Determine if patients undergoing elective surgery have risk factors for obstructive sleep apnea syndrome (OSAS), using the Stop-bang questionnaire.
Material and methodsPatients who entered a university hospital for surgery and met the inclusion criteria were asked to be weighed, measure, and answered questions about their sleep habit. They were measured and weighed on a stationary SECA scale with a maximum capacity of 220kg. The neck was measured in inches with a tape measure. The questionnaire was answered and given a risk measured by the same scale, and the data was collected in the capture sheet.
ResultsA power of 80% was used, considering a p-value that registered below 0.05 statistically significant. Data was collected from 222 patients undergoing surgical procedures at a teaching hospital in northeastern México. The average age was 57 years (24–87 years). The body mass index presented an average of 29.6kg/m2. We found that 19.8% of the patients had normal BMI, with 80.2% of the sample being overweight or obese (n=178). As for the circumference of the neck, an average of 16.4in. was recorded.
ConclusionsIt was found that 68% of the sample posed an intermediate or high risk for OSAS, compared to other literature that marked 30%. Also, 80% of the preoperative population was found to be overweight or obese.
Obstructive sleep apnea (OSA) is a common chronic disorder which often requires attention and care all throughout life. Characteristics in adults include obstructive apneas, hypopnea, or respiratory distress, and daytime symptoms attributed to interrupted sleep. OSA is an important disorder because patients have a higher risk of deficient neurocognitive performance, as well as problems in other systems. Untreated severe OSA has been linked to a higher cardiovascular mortality.1 The most important risk factors of OSAS are advanced age, male, obesity, and high blood pressure. Of these, obesity is without a doubt the most significant risk; prevalence increases progressively as body mass index increases (BMI).2 Between the years 1990 and 2010, OSAS prevalence increased for each group age and BMI category, up to 50%.3
This syndrome is characterized by a recurrent functional collapse of the airways during sleep, causing a substantial reduction and, in some cases, a total ceasing of airflow, regardless of any breathing efforts in progress. This leads to periodic perturbations in the exchange of air.4 The collapse or opening of the pharynx during sleep depends on two opposite forces: one is the “dilating” force which tends to keep the pharynx opened through the genioglossi muscles and pulmonary volume. The other is the “collapsing” force which tends to close the pharynx. These include negative intraluminal pressure and the positive extramural pressure which the soft tissues apply.4
Polysomnography is multiple parameters test utilized in the study of sleep. Today, it is the gold standard for the diagnosis of sleep disorders, particularly of obstructive sleep apnea. In fact, most studies nowadays involving polysomnography are for the diagnosis of OSAS.5 Among the detection tools used in OSAS screening are the Stop-bang questionnaire, The Berlin questionnaire and the Sleep Apnea Clinical Score (SACS), to name a few.
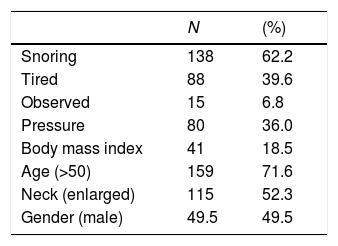
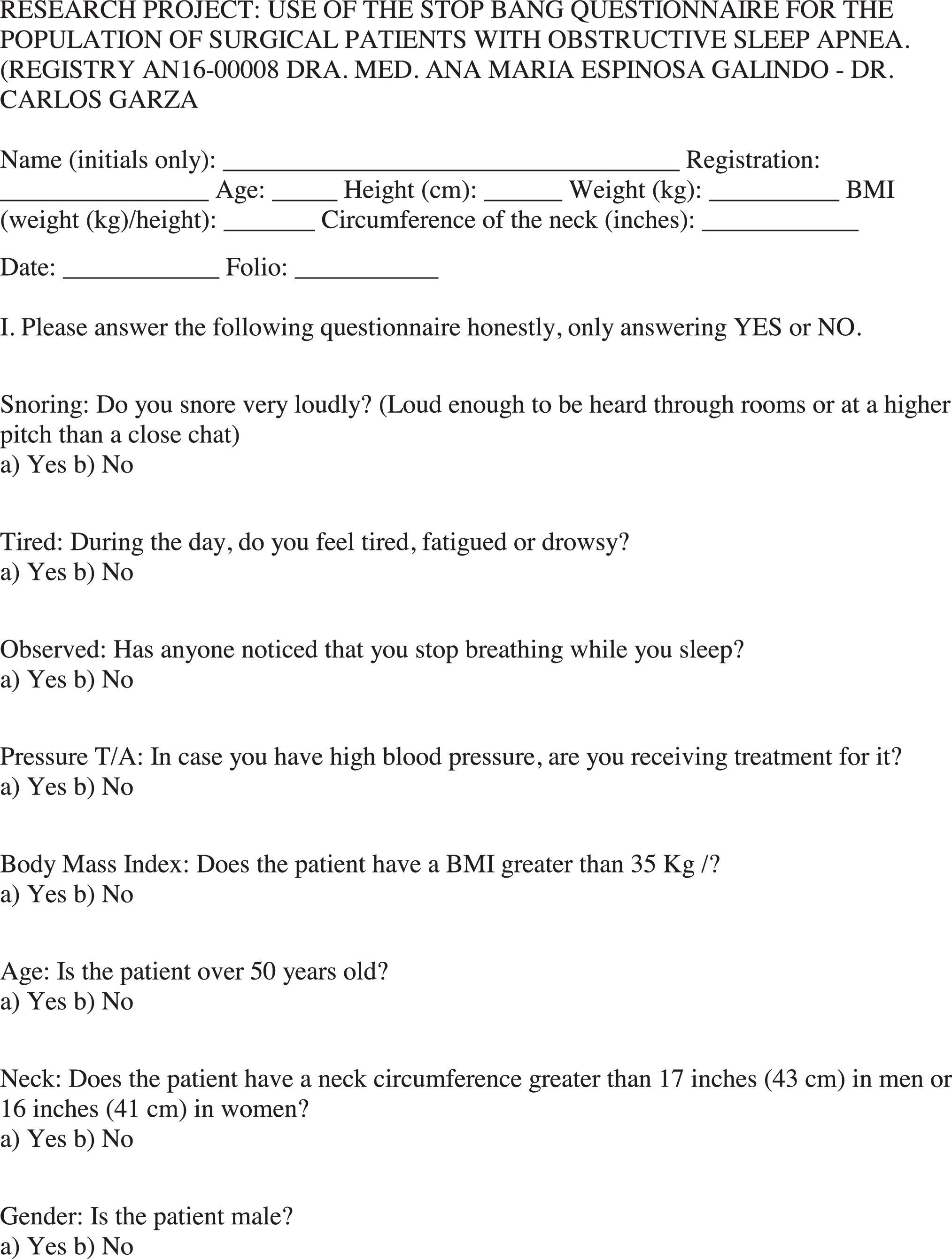
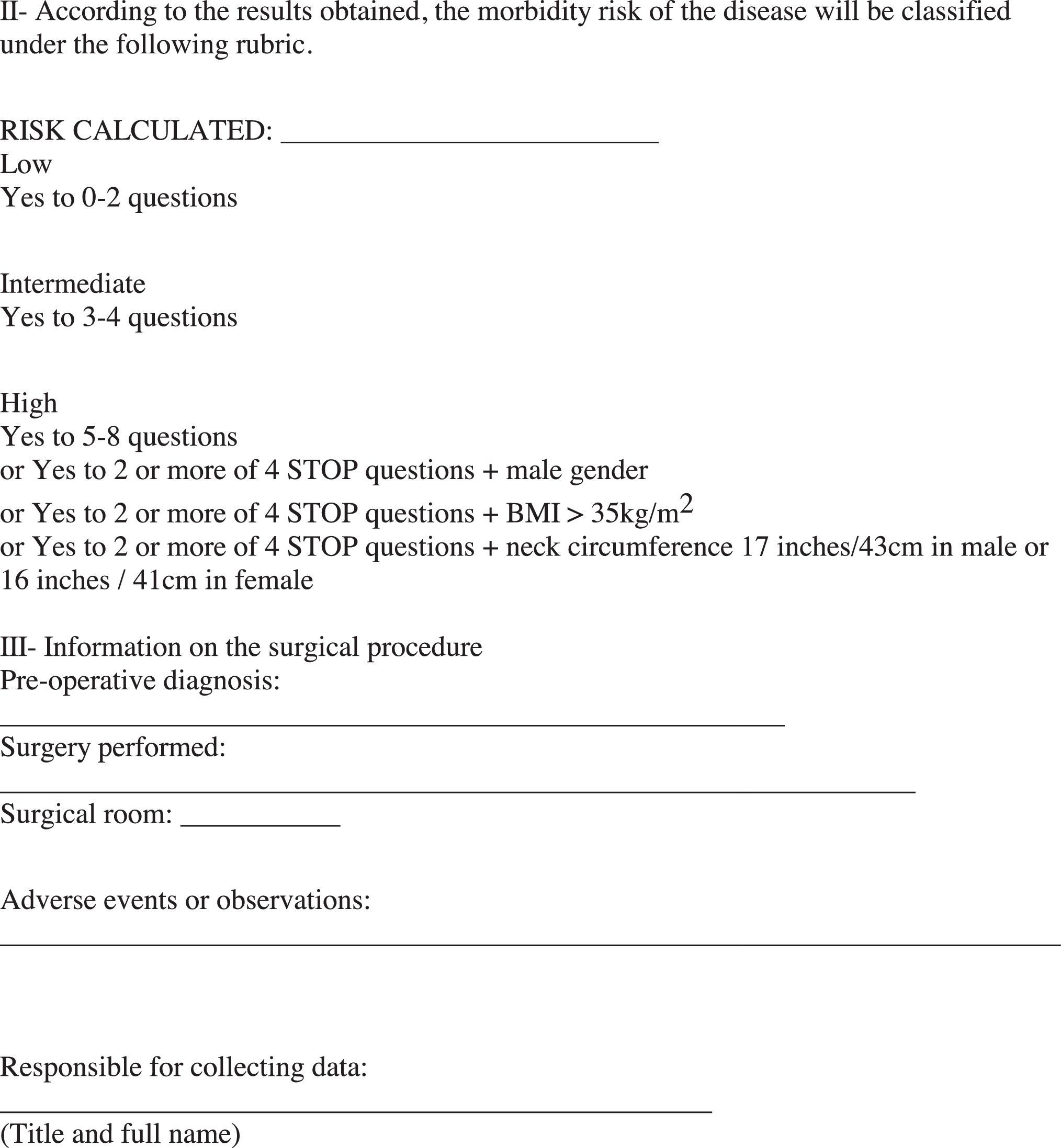
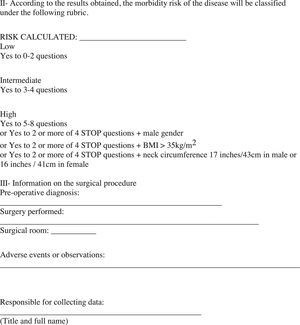
The Stop-bang questionnaire requires “yes” or “no” answers to eight questions about snoring, tiredness, observed apneas and blood pressure, BMI>35kg/m2, age >50 years, and neck circumference >17in. for males and 16in. for females. Even though the Stop-bang questionnaire grants the same score for any question, not all items have the same predictive value for OSAS, and a two-step scoring system may improve performance.5
The potential benefits of successful OSAS treatment include an improvement in the patient's quality of life, improvement in systemic blood pressure, reduction of the use and costs of health attention, and possibly a reduction in cardiovascular morbidity and mortality.6
Materials and methodsWith the previous authorization of the Ethics Committee, a total of 222 patients were studied. Taking into account the following selection criteria; all the patients who were admitted to the pre-surgical area of the university hospital fully conscious and oriented, and who understood the items in the questionnaire. Also being between 40 and 75 years of age, male or female, with AAS I, II or III, regardless of their type of anesthesia. The patients who met all requirements and criteria were asked permission to have their measurements taken and were asked about their sleeping habits. The patients were weighed and measured using a SECA stationary scale with a maximum capacity of 220kg; their necks were measured in inches using a measuring tape. After the questionnaire was conducted, they were given a risk measured by the same scale, and the data was gathered in a form.
Exclusion criteria included disoriented patients, patients with neurological deterioration who did not understand or could not answer the questionnaire, anyone outside of the age range, SAA IV, and patients who were incapable of walking to be weighed.
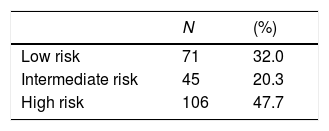
ResultsData were collected from 222 patients, of whom 104 were men and 118 were women, as well as by surgical specialty, General Surgery with 71 patients (32%), Traumatology with 26 patients (12%), Urology with 51 patients (23%), Gynecology with 33 patients (15%), Otolaryngology with 13 patients (6%), Plastic Surgery with 11 patients (5%), Neurosurgery with 12 patients (5%), Ophthalmology with 5 patients (2%).
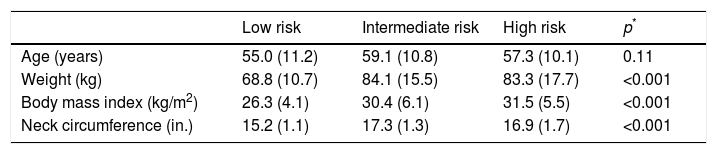
General demographicsThe median age of all the patients was 57 years (24–87 years). The body mass index showed an average of 29.6kg/m2. Regarding the circumference of the neck, an average of 16.4 inches (12.5–21.5) was recorded. The average value of the neck diameter for women in inches was 15.61 inches (±1.33), and in men it was 17.22 (±1.59) p<0.001. 19.8% of the sample had a BMI considered normal, with 80.2% of the sample being overweight or obese (n=178).
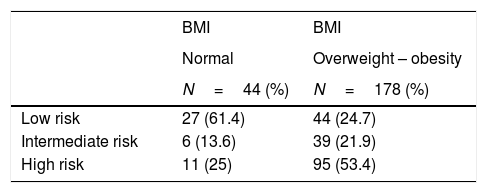
The most relevant results are presented in Tables 1–3.
Demographic variables according to the identifies risk group.
| Low risk | Intermediate risk | High risk | p* | |
|---|---|---|---|---|
| Age (years) | 55.0 (11.2) | 59.1 (10.8) | 57.3 (10.1) | 0.11 |
| Weight (kg) | 68.8 (10.7) | 84.1 (15.5) | 83.3 (17.7) | <0.001 |
| Body mass index (kg/m2) | 26.3 (4.1) | 30.4 (6.1) | 31.5 (5.5) | <0.001 |
| Neck circumference (in.) | 15.2 (1.1) | 17.3 (1.3) | 16.9 (1.7) | <0.001 |
The values indicate median with standard deviation.
In this study, 62.2% of patients admitted snoring loudly, 39.6% felt tired during the daytime, and 36% were receiving treatment for high blood pressure (Table 3).
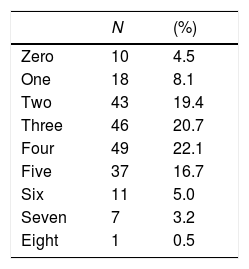
About 22% of all patients had four risk factors for OSAS, 20.7% had three, and 19.4% had two of them; 8.7% of patients had six or more risk factors (Table 4).
Risk stratificationOf all the patients included in the sample, 68% of them were considered at intermediate to high risk (n=151). Of the 47.7% of patients having a high OSAS risk level, 53% of them had either overweight or obesity (Table 5). Most relevant demographic and clinical variables according to OSAS risk group are shown in Table 1.
DiscussionObstructive sleep apnea is a syndrome affecting millions of people, being the most common chronic disease related to sleep. The diagnosis is not always easy since it can go unnoticed or does not get the proper importance. As stated by Frances Chung in his paper on OSAS in pre-surgical patients, over 80% of men and over 90% of women are unaware of having an OSAS diagnosis.7
The simple fact of suffering from OSAS alters the quality of life of the individuals, cognitively as well as in other systems. Not only does it increase the odds of an accident during everyday activities, such as while driving, where estimations suggest that it is between 2 and 10 times more frequent,8 but it also alters other systems, such as the cardiovascular system. Constant apneas and hypercapnia during sleep can result in a constant liberation of catecholamines, leading to hypertense patients without proper control, despite treatment. This deleterious effect is shown in several studies, i.e., the work of Jose M. Marin et al. where they compare the risk of fatal and non-fatal heart events in patients with OSAS, where the events increase in patients with OSAS, especially the untreated ones.6
According to the literature, the number of undiagnosed patients who undergo surgery varies depending on the diagnostic method and the area of population. In this case, we only studied older adults (ages ranging from 50 to 75 years of age). The results suggest that in our hospital, 80% of pre-surgical patients are overweight or obese; additionally, the number of patients with a high risk of OSAS is alarming. This was determined using the Stop-bang questionnaire, without taking into account the fact that in our area, we do not have the CPAP for the recovery of the patient.
We are aware of the fact that the higher the patient's age, the higher the risks of OSAS. Thus explaining the moderate rise in the amount of moderate and high-risk patients; yet, numbers of up to 70% for moderate and high-risk patients exceed these estimations, in comparison to the 28% of other studies. Hypercapnia during sleep can result in a deleterious effect shown in several papers. A good example is in the work of Jose M. Marin et al. where they compare the risk of fatal and non-fatal cardiac events in patients with OSAS, with and without CPAP therapy and controls, and the events increase in patients with OSAS, especially those untreated.6
While OSAS is a disease which affects various systems, it is also true that its treatment helps control many of the same deleterious effects, and significantly decreases the patient's morbidity and mortality. In a study conducted on 240 patients who underwent surgery (with and without OSAS), a higher morbidity rate was observed in those patients with OSAS. Moreover, it was higher amongst those patients who were not previously treated with CPAP. Some of the patients who undergo surgery at our institution receive the benefits of a CPAP therapy prior to surgery.9 Currently, we do not have a pre-surgical pulmonary assessment that has the Stop-bang as a clause, and if we follow the research cycle, to be able to make a clinical practice guide, we will first need several systematic reviews. Moreover, for these, we will need to have several studies that together can show results with statistical significance. We hope that more studies will be done using this tool for screening in pre-surgical patients to be able to make decisions in favor of the patient.
Sixty-eight percent of our sample was found to have a moderate to high risk of OSAS, and none of these patients had CPAP therapy, not even a diagnosis by polysomnography. We hope that this study will help us make a better comprehensive evaluation of the patients in a second study. We could investigate the increased cost of resources in our hospital linked to OSAS, balancing the cost of polysomnography with treatment before surgery and the risk of operating. In a study conducted in the United States in 400 hospitals and 530,000 patients, they compared the use of resources related to sleep apnea, Stavros and colleagues found an increase in the use of resources. Of the 222 patients studied, 21% had a BMI of more than 35kg/m2 (obesity class 2); with the simple fact of obesity. These patients have a high risk of endocrine and cardiovascular morbidity, due to such factors as difficult-to-control hypertension or heart failure,10 without adding the deleterious effect of a constant release of catecholamines in those who have OSAS. In conclusion, we suggest that the use of Stop-bang questionnaire could help if included as a routine in the evaluations of patients before a surgical procedure.
FundingNo financial support was provided.
Conflict of interestNo conflicts of interest to declare.