The recent article published in your journal by Jara Chinarro et al.,1 titled “Innovations and Challenges in Intermediate Respiratory Care Units: Toward Effective Integration into the Hospital System”, provides a valuable insight into the impact and challenges faced by Intermediate Respiratory Care Units (IRCUs) in Spain regarding their integration into the hospital system.
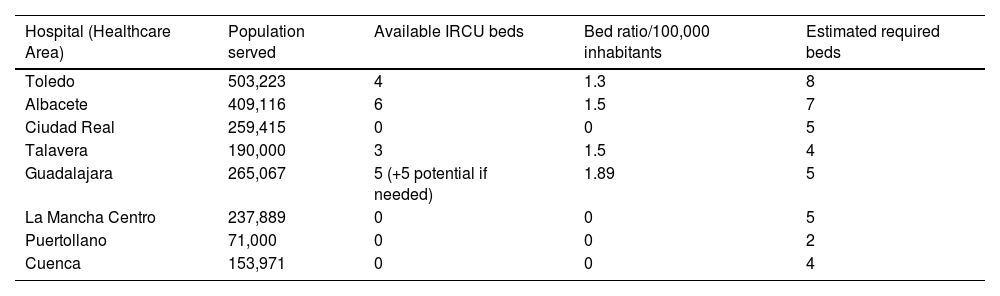
However, we believe that for a comprehensive understanding of the development of IRCUs in the Spanish context, it is crucial to complement the analysis with a regional perspective to adequately evaluate the planning and healthcare needs across different hospitals. In this regard, a Consensus Document was developed by SOCAMPAR (Castilla-La Mancha Society of Pulmonology and Thoracic Surgery) based on a survey conducted among various Pulmonology departments. We revealed significant disparities in the distribution, funding, and consolidation of these units, factors that could notably influence their effectiveness and long-term sustainability. The current situation and the estimated number of required beds were also analyzed (Table 1).
Comparison of IRCU capacity in Castilla-La Mancha.
| Hospital (Healthcare Area) | Population served | Available IRCU beds | Bed ratio/100,000 inhabitants | Estimated required beds |
|---|---|---|---|---|
| Toledo | 503,223 | 4 | 1.3 | 8 |
| Albacete | 409,116 | 6 | 1.5 | 7 |
| Ciudad Real | 259,415 | 0 | 0 | 5 |
| Talavera | 190,000 | 3 | 1.5 | 4 |
| Guadalajara | 265,067 | 5 (+5 potential if needed) | 1.89 | 5 |
| La Mancha Centro | 237,889 | 0 | 0 | 5 |
| Puertollano | 71,000 | 0 | 0 | 2 |
| Cuenca | 153,971 | 0 | 0 | 4 |
Efforts have been made to analyze the post-pandemic reality of IRCUs across Spain, echoing findings from Jara Chinarro et al., which identified marked heterogeneity in IRCU structures and operational models. In Castilla-La Mancha, the situation is even more disparate.
There is no definitive scientific evidence on the recommended number of beds or size of RICUs.2 The 2021 British guidance suggests that “a minimum of 10 beds per 250,000 population would provide sufficient capacity for many, though some will require more”,3 however, the Italian Consensus Document from ITS-AIPO has recently maintained the recommendation of providing 1–2 Respiratory Intermediate Care Unit (RICU) beds per 100,000 inhabitants.4,5 We believe this guideline offers a viable recommendation for our setting, based on the leadership of Italian pulmonology at the European level and a socio-healthcare context similar to our. It has been estimated that a hospital serving a population of approximately 250,000 inhabitants may admit up to 70 COPD exacerbations requiring ventilatory support per year.6 Additionally, patients requiring continuous monitoring, high-flow nasal cannula oxygen therapy, CPAP, or NIV for other causes of acute respiratory failure, including COVID-19 pneumonia, and weaning could increase this number to approximately 120 cases annually.
Reviewing data from the Respiratory Monitoring Unit at Nuestra Señora del Prado University Hospital in Talavera revealed that 50% of patients with respiratory acidosis had COPD. Furthermore, these units should be capable of handling seasonal variations and increased demands during respiratory virus epidemics. Consequently, based on the serviced population, IRCUs should ideally have at least 2 beds per 100,000 inhabitants, allowing flexibility to expand capacity in various healthcare contexts.
As indicated in Table 1, IRCU bed availability per 100,000 inhabitants varies significantly, lacking clear standardization or a strategic plan for equitable expansion. The number of beds required at each center was estimated based on the optimal bed-to-population ratios reported in the literature, particularly in relation to the expected number of admissions for certain pathologies, while also taking into account the specific needs of each department (such as on-call availability, coordination with the ICU, etc.).
This deficit in specific areas underscores the need for a planning model based on objective healthcare criteria rather than isolated administrative decisions.
One of the most significant challenges is the absence of a legislative framework regulating the creation and maintenance of IRCUs in Spain. Despite acknowledgment from scientific societies such as SEPAR or the European Respiratory Society7 and documented clinical and healthcare advantages,8 there is currently no official Spanish or specific European regulation ensuring their stability and funding.
The SOCAMPAR Consensus Document highlights the lack of a homogeneous financial provision model, leading to IRCUs either closing post-pandemic or operating minimally. Additionally, as emphasized by Jara Chinarro et al., the absence of standardized admission and treatment criteria among hospitals and uniform clinical data analysis poses substantial limitations for precise cost and clinical outcome analysis within this healthcare context.
Of note, Salcedo Lobera et al.9 highlights an aspect potentially generalizable to most IRCUs in Spain: a portion of patients exhibit significant frailty due to chronic conditions and age. The appropriateness or proportionality of admission to IRCUs and initiation of non-invasive respiratory support in these cases is debatable. Without clearly defined exclusion criteria, individualized decisions based on baseline health status, cognitive level, and patient comfort are prioritized when initiating therapeutic measures.
Comprehensive multicenter studies analyzing data from various IRCUs across Spain are lacking. Consequently, consolidating IRCUs within the Spanish hospital system requires coordinated efforts among administrators, hospital managers, and scientific societies. This endeavor must be prioritized to guarantee quality care, universality, and equitable patient assistance. Finally, we believe incorporating regional analysis into the article could highlight the importance of equitable planning and the necessity for a robust regulatory framework. Establishing a national development plan for IRCUs with standardized staffing and funding criteria is essential to ensure long-term stability and efficiency.
We appreciate the opportunity to share these findings and hope they contribute constructively to the debate on IRCU planning and sustainability in Spain.
Artificial intelligenceArtificial intelligence technology was not used in the preparation of this manuscript.
FundingThis work has not received any specific support from public sector agencies, the commercial sector, or non-profit organizations.
Authors’ contributionsAll authors have contributed intellectually to the work, meet the requirements for authorship, and have approved the final version.
Conflicts of interestThe authors declare no conflicts of interest.