Technology Enhanced Medical Education International Conference (THEME 2019)
Más datosThis study was aimed to compare the sleep disturbances of patients with Parkinson's disease and those with vascular parkinsonism.
MethodAnalytic study with a case–control approach. Fifteen participants then grouped as Parkinson's disease and vascular parkinsonism and Hoehn and Yahr stage. Sleep disturbances were assessed by Parkinson's Disease Sleep Scale-2 (PDDS-2) and Pittsburgh Sleep Quality Index (PSQI. A t-independent test analyzed data.
ResultAmong 15 samples, 10 of them were Parkinson's disease, and five others were vascular parkinsonism. PDSS-2 for all participants was concluded to have sleep disturbances. The type of sleep disturbances was found consistent in all study groups. PSQI showed a 100% abnormality in both groups. All statistical analyses for PDSS-2 and PSQI between vascular parkinsonism and Parkinson's disease revealed no significant difference except in PSQI results (p=0.015) for the mild stage.
ConclusionThere were no significant differences found in both groups, Parkinson's disease and vascular parkinsonism.
Parkinson's disease, also called primary Parkinsonism, is a part of Parkinsonism, which is pathologically characterized by degeneration of the basal ganglia, especially in the substantia nigra pars compacta and by the presence of eosinophilic cytoplasmic inclusions (Lewy bodies).1–3
Parkinson's disease is one of the most common neurodegenerative diseases in the elderly, with a ratio of men to women 3:2. Parkinson's disease includes more than 80% of parkinsonism. Parkinson's disease has a prevalence of 329 per 100,000 populations, where the average incidence ranges from 16 to 19 per 100,000 people. At the age of 70 years, the prevalence can reach 120, and the incidence rate is 55 cases per 100,000 populations per year. In Indonesia, the incidence of Parkinson's disease is estimated to be ten people each year, and temporary estimates have around 200,000–400,000 patients.1
Vascular Parkinsonism, one type of secondary parkinsonism, is a disorder of involuntary motion post-stroke associated with infarction as well as cerebral hemorrhage. The emergence can be related to symptomatic acute stroke, and can also arise later, or become progressive. Findings regarding European studies are vascular parkinsonism occurs in as many as 3% of all parkinsonism patients, and it is even higher than previously thought.1
Non-motor symptoms as a clinical manifestation of parkinsonism, present in almost all patients with Parkinson's disease and even more often precede the onset of motor symptoms.1,4,5
Subjective and objective examinations can assess sleep disorders. A subjective examination is made by using a questionnaire. From the whole questionnaires, there were three questionnaires recommended to meet the criteria and could be used to evaluate the presence of sleep disorders such as the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and Parkinson Disease Sleep Scale (PDSS).6,7
Until now, there have been no studies specifically describing sleep disorders in Parkinson's disease and secondary parkinsonism associated with the severity of the disease. Understanding the types of sleep disorders, Parkinson's disease, and vascular parkinsonism will lead us to provide appropriate treatment so that morbidity and mortality can be reduced.
This study aims to analyze sleep disorders in Parkinson's disease and vascular parkinsonism, associated with the severity of the disease.
MethodThis research is a pilot study with an analytic method for case-control studies. This study population was all patients with Parkinson's disease and vascular parkinsonism who were outpatient at the Dr. Wahidin Sudirohusodo General Hospital and affiliated hospitals in June 2019. The study sample was total sampling, with whom patients were diagnosed with Parkinson's disease based on Hughes and United Kingdom Parkinson's Disease Brain Bank criteria, and vascular parkinsonism was assessed using a vascular rating scale previously described by Winikates and Jankovic. Patients were included in this study after signing the informed consent document. Based on the inclusion criteria above, 18 samples were collected, but three samples were excluded from the study due to impaired cortical function (MMSE<24) and had a history of the use of sleeping pills.
Therefore, there are 15 samples of total sampling. Sleep disorders are assessed using the Parkinson's Disease Sleep Scale (PDSS-2), and sleep quality are assessed by the Pittsburgh Sleep Quality Index (PSQI). We also determine the degree of progression of the sample using the Scale Hoehn and Yahr (H & Y). The data obtained were importing from Microsoft Excel into Statistical Package for the Social Sciences (SPSS) 22.0 and analyzed using an independent t-test.
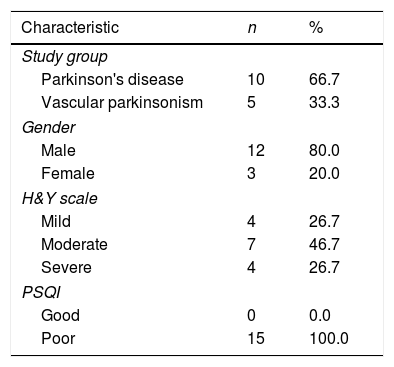
ResultsThis was a study of 15 patients who had a diagnosis of Parkinson's disease and vascular parkinsonism (Table 1), ten patients (66.7%) were diagnosed with Parkinson's Disease and five patients with vascular Parkinsonism (33.3%). Of the total subjects, 12 (80%) patients were male. The most commonly found Parkinsonism stages are medium Stage/Stage 2 H & Y (46.7%). Based on the assessment of sleep quality, the Pittsburgh Sleep Quality Index (PSQI) shows that 100% of the study subjects had poor sleep quality.
Clinical and demography characteristic of study subjects (n=15).
| Characteristic | n | % |
|---|---|---|
| Study group | ||
| Parkinson's disease | 10 | 66.7 |
| Vascular parkinsonism | 5 | 33.3 |
| Gender | ||
| Male | 12 | 80.0 |
| Female | 3 | 20.0 |
| H&Y scale | ||
| Mild | 4 | 26.7 |
| Moderate | 7 | 46.7 |
| Severe | 4 | 26.7 |
| PSQI | ||
| Good | 0 | 0.0 |
| Poor | 15 | 100.0 |
PSQI, Pittsburgh Sleep Quality Index.
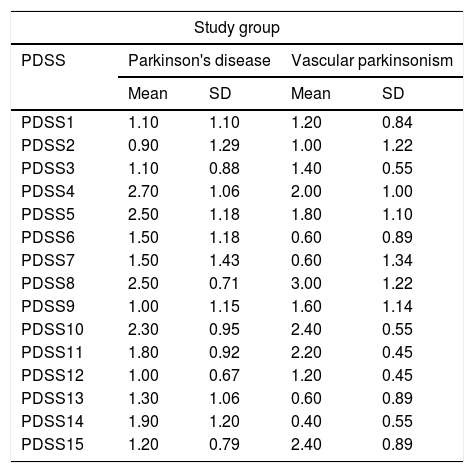
Table 2, individual assessment of sleep disorders based on PDSS-2, shows that the lowest average Parkinson's disease was found in the second item, specifically difficulty in starting night sleep/insomnia (0.90) and the highest average in the fourth item, restless leg syndrome/RLS while in Vascular parkinsonism, the lowest average was found in item 14, which is sleep refreshment (0.40) and the highest in item 8 namely nocturia (3.00).
Individual score for PDSS-2 (n=15).
| Study group | ||||
|---|---|---|---|---|
| PDSS | Parkinson's disease | Vascular parkinsonism | ||
| Mean | SD | Mean | SD | |
| PDSS1 | 1.10 | 1.10 | 1.20 | 0.84 |
| PDSS2 | 0.90 | 1.29 | 1.00 | 1.22 |
| PDSS3 | 1.10 | 0.88 | 1.40 | 0.55 |
| PDSS4 | 2.70 | 1.06 | 2.00 | 1.00 |
| PDSS5 | 2.50 | 1.18 | 1.80 | 1.10 |
| PDSS6 | 1.50 | 1.18 | 0.60 | 0.89 |
| PDSS7 | 1.50 | 1.43 | 0.60 | 1.34 |
| PDSS8 | 2.50 | 0.71 | 3.00 | 1.22 |
| PDSS9 | 1.00 | 1.15 | 1.60 | 1.14 |
| PDSS10 | 2.30 | 0.95 | 2.40 | 0.55 |
| PDSS11 | 1.80 | 0.92 | 2.20 | 0.45 |
| PDSS12 | 1.00 | 0.67 | 1.20 | 0.45 |
| PDSS13 | 1.30 | 1.06 | 0.60 | 0.89 |
| PDSS14 | 1.90 | 1.20 | 0.40 | 0.55 |
| PDSS15 | 1.20 | 0.79 | 2.40 | 0.89 |
PDSS, Parkinson's Disease Sleep Scale.
Sleep disorders are grouped according to sleep disturbances that occur, sleep quality (items 1–3), nocturnal restlessness (items 4 and 5), nocturnal psychosis (items 6 and 7), nocturia (item 8), nocturnal motor symptoms (items 9–13), and daytime somnolence (items 14 and 15). It shows the highest mean value on Nocturnal Motor Symptoms for both groups with a mean for the Parkinson's disease group 7.4, and vascular parkinsonism is 8. The lowest mean for Parkinson's disease is nocturia (2.5), whereas vascular parkinsonism is nocturnal psychosis (Fig. 1).1,2
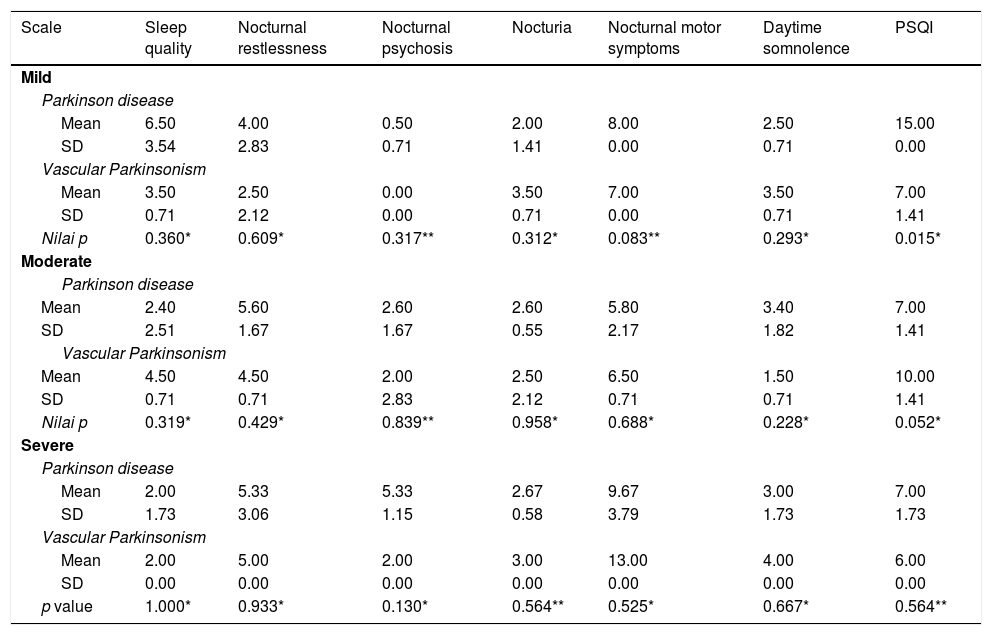
Types of sleep disorders shown in Table 3, from the highest to the lowest, both in Parkinson's disease and in vascular parkinsonism. At the lowest (mild) level of disease both for Parkinson's disease and vascular parkinsonism, sleep disorders with the lowest average value are nocturnal psychosis, and the highest is nocturnal motor symptoms. For moderate degrees of disease, Parkinson's disease has the lowest average value for impaired sleep quality, insomnia, and sleep duration, while the highest mean value was found in nocturnal motor symptoms. Whereas for the same degree of vascular parkinsonism, the lowest average value was obtained at daytime somnolence and the highest in nocturnal motor symptoms. Furthermore, for the degree of severe illness, Parkinson's disease shows the lowest mean values of impaired sleep quality, insomnia and sleep duration, and the highest values in nocturnal motor symptoms. Meanwhile, vascular parkinsonism in the same degree showed the lowest mean scores for sleep quality, insomnia, sleep duration, and nocturnal psychosis, while the highest values were found in nocturnal motor symptoms (Fig. 1). Statistical tests gave insignificant results except for the PSQI value of Parkinson's disease and mild grade vascular parkinsonism (p=0.015), where these results showed that there were statistically significant differences between the PSQI value of Parkinson's disease and mild grade vascular parkinsonism. Statistical analysis for other parameters gives a value of p>0.05 with the result that concluded. It does not provide a statistically significant difference.
Types of Sleep Disturbance based on PDSS-2 and PSQI in both Parkinson and Vascular Parkinsonism based on the severity of disease (n=15).
| Scale | Sleep quality | Nocturnal restlessness | Nocturnal psychosis | Nocturia | Nocturnal motor symptoms | Daytime somnolence | PSQI |
|---|---|---|---|---|---|---|---|
| Mild | |||||||
| Parkinson disease | |||||||
| Mean | 6.50 | 4.00 | 0.50 | 2.00 | 8.00 | 2.50 | 15.00 |
| SD | 3.54 | 2.83 | 0.71 | 1.41 | 0.00 | 0.71 | 0.00 |
| Vascular Parkinsonism | |||||||
| Mean | 3.50 | 2.50 | 0.00 | 3.50 | 7.00 | 3.50 | 7.00 |
| SD | 0.71 | 2.12 | 0.00 | 0.71 | 0.00 | 0.71 | 1.41 |
| Nilai p | 0.360* | 0.609* | 0.317** | 0.312* | 0.083** | 0.293* | 0.015* |
| Moderate | |||||||
| Parkinson disease | |||||||
| Mean | 2.40 | 5.60 | 2.60 | 2.60 | 5.80 | 3.40 | 7.00 |
| SD | 2.51 | 1.67 | 1.67 | 0.55 | 2.17 | 1.82 | 1.41 |
| Vascular Parkinsonism | |||||||
| Mean | 4.50 | 4.50 | 2.00 | 2.50 | 6.50 | 1.50 | 10.00 |
| SD | 0.71 | 0.71 | 2.83 | 2.12 | 0.71 | 0.71 | 1.41 |
| Nilai p | 0.319* | 0.429* | 0.839** | 0.958* | 0.688* | 0.228* | 0.052* |
| Severe | |||||||
| Parkinson disease | |||||||
| Mean | 2.00 | 5.33 | 5.33 | 2.67 | 9.67 | 3.00 | 7.00 |
| SD | 1.73 | 3.06 | 1.15 | 0.58 | 3.79 | 1.73 | 1.73 |
| Vascular Parkinsonism | |||||||
| Mean | 2.00 | 5.00 | 2.00 | 3.00 | 13.00 | 4.00 | 6.00 |
| SD | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| p value | 1.000* | 0.933* | 0.130* | 0.564** | 0.525* | 0.667* | 0.564** |
Sleep disorders commonly occur in Parkinson's disease patients; two-thirds of Parkinson's patient's populations are reported to suffering from sleep disorders. Insomnia and waking up at night, are types of sleep disorders.8 One study reported that the number of sleep disorders in Parkinson's disease reached 96%.9 It is confirmed with the results of a study conducted, where 100% of the samples were proven to have sleep disorders based on Parkinson's Disease Sleep Scale-2 (PDSS-2). PDSS-2 is a screening tool that is useful to screen for sleep disorders in Parkinson's disease, but not for diagnosing.6
PDSS-2 is an assessment used for sleep evaluation in Parkinson's patient's sleep disorder. Sleep disorders in Parkinson's disease are mostly caused by nocturnal motor symptoms (Fig. 1), where motoric symptoms of tremors are more common in patients with vascular parkinsonism than in Parkinson's disease.10 It is what might be the underlying differences in the value of PDSS-2 in both groups.
Based on Table 3, it was found that nocturnal motor symptoms dominate the causes of sleep disorders in both Parkinson's disease and vascular parkinsonism (mild, moderate, and severe degree). Nocturnal motor symptoms consist of several types, including nocturnal akinesia, cramps, nocturnal akathisia, dystonia, restless leg syndrome (RLS), periodic movements of limbs (PMS) and psychomotor agitation. Of all the nocturnal motor symptoms that can be found in Parkinson's disease patients, nocturnal akinesia is the most frequent. This condition is mainly found in patients who take dopamine agonists or quick-acting carbidopa or levodopa. Although other motor symptoms such as resting tremor and rigidity will experience improvement during sleep, this does not apply to nocturnal akinesia. The causes of these nocturnal motor symptoms are caused by the progressive depletion of dopamine in the mesencephalon. This condition then causes sleep disturbances in Parkinson's patients.11
Despite Table 3 also shown the causes of sleep disorders that are predominantly least commonly found in Parkinson's disease and vascular parkinsonism are nocturnal psychosis, both mild, moderate, and severe. Further studies discussion regarding nocturnal psychosis in Parkinson's disease are still uncommon. Nonetheless, the results of the current study are supported by several other studies showing a low incidence of nocturnal psychosis in Parkinson's disease. A study evaluating 165 Parkinson patients for two years showed that only six patients were identified had experienced sleepwalking. Another study also showed that only 10 of 93 Parkinson patients had the same complaint. Nocturnal psychosis complaints are more common in children, but the incidence is increasing in adults with neurological disorders.12
The statistical analysis shown in Table 3 shows that in general, there were no significant differences in sleep disturbances between Parkinson's disease and vascular parkinsonism. It is supported by a 2014 research which showed that there were no differences in PDSS values in patients with Parkinson's disease or vascular parkinsonism.13 It is likely to occur because the symptoms found in patients with Parkinson's disease can also be found in patients with vascular parkinsonism, as a result of the effect on quality sleep is also not much different.
Furthermore, the mean PSQI for mild degrees in Parkinson's disease was found to be higher than in vascular parkinsonism with p=0.015, indicating that the difference was statistically significant. This result has shown that the sleep quality of patients with a mild degree of Parkinson's disease is worse than those with vascular parkinsonism for the same degree. Other studies using PDSS in distinguishing the quality of sleep in Parkinson's patients and vascular parkinsonism did not actually show a significant difference. However, no other study has accurately assessed PSQI scores for cases of vascular parkinsonism, so that the difference in PSQI values in the current study is still possible due to a lack of the number of samples.
ConclusionThere were no statistically significant differences in the sleep disturbances between the Parkinson's disease group and the vascular parkinsonism group. Nevertheless, there were differences in sleep quality between the Parkinson's disease group and the vascular parkinsonism group in the severity of the disease.
Conflict of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the Technology Enhanced Medical Education International Conference (THEME 2019). Full-text and the content of it is under responsibility of authors of the article.