Coronavirus disease (COVID-19) is an infectious disease that causes both physical and mental sequelae. The aim of the present study was to evaluate the quality of life and the level of depression in post-COVID-19 patients using the SF-36 Questionnaire (SF-36) and the Beck depression inventory (BDI) and to compare it with the quality of life of the general population for the same sex and age group.
MethodsA cohort, observational, and prospective study was designed with the survivors of the group of 115 patients hospitalized at Hospital Público de Monforte to whom the SF-36 and BDI were performed.
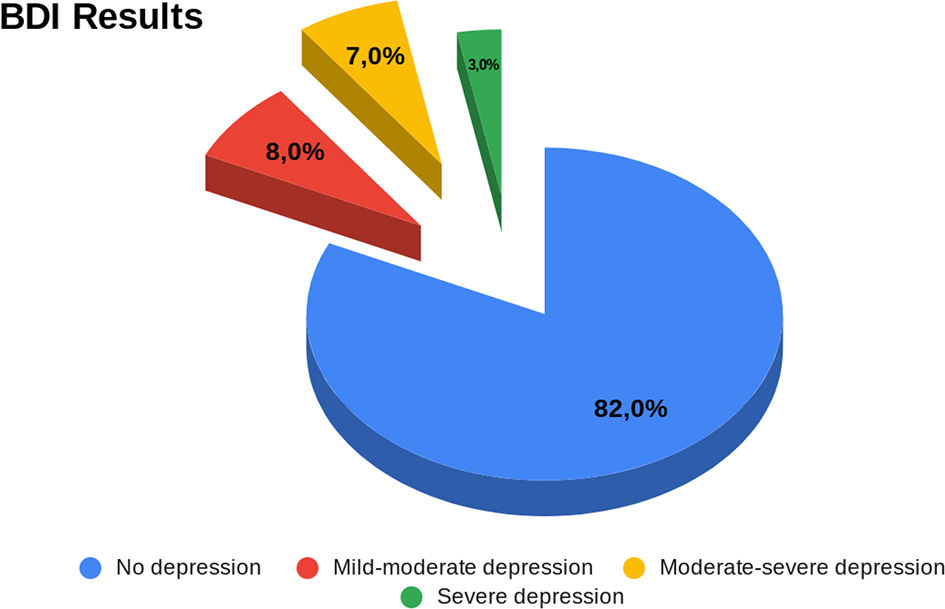
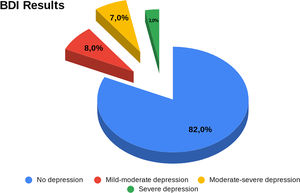
Results60 patients responded to the questionnaires (mean age 65.24 (±15.49) years and 40% women). In the SF-36, the summary of the physical and mental component was, respectively, 47.71(±8.48) and 47.25(±9.39). Women have lower scores than men in half of the components of the SF-36. The probability of depression inferred by SF-36 was 28% and applying BDI results were 81.67% of the sample were not depressed, 8.33% were mild–moderate depressed, 6,67% were moderate–severe depressed, and 3.33% were severely depressed.
ConclusionsPatients who have suffered COVID-19 predisposes to a higher frequency of depression as well as to a worse quality of life in terms of both physical and mental health. This should serve to raise awareness of the follow-up of patients with long COVID-19 in order to prevent, as far as possible, a decrease in their quality of life.
La enfermedad por coronavirus (Covid-19) es una enfermedad infecciosa que causa secuelas tanto físicas como mentales. El objetivo del presente estudio fue evaluar la calidad de vida y el nivel de depresión de los pacientes que han padecido utilizando el cuestionario SF-36 (SF-36) y el inventario de depresión de Beck (BDI), y compararlos con la calidad de vida de la población general para el mismo grupo de sexo y edad.
MétodosEl estudio de cohorte, observacional y prospectivo fue diseñado con los supervivientes del grupo de 115 pacientes hospitalizados en el Hospital Público de Monforte, a quienes se administraron SF-36 y BDI.
ResultadosSesenta pacientes respondieron a los cuestionarios (edad media 65,24 (±15,49) años y 40% de mujeres). En SF-36, el resumen del componente físico y mental fue de 47,71(±8,48) y 47,25(±9,39) respectivamente. Las mujeres tuvieron puntuaciones menores que los hombres en la mitad de los componentes de SF-36. La probabilidad de depresión inferida por SF-36 fue del 28% y aplicando los resultados de BDI el 81,67% de la muestra no tenía depresión, el 8,33% tenía depresión de leve a moderada, el 6,67% tenía depresión de moderada a severa, y el 3,33% tenía depresión severa.
ConclusionesLos pacientes que han padecido COVID-19 tienen predisposición a una mayor frecuencia de depresión, así como peor calidad de vida en términos tanto de salud física como mental. Esto deberá servir para suscitar la concienciación sobre seguimiento de los pacientes con Covid de larga duración, a fin de prevenir, en la medida de lo posible, la reducción de su calidad de vida.
The SARS-CoV-2 created a global pandemic in December 2019.1 Until today, March 9, according to the WHO, the coronavirus disease has caused 759 408 703 confirmed cases, including 6 866 434 deaths globally,2 and it has remained one of the causes of consultation in the health system worldwide. Back in 2020, many countries were caught off guard when COVID-19 began. It is well known that the first country to present many cases was China, after that, countries were alerted. According to an experience in a regional hospital in Galicia (Northwest of Spain) published in 2020, they developed a multidisciplinary approach to be prepared for the epidemic and the hospital later presented a low incidence of the disease3,4 but unfortunately, this was not the case for many other places where the impact of COVID-19 left us with hospitals overcrowded with patients and multiple long-term consequences since the disappearance of acute symptoms is not the end of this condition. Some patients who have suffered COVID-19 may experience long-term effects from their initial illness, well-known as a PC19S (post-COVID-19 syndrome) whose conditions include general symptoms, respiratory, digestive, and heart symptoms.5,6 But a variety of neurological and psychiatric sequelae such as headache, hyposmia, myalgia, neuropathy, encephalopathies, neurocognitive impairment, anxiety, and depressed mood have been reported in patients who have recovered from COVID-19 causing an impact on health-related quality of life (HRQoL).7 According to an investigation carried out in a hospital in Wuhan, China, it was found that 6 months after the onset of COVID-19 symptoms, the majority of patients presented at least one symptom, particularly fatigue or muscle weakness, shortness of breath, and anxiety or depression.8 Many factors can contribute to the impact in the quality of life in COVID-19 survivors, including length of hospitalization, the severity of illness, and possibly obesity. These findings can help the health provider to assist COVID-19 survivors improving their quality of life and previous functional status. According to a short-term mental health correlation study in patients discharged after COVID-19, the results showed that after hospitalization, mental health was impaired due to the long recovery time they stayed in the hospital. Many recovered patients had to be isolated in long-term hospitalizations, which can cause depression and anxiety.9,10
HRQoL is a concept that includes areas related to physical, mental, emotional, and social functioning. It goes beyond direct measures of population health, life expectancy, and causes of death, focusing on the impact of health status on quality of life.11 The 36-item short-form health survey questionnaire (SF-36) is a popular instrument for assessing HRQoL. Component analytics showed 2 distinct concepts measured by the SF-36: a physical dimension, represented by the physical component summary (PCS), and a mental dimension, represented by the mental component summary (MCS).12 Some studies used Beck depression inventory (BDI), 21 self-reported items (4-point scale) used to assess the intensity of physical and cognitive depression and anxiety symptoms during the past week. Studies used this instrument demonstrating that low levels of physical activity had a big impact on the incidence of depression.13 This study aims to investigate if there is impairment in HR-QoL evaluated with the SF-36 after COVID-19 diagnosis in hospitalized patients and assess depression during the COVID-19 pandemic using BDI.
MethodsThis was an observational, prospective cohort study with 115 patients whose inclusion criteria were: older than 18 years old, who had COVID-19 and were hospitalized in the public hospital of Monforte de Lemos. Inclusion criteria were patients who had COVID-19 and were hospitalized at Hospital Público de Monforte (Lugo, Spain). Exclusion criteria were patients less than 18 years old, any kind of dementia, neurodegenerative disorders or neoplasm at an advanced stage. Once the inclusion and exclusion criteria were fulfilled and informed consent had been provided the patients completed SF-36 questionnaire and BDI to assess their general health, limitations of their daily activities, emotional health problems, social activities, feeling of pain, their energy, and their psychological feelings. The SF-36 is a very popular instrument for assessing HRQoL. Component analytics showed that there are 2 distinct concepts measured by the SF-36: a physical dimension, represented by the physical component summary (PCS), and a mental dimension, represented by the mental component summary (MCS). All the scales contribute in different proportions to the score of the PCS and MCS measures.12 BDI, 21 self-reported items (4-point scale) is used to assess the intensity of physical and cognitive depressive symptoms during the past week. Many studies used this instrument demonstrating that low levels of physical activity had a big impact in the incidence of depression.13 The SF-36 is considered a generic 36-item questionnaire that measures self-perceived health in 8 dimensions or domains of health status: physical function, physical role, bodily pain, general health, vitality, social function, emotional role, and mental health that can be summarized into 2 summary components of physical health and mental health. Each of the domains has several items that together total 36, and each of the items has a scale of scores. The sum of the points for each of the items gives an overall score (scale between 0 and 100, with 100 being the best perceived quality of life). The test detects both positive and negative health states, and the content of the questions focuses on functional status and emotional well-being and it has a high internal consistency and reproducibility. Alonso et al. have validated the Spanish version of the SF-36, with a Cronbach's alpha value above 0.7 in all domains (range 0.71–0.94), except in the social relationship (alpha = 0.45); therefore, it is recommended for quality of life assessments in patients in our setting. It is a widely validated instrument for use in Spanish and standardized data are available in the general Spanish population for comparison of the results. It is a self-administered questionnaire, although it has also been used by interviewers, by telephone or by computer support. For the comparison of the scores of the different scales of the SF-36 health questionnaire with the general population, we have used the data published for the Spanish population over 60 years of age.14 A gender-differentiated comparison was made and the 5-year age range was established, which corresponded to the mean age of our patient sample. The average duration of the interview was approximately 15 min and was carried out after verbal and written informed consent had been given.
The study design ensured the integrity of the data; completion of the questionnaires was reviewed in the presence of the patient to avoid the problem of non-response to the SF-36; therefore, each question analyzed had 100% of responses answered.
Statistical analysisThe Health Institute method with computer support was used to calculate the questionnaire score. Quantitative variables were described using measures of central tendency (mean or median) and dispersion (standard deviation [SD]). Qualitative variables were described using frequency tables and percentages.
A bivariate analysis was performed with the statistical tests that correspond according to the type of variable: Chi square for qualitative variables and t of Student Fisher for quantitative variables. Non-parametric tests were applied when the variables did not follow a normal distribution. Correlation coefficient and receiver operating characteristics (ROC) curves and areas under the curve (AUC) were calculated to determine the relationship and predictive ability of the test.
Database and statistical analysis were performed using SPSS for Windows version 21.0 (SPSS Inc., Chicago, IL) and EPIDAT 3.1 (Dirección Xeral de Saúde Pública, Santiago de Compostela, Spain). A p-value <.05 was considered to be statistically significant.
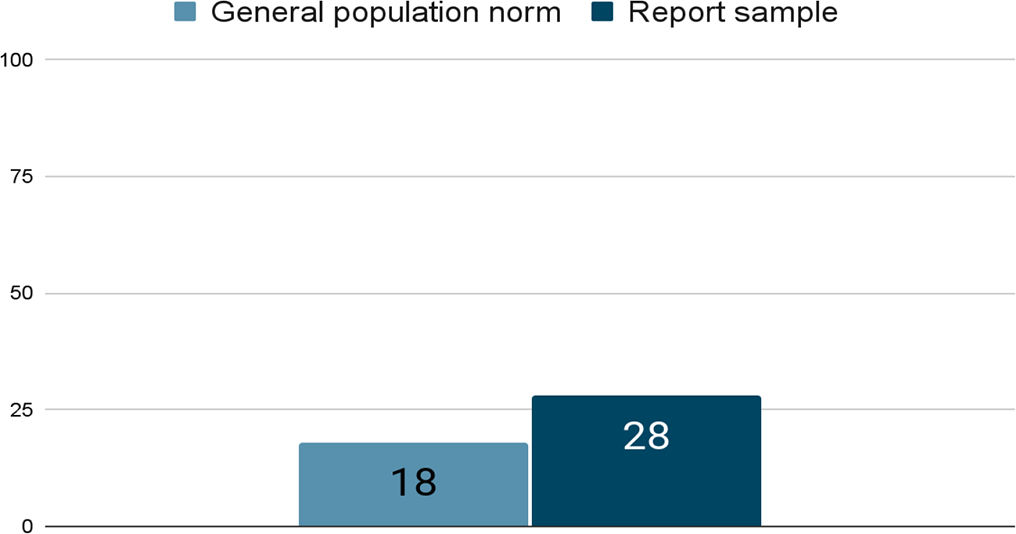
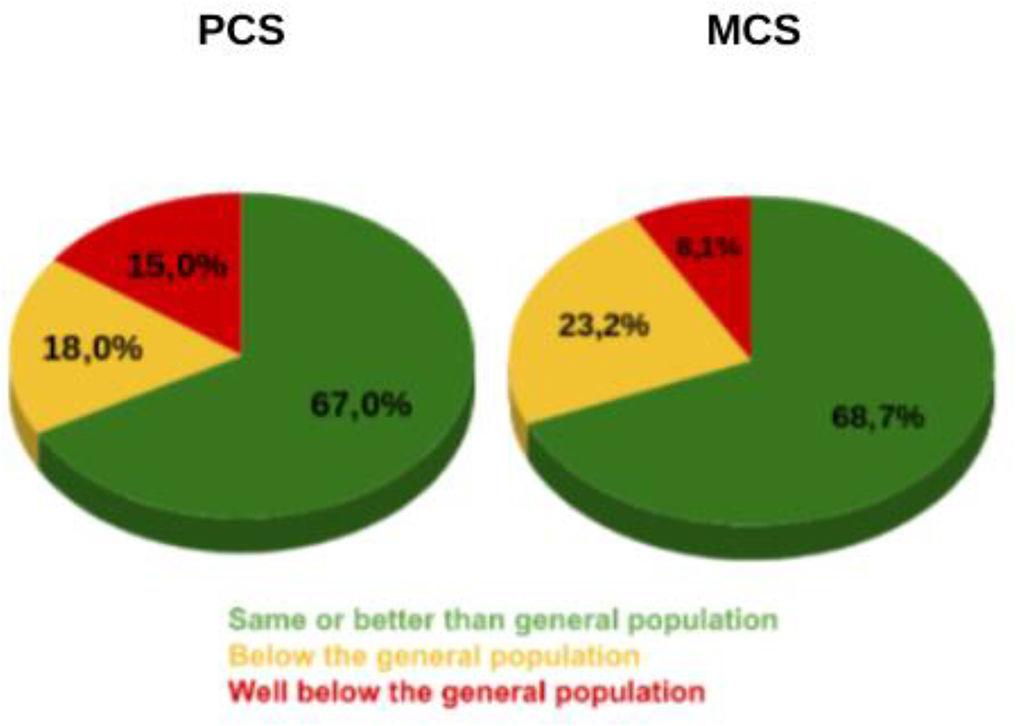
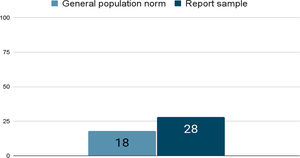
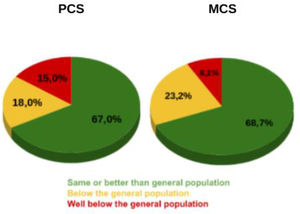
ResultsInitially, 115 patients were recruited into the study and we got data and analyzed the results of 60 (52.17%)of them. 36 (60%) of our sample being males and 24 (40%) females. The mean age of the sample was 65.24(±15.49) years. According to the SF-36 test, the probability of having depression in our sample is 28%, while the probability in the general population is 18% (Fig. 1). All the components of the SF-36 questionnaire, PCS, MCS, GH, PF, RP, BP, VT, SF, RE, MH in our sample are below the norm of the general population. After analyzing the physical component (PCS) of the SF-36 questionnaire, 67% of the sample was the same or better than the general population, 18% below the general population, and 15.0% well below the general population (Fig. 2). The summary results from the mental component (MCS) of the SF-36 in our sample was 68.7% the same or better than the general population, 23.2% below the general population, and 8.1% well below the general population (Fig. 2).
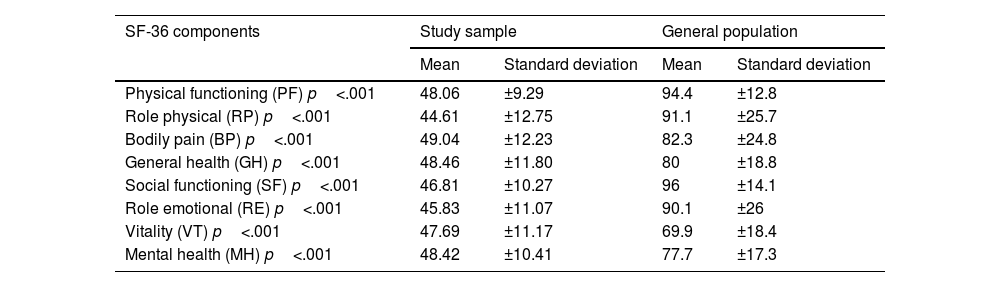
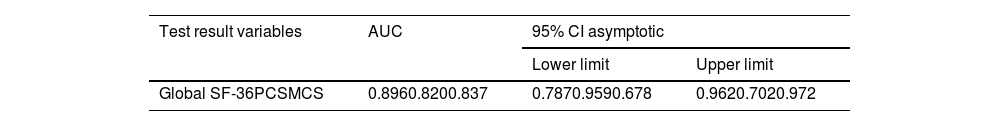
Descriptive general results of each SF-36 component in our study and the comparison in the SF-36 Components between our sample and the general population of same age and gender (p<.001) are shown in Tables 1 and 2. The most decreased items in our sample compared to the general population are physical role and emotional role. In relation with BDI, we found that 81.67% of the sample were not depressed, 8.33% were mild–moderate depressed, 6.67% were moderate–severe depressed, and 3.33% were severely depressed (Fig. 3). Subsequently, when studying the correlation between the results of the BDI and the SF36, it was found that the correlation was −0.578 with respect to the PCS component, −0.606 with the MCS component, and −0.744 in the Global score. When studying the predictive capacity of depression using the global scores of the SF-36 test, it was found that the value of the AUC=0.896 CI 95%=[0.787–0.959] Using the cut-off point obtained in the ROC curve (optimal cut-off point=45.55) for the global SF-36, the value of sensitivity and specificity were Se=77.55% (95% CI: 64.12–86.98), specificity: Sp=90.91% (95% CI: 62.26–98.38) and the positive-predictive value and a negative-predictive value were PV+=65.19%, PV-=94.86%.
Average values and standard deviation of the SF-36 in the study compared to the general population. p-values were calculated using Student's t-test and U de Mann–Whitney test.
| SF-36 components | Study sample | General population | ||
|---|---|---|---|---|
| Mean | Standard deviation | Mean | Standard deviation | |
| Physical functioning (PF) p<.001 | 48.06 | ±9.29 | 94.4 | ±12.8 |
| Role physical (RP) p<.001 | 44.61 | ±12.75 | 91.1 | ±25.7 |
| Bodily pain (BP) p<.001 | 49.04 | ±12.23 | 82.3 | ±24.8 |
| General health (GH) p<.001 | 48.46 | ±11.80 | 80 | ±18.8 |
| Social functioning (SF) p<.001 | 46.81 | ±10.27 | 96 | ±14.1 |
| Role emotional (RE) p<.001 | 45.83 | ±11.07 | 90.1 | ±26 |
| Vitality (VT) p<.001 | 47.69 | ±11.17 | 69.9 | ±18.4 |
| Mental health (MH) p<.001 | 48.42 | ±10.41 | 77.7 | ±17.3 |
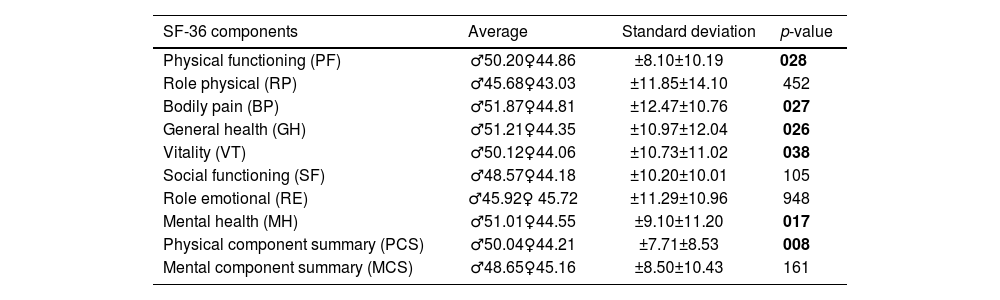
SF-36 scores by gender. p-values were calculated using Student's t-test and U de Mann–Whitney test.
| SF-36 components | Average | Standard deviation | p-value |
|---|---|---|---|
| Physical functioning (PF) | ♂50.20♀44.86 | ±8.10±10.19 | 028 |
| Role physical (RP) | ♂45.68♀43.03 | ±11.85±14.10 | 452 |
| Bodily pain (BP) | ♂51.87♀44.81 | ±12.47±10.76 | 027 |
| General health (GH) | ♂51.21♀44.35 | ±10.97±12.04 | 026 |
| Vitality (VT) | ♂50.12♀44.06 | ±10.73±11.02 | 038 |
| Social functioning (SF) | ♂48.57♀44.18 | ±10.20±10.01 | 105 |
| Role emotional (RE) | ♂45.92♀ 45.72 | ±11.29±10.96 | 948 |
| Mental health (MH) | ♂51.01♀44.55 | ±9.10±11.20 | 017 |
| Physical component summary (PCS) | ♂50.04♀44.21 | ±7.71±8.53 | 008 |
| Mental component summary (MCS) | ♂48.65♀45.16 | ±8.50±10.43 | 161 |
The COVID-19 pandemic has had a significant impact on the quality of life for people all around the world and with the ongoing spread of the virus, many individuals have experienced a decline in their mental and physical health, as well as their social and economic well-being. One of the biggest impacts of COVID-19 on quality of life has been the stress and anxiety it has caused, but in COVID-19 patients, there is an elevated risk of other organic diseases.15–18 In our hospital, we tried to study the quality of life and the frequency of depression in patients hospitalized for COVID-19. Some authors indicate that neurological alterations reach 36.4%19–22 and many of them present a chronic course and difficult management. However, neuropsychological alterations,23–26 although frequent, have not been studied as frequently. In some cases, post-COVID-19 syndrome with neuropsychological sequelae has been diagnosed as chronic fatigue syndrome27–30 IBS31 and other disorders such as brain fog.32 Other studies associate post-COVID-19 syndrome with high risk of suicide indicating significant emotional lability in patients with moderate or severe COVID-19.33–35 Depression is one of the diagnostic entities most closely related to suicide.36 Although some studies conducted during the pandemic showed that depression during confinement was a protective factor for suicide.37 Post-COVID-19 damage is reflected even in imaging techniques38 indicating organic alterations as a substrate of the psycho-functional alterations and the previous mental response such as excessive fear of the disease or anxiety could condition a higher risk of later mental sequelae.39 The HRQoL of patients with post-COVID-syndrome is still reduced months after infection and so is their occupational performance. In particular, the number of symptoms could have an influence on this deficit.40 The fear of contracting the virus, as well as the social isolation and economic uncertainty it has taken a toll on people's mental health. Many people have reported feeling depressed, anxious, and overwhelmed by the pandemic's effects on their daily lives. Persistence of symptoms was associated with poor MCS and PCS, so it is important to follow-up not only patients discharged from the hospital after SARS-CoV-2 infection, but also those under ambulatory management to provide them with rehabilitation and psychological therapy to improve their QoL.41 Despite good independence in activities of daily living and perceived health, individuals surviving the COVID-19 may not have fully recovered their premorbid functioning status seven to 15 months after the infection.42 The clinical sequelae associated with prolonged COVID-19 may persist for at least 9 months after hospital discharge in most patients and may impair long-term HRQoL in more than half of patients, regardless of disease severity and clinical–demographic characteristics43 as we have shown in our study. Depression is one of the most common symptoms of post-COVID-19 syndrome. Patients with a pre-pandemic existing psychiatric disorder were found to be at increased risk for long COVID-19 psychiatric symptoms.44 There are 2 hypothesized immune pathways by which SARS-COV-2 infection can lead to the development of enduring depression: SARS-COV-2 infection can induce cytokine dysregulation by activating the release of pro-inflammatory cytokines and the second can directly invade the brain causing direct brain damage.45,46 As in our study, 30%–40% of COVID-19 survivors have been found to have depression and due to the high percentage of post-COVID-19 survivors with depression, it is important to explore different treatment options47 because a rapid response to SSRIs was found after 4 weeks of treatment.48 As we previously saw PC19S involved many different symptoms and systems and other treatment options were studied, e.g., Traditional Chinese exercises49 were found to be effective in many symptoms of PC19S, such as chronic fatigue, anxiety, depression, and sleep. Another treatment possibility is multidisciplinary rehabilitation that may be effective in reversing some of the long-term effects of PC19S.50 Other authors have studied the relationship between quality of life with SF36 questionnaires in certain pathologies and we can observe a decrease of the quality of life as well as in our study: The results were lower in the physical dimensions than in the mental dimensions of the SF-36 in patients with heart failure,51 the physical functioning in the SF-36 was lower in substance abusers than in their caregivers, 52 the physical role in the SF-36 was decreased in people suffering from addiction than in the general population53 and the quality of life of diabetic patients was found to be lower than normal population.54 After comparing the results from our study with the general population, we found significant p-values. Women have worse scores in the SF-36 than men in half of the components except for role physical, social functioning, role emotional, and mental component summary (Table 3). Comparing the results from the SF-36 according to age intervals, it was found a significant p-value of 0.026 in the PF item.
Reviewing the medical literature, this is the only study to date to simultaneously assess quality of life and depression in post-COVID-19 patients and after analyzing all the data from the SF-36 questionnaire, we found that our report sample is at a 10% more likelihood of suffering depression than the general population, although the results of BDI showed a similar percentage of depression to that of the general population. But in spite of the differences in the degree of depression between the SF-36 and BDI, the ROC curve shows high sensitivity and specificity. This difference between both tests may be due to the small sample size of our study.
In addition to mental health concerns, COVID-19 has also had a significant impact on physical health since the virus itself can cause severe illness and even death, and the measures taken to control its spread, such as lockdowns and social distancing, have led to reduced physical activity, poor nutrition, and other health issues. The lack of access to medical care and clinical particularities that conditioned the health system and particularly the continuity of care in mental pathology has also impacted mental and physical health. Furthermore, the pandemic has had economic consequences that have affected people's quality of life. Many people have lost their jobs or had their incomes reduced, leading to financial stress and insecurity. This has also led to increased food insecurity and homelessness for some. Despite the challenges posed by the pandemic, there have also been some positive changes in quality of life: many people have developed new hobbies, spent more time with family, and found new ways to connect with others through technology. In addition, the pandemic has led to a renewed appreciation for essential workers and increased attention to the importance of public health. Overall, the COVID-19 pandemic has had a significant impact on the quality of life for people around the world and has also had a high negative impact on health workers causing a significant increase in burnout syndrome55,56 and also an upswing in depression and suicidal ideation in healthcare workers.57 This aspect is very relevant since Spanish physicians have a higher risk of suicide than the general population (especially women).58
LimitationsOur study has certain limitations: a small sample size (Caucasian patients only), it is single-center, with no control group, and no long-term follow-up of the patients, so extrapolation of the results should be made with caution.
ConclusionsWith our work, we provide some evidence that having suffered COVID-19 predisposes to a higher frequency of depression as well as to a worse quality of life. We can affirm that a significant percentage of patients who suffered moderate to severe COVID-19 have varying degrees of depression and impairment of their quality of life from both the physical and mental points of view, so that prospective multicenter studies with a larger sample size should be carried out to confirm these results and this should serve to raise awareness of the follow-up of patients with long COVID-19 in order to prevent, as far as possible, a decrease in their quality of life.
Ethical issuesPatient data were processed in accordance with the Data Protection Law L.O. 15/99, of December 13, 1999, on the protection of personal data, and the use of medical records for non-medical purposes (Law 3/05, modifying Law 3/01, regulating informed consent and the medical records of patients).
Scientific and ethical permission to conduct this study was obtained from the Provincial Research Ethics Committee of Málaga (Spain), in the context of REGINA-COVID Study. Informed consent was obtained from patients for the purpose of publication. Personal data were processed in strict compliance with Spanish Law 14/2007, of July 3, on Biomedical Research; Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data (General Data Protection Regulation); and Spanish Organic Law 3/2018, of December 5, on Personal Data Protection and the Guarantee of Digital Rights.
FundingThe research used no funding or financial support at any stage.