Glioblastoma multiforme (GBM) is an aggressive who grade IV primary brain tumor, yet extracranial metastasis occurs in less than 2% of cases due to the protective effects of the blood–brain barrier and lack of lymphatic drainage. This report describes a 79-year-old woman diagnosed with GBM after resection of a right occipital lesion invading the transverse sinus. Following surgery and radiotherapy, radiological progression was noted seven months later. A PET-CT scan revealed multiple suspicious pulmonary nodules, and further evaluation confirmed right-sided pleural effusion with lymphocytic predominance. Biopsy of a right upper lobe mass demonstrated pulmonary metastasis of glioblastoma, ruling out a second primary lung tumor. The patient required repeated thoracenteses and later pleurodesis, but her condition worsened, leading to death two months after metastasis diagnosis. This case highlights the rarity yet possibility of GBM spreading beyond the central nervous system, especially following neurosurgery or sinus invasion, emphasizing the need for clinical vigilance when systemic symptoms appear.
El glioblastoma multiforme (GBM) es un tumor cerebral primario agresivo de grado IV, pero la metástasis extracraneal se produce en menos del 2% de los casos debido a los efectos protectores de la barrera hematoencefálica y a la falta de drenaje linfático. Este informe describe el caso de una mujer de 79 años diagnosticada con GBM tras la resección de una lesión occipital derecha que invadía el seno transverso. Tras la cirugía y la radioterapia, se observó una progresión radiológica siete meses después. Una PET-TC reveló múltiples nódulos pulmonares sospechosos, y una evaluación más detallada confirmó un derrame pleural del lado derecho con predominio linfocítico. La biopsia de una masa en el lóbulo superior derecho demostró metástasis pulmonar de glioblastoma, descartando un segundo tumor pulmonar primario. La paciente requirió repetidas toracocentesis y posteriormente pleurodesis, pero su estado empeoró, lo que le provocó la muerte dos meses después del diagnóstico de metástasis. Este caso pone de relieve la rareza, pero también la posibilidad, de que el GBM se extienda más allá del sistema nervioso central, especialmente tras una neurocirugía o una invasión del seno, lo que subraya la necesidad de vigilancia clínica cuando aparecen síntomas sistémicos.
Glioblastoma multiforme (GBM) is a who grade 4 glioma and the most common malignant primary brain tumor.1 Despite its an aggressive behavior, less than 2% of patients develop extraneural metastasis.1
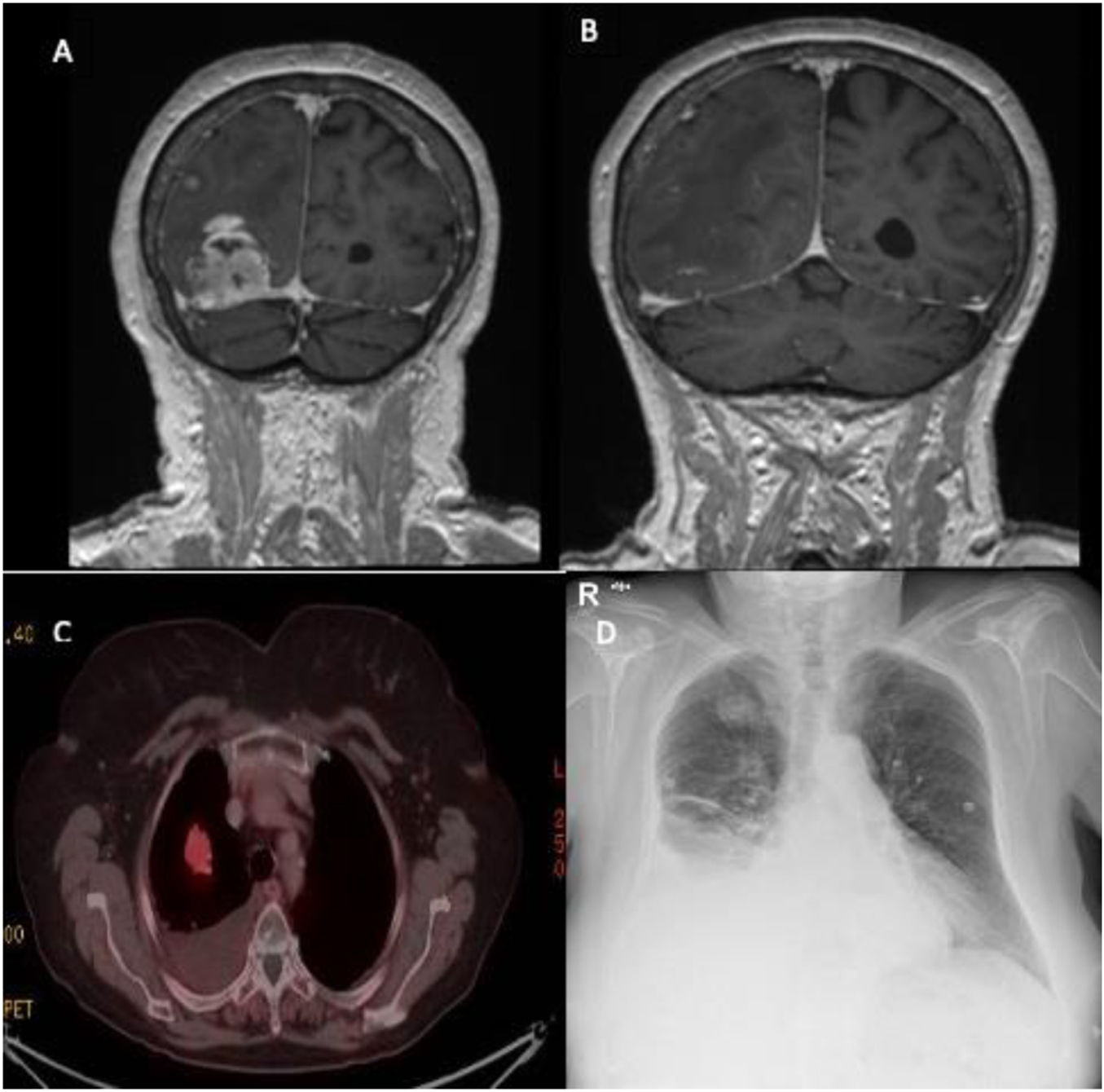
We present the case of a 79-year-old woman diagnosed with GBM after surgical resection of a right occipital lesion invading the transverse sinus, identified through cranial computed tomography (CT) and magnetic resonance imaging (MRI) (Fig. 1A, B), performed due to neurological symptoms. After partial resection, she underwent radiotherapy. Seven months later, radiological progression was observed, and a positron emission tomography-computed tomography (PET-CT) scan was performed for further evaluation.
(A and B) A magnetic resonance scan showed a right occipital lesion of rounded morphology close to the confluence of the venous sinuses, with invasion of the transverse sinus. (C) A positron emission tomography scan showed in the lung parenchyma a solid nodule in the right lung, which shows a slight increase in uptake, with a suspicious appearance. (D) A chest X-ray showed right pleural effusion and a pulmonary nodule in the right upper lobe.
The PET-CT scan (Fig. 1D) showed multiple solid nodules in the right lung parenchyma, suspicious for malignancy. The patient reported exertional dyspnea and right-sided rib pain without infectious signs. A chest X-ray revealed right-sided pleural effusion and a pulmonary nodule in the right upper lobe (Fig. 1C). Pleural fluid analysis confirmed an exudative effusion with lymphocytic predominance. Laboratory tests were within normal limits.
Given the potential for a second primary pulmonary neoplasm, a biopsy of the right upper lobe lesion was performed. Histopathology confirmed pulmonary metastasis of glioblastoma.
During follow-up, multiple thoracentesis were required before chest tube placement and talc pleurodesis. Unfortunately, the patient's condition progressively deteriorated and she died two months after the diagnosis of pulmonary metastasis.
GBM accounts for 12–15% of all primary brain tumors. Despite advances in neurosurgery, radiotherapy, and chemotherapy, median survival remains poor, between 12.1 and 14.6 months. Extraneural and extracranial metastases (ENM) from primary central nervous system tumors are rare and diagnostically challenging.2
The rarity of extracranial metastasis is attributed to the protective role of the blood-brain barrier and lack of a lymphatic drainage system. Nevertheless, rare cases of hematogenous spread and direct implantation have been reported.3
The incidence of ENM due to primary intracranial gliomas it usually occurs in the later stages of the disease, and mostly takes place following craniotomy for tumor excision, as in the case of our patient. The high incidence of ENM after neurosurgery reported was likely secondary to inadequate closure of dura that may result in direct communication between tumor cells and extra-meningeal vessels lymphatics.4
Although risk factors for GBM metastasis are not fully defined, prolonged survival has been proposed as a potential contributing factor. In our case, both tumor invasion of the transverse sinus and prior neurosurgery may have facilitated extracranial spread.5
This case underscores the importance of considering pulmonary metastasis in GBM patients with systemic symptoms, especially after neurosurgical intervention and sinus involvement.
Artificial intelligence involvementNone.
Informed consentIn this case, informed consent was obtained verbally from the patient's family member due to the patient finally pass away.
FundingThe authors received no financial support for the research and/or authorship of this article.
Authors’ contributionWe verified that all authors had access to the data and a role in the drafting of the manuscript.
Conflicts of interestNone.