve, when it is caused by overdilation to treat residual paravalvular regurgitation.3
Pre-TAVI MDCT is very useful for detecting some of the risk factors for aortic root rupture during TAVI, such as: discrepancy between the size of the native annulus and the prosthesis; severe calcification in vulnerable areas; small annulus or root; presence of a severely calcified bicuspid valve; commissural fusion; short distance between the ostium of the coronary arteries and the annulus; severe asymmetric interventricular septum hypertrophy; high Agatston score in the aortic root2; asymmetric calcification of the cusps and long length of the membranous interventricular septum.4
The risk of rupture of the aortic root is increased when the prosthesis is oversized to avoid the risk of postoperative paravalvular leaks, so accurate measurement of the aortic valve annulus is crucial to select the size of the device and prevent rupture of the aortic root. In addition to accurate measurement of the annulus, MDCT can also evaluate the structures surrounding the annulus and the distribution of calcium deposits, which also helps select an appropriately sized valve.5
Our patient was a borderline case, with an aortic annulus measuring 20mm minimum diameter and 25mm maximum diameter, an average diameter of 22mm, narrow root with small sinuses, asymmetric calcification of the leaflets, and short distance between the annulus and the ostium of the coronary arteries. In addition, post-dilation was performed by regurgitation. All these factors could have predisposed the patient to root rupture.
The management of these complications is challenging, and should be discussed by a multidisciplinary team. Treatment can be either surgical or conservative, depending on the location and clinical manifestations. In asymptomatic patients such as ours, conservative management with follow-up serial echocardiograms is usually chosen because it has a better prognosis. Surgical treatment could be considered in patients with a high Qp/Qs ratio if there is significant structural or clinical involvement.
In conclusion, preoperative MDCT plays a fundamental role in assessing the risk factors for perioperative complications, such as rupture of the aortic root. The role of postoperative computed tomography remains unclear and is the subject of intense debate, but its value in detecting periaortic complications is undeniable.1
Authorship- 1.
Responsible for the integrity of the study: IDG, MEGS.
- 2.
Study conception: IDG, MEGS.
- 3.
Study design: IDG, MEGS.
- 4.
Data collection: IDG, MEGS.
- 5.
Data analysis and interpretation: IDG, MEGS.
- 6.
Statistical processing: not applicable.
- 7.
Literature search: IDG, MEGS.
- 8.
Drafting of the article: IDG, MEGS.
- 9.
Critical review of the manuscript with intellectually significant contributions: IDG, MEGS, MCFG, EAH.
- 10.
Approval of final version: IDG, MEGS, MCFG, EAH.
The authors declare that they have no conflicts of interest or sources of funding.
Please cite this article as: Dieste Grañena I, Guillén Subirán ME, Ferrer Gracia MC, Angulo Hervías E. Rotura de raíz aórtica con formación de shunt intracardíaco secundaria a implante valvular aórtico transcatéter. Radiología. 2019;61:341–344.