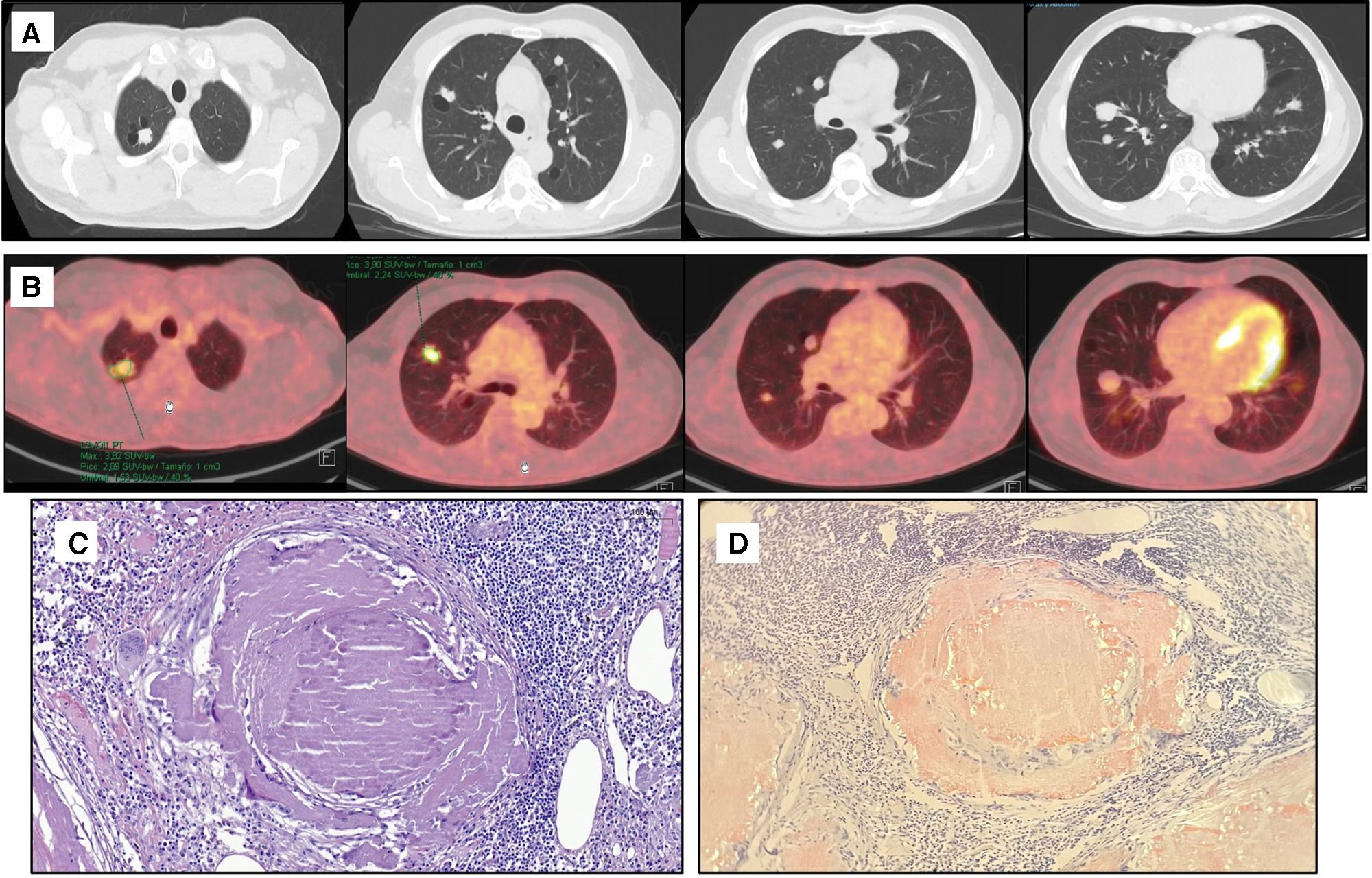
A 59-year-old male without medicals records was incidentally diagnosed with multiple bilateral pulmonary nodules. Thoracic TC showed multiple, bilateral, rounded, with well-defined but irregular contours nodules ranging from 0.5 to 2.7cm, suspected to be metastases (Fig. 1A). PET-TC revealed heterogeneous uptake (Fig. 1B). Differential diagnoses include inflammatory, infectious processes or primary pulmonary neoplasia with bilateral metastases containing cystic and necrotic components. Surgical wedge resection of three nodules from the right upper lobe was performed by VATS, based on their different size, peripheral location and PET uptake. Histopathology examination confirmed AL nodular amyloidosis (Fig. 1C and D). Postoperative course was satisfactory with discharge 24h after surgery. Amyloidosis is an unusual pathology which results from accumulation of misfolded extracellular insoluble protein. Nodular pulmonary amyloidosis (NPA) is rare, typically found incidentally in radiological studies where well-defined bilateral, subpleural and peripheral nodules are shown. These nodules range in size from 0.5 to 15cm and may present calcifications or cavitation.2 They may also show increased uptake on PET-TC. Diagnosis is achieved through histopathological examination that reveals homogeneous eosinophilic amorphous material with red-green birefringence under cross polarized light with Congo red stanning.1,2 Given its radiological resemblance to malignant lung tumors, histological confirmation is essential. NPA has a benign course and rarely requires treatment.2
(A) Thoracic CT in axial plane showing some of the multiple nodules with different sizes, calcification and cyst in both lungs. (B) PET-CT in axial planes showing the bilateral nodules with varying degrees of 18F-fluoro-deoxyglucose uptake. (C) Histological findings of pulmonary nodules resected: hematoxylin–eosin staining shows well-circumscribed eosinophilic nodule with acellular amorphous material, accompanied by lymphocytes, plasma cells and granulomatous reaction (H&E 20×). (D) Congo red staining reveals nodule with amorphous material exhibiting a salmon-colored appearance and apple-green birefringence under polarized microscopy, suggesting amyloidosis.
This manuscript has been produced without the help of any artificial intelligence software or tool.
Authors’ contributionsM.R.G. developed the manuscript with support from S.V.V.A. and J.G.T. S.V.V.A. performed the histopathological study and provided the histological images. J.G.T. supervised the project. All authors have read and approved the final version of the article.
Informed consentIt is affirmed that the article does not contain any patient data that could compromise confidentiality, violate privacy, or enable patient identification.
The patient provided written informed consent, granting authorization for the utilization of their medical records for educational purposes or the dissemination of scientific knowledge.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestThe authors declare not to have any conflicts of interest that may be considered to influence directly or indirectly the content of the manuscript.