Cancer continues to be one of the leading causes of morbidity and mortality in the world, with approximately 18.1 million new cases in 2018. Population estimates indicate that the number of new cases will increase in the next two decades to 29.5 million a year in 2040. In addition, each year there are more than 9.5 million deaths from cancer in the world, with this disease being the first cause of death in men, and the second in women.1 As in most western countries, cancer in Spain is currently one of the most relevant health problems in terms of public health. It is estimated that the number of new cancer cases diagnosed in Spain in 2020 will reach 277,394 cases (160,198 will be in men), according to the latest estimates from the Spanish Cancer Registry Network (REDECAN).2
Due to the COVID-19 pandemic this year, the operation of our healthcare system has changed dramatically in a matter of days. On 23rd April, the Ministry of Health reported more than 219,000 confirmed cases of SARS-CoV-2 virus infection and more than 22,500 deaths due to the associated COVID-19 disease (https://covid19.isciii.es/). The profound reorganization that healthcare has undergone in order to care for the sick and the measures adopted to stop the occurrence of new cases are affecting routine practice in oncology, with potential medium and long-term consequences for cancer patients. Therefore, the objective of this article is to give a global vision of the implications of the pandemic on cancer in Spain.
Cancer patients: a risk group in the COVID-19 pandemicMost people diagnosed with cancer are elderly (65 or older) and have one or more comorbidities, which increases the risk of complications from COVID-19.3 In addition, cancer and cancer-related treatments commonly cause immunosuppression, and therefore it is believed that cancer patients will be more susceptible to severe SARS-CoV-2 virus infections and to developing COVID-19.4 For these reasons, cancer patients are considered one of the high-risk groups in the current pandemic.
Available data are still limited, but suspicions about the role of cancer in COVID-19 are confirmed in the first studies from China.5,6 In a meta-analysis based on 11 articles, it is estimated that around 2% (95% CI: 2.0-3.0%) of patients with COVID-19 in China had cancer.7 Furthermore, early analyses suggest that cancer patients are at increased risk for serious events, such as ICU admission, mechanical ventilation, or death, and experience a more rapid progression of the disease.5 The risk of these fatal outcomes has also been observed to be higher in patients who have recently received chemotherapy and surgery.5,8 In Italy, reviewing the medical records of a sample of 355 patients who died of COVID-19 revealed that 20% were undergoing treatment for cancer.9
It remains to be seen if these results are confirmed in Spain. It should be noted that, for the time being, significant differences have been observed among the countries involved, in terms of incidence and mortality,9 Furthermore, the studies mentioned are based on a small number (e.g., 20–30 patients) of cancer patients, with different types of cancer and very heterogeneous treatments. Some authors note that in previous epidemics of other types of coronavirus (e.g., SARS and MERS), no increased risk of severe disease was observed in patients with immunosuppression.10 All this indicates that the evidence must be interpreted with caution and that it is early to draw valid conclusions. However, in these exceptional circumstances, the mere suspicion of vulnerability to COVID-19 has been enough for experts to take steps to protect cancer patients.
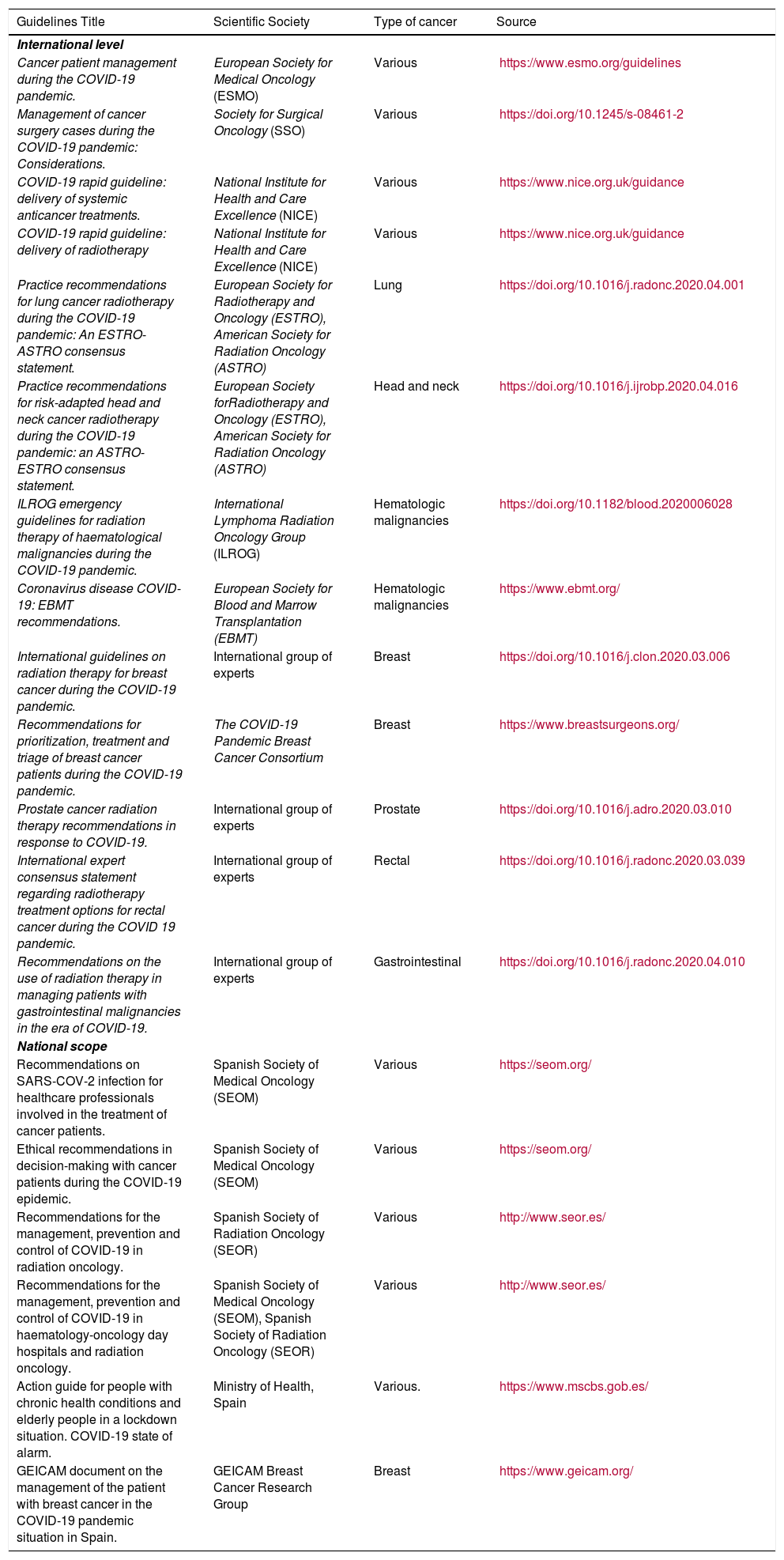
Measures taken to protect cancer patientsGuidelines on how to modify clinical practice during the COVID-19 epidemic have been published by various scientific societies and expert groups (Table 1). The European Society for Medical Oncology (ESMO)11), the Spanish Society of Medical Oncology (SEOM12) and the Spanish Society of Radiation Oncology (SEOR)13 have published recommendations on how to modify healthcare and/or treatment protocols to minimize risks in cancer patients.
Some international and national guidelines of interest to professionals on the treatment and care of cancer patients during the COVID-19 pandemic.
| Guidelines Title | Scientific Society | Type of cancer | Source |
|---|---|---|---|
| International level | |||
| Cancer patient management during the COVID-19 pandemic. | European Society for Medical Oncology (ESMO) | Various | https://www.esmo.org/guidelines |
| Management of cancer surgery cases during the COVID-19 pandemic: Considerations. | Society for Surgical Oncology (SSO) | Various | https://doi.org/10.1245/s-08461-2 |
| COVID-19 rapid guideline: delivery of systemic anticancer treatments. | National Institute for Health and Care Excellence (NICE) | Various | https://www.nice.org.uk/guidance |
| COVID-19 rapid guideline: delivery of radiotherapy | National Institute for Health and Care Excellence (NICE) | Various | https://www.nice.org.uk/guidance |
| Practice recommendations for lung cancer radiotherapy during the COVID-19 pandemic: An ESTRO-ASTRO consensus statement. | European Society for Radiotherapy and Oncology (ESTRO), American Society for Radiation Oncology (ASTRO) | Lung | https://doi.org/10.1016/j.radonc.2020.04.001 |
| Practice recommendations for risk-adapted head and neck cancer radiotherapy during the COVID-19 pandemic: an ASTRO-ESTRO consensus statement. | European Society forRadiotherapy and Oncology (ESTRO), American Society for Radiation Oncology (ASTRO) | Head and neck | https://doi.org/10.1016/j.ijrobp.2020.04.016 |
| ILROG emergency guidelines for radiation therapy of haematological malignancies during the COVID-19 pandemic. | International Lymphoma Radiation Oncology Group (ILROG) | Hematologic malignancies | https://doi.org/10.1182/blood.2020006028 |
| Coronavirus disease COVID-19: EBMT recommendations. | European Society for Blood and Marrow Transplantation (EBMT) | Hematologic malignancies | https://www.ebmt.org/ |
| International guidelines on radiation therapy for breast cancer during the COVID-19 pandemic. | International group of experts | Breast | https://doi.org/10.1016/j.clon.2020.03.006 |
| Recommendations for prioritization, treatment and triage of breast cancer patients during the COVID-19 pandemic. | The COVID-19 Pandemic Breast Cancer Consortium | Breast | https://www.breastsurgeons.org/ |
| Prostate cancer radiation therapy recommendations in response to COVID-19. | International group of experts | Prostate | https://doi.org/10.1016/j.adro.2020.03.010 |
| International expert consensus statement regarding radiotherapy treatment options for rectal cancer during the COVID 19 pandemic. | International group of experts | Rectal | https://doi.org/10.1016/j.radonc.2020.03.039 |
| Recommendations on the use of radiation therapy in managing patients with gastrointestinal malignancies in the era of COVID-19. | International group of experts | Gastrointestinal | https://doi.org/10.1016/j.radonc.2020.04.010 |
| National scope | |||
| Recommendations on SARS-COV-2 infection for healthcare professionals involved in the treatment of cancer patients. | Spanish Society of Medical Oncology (SEOM) | Various | https://seom.org/ |
| Ethical recommendations in decision-making with cancer patients during the COVID-19 epidemic. | Spanish Society of Medical Oncology (SEOM) | Various | https://seom.org/ |
| Recommendations for the management, prevention and control of COVID-19 in radiation oncology. | Spanish Society of Radiation Oncology (SEOR) | Various | http://www.seor.es/ |
| Recommendations for the management, prevention and control of COVID-19 in haematology-oncology day hospitals and radiation oncology. | Spanish Society of Medical Oncology (SEOM), Spanish Society of Radiation Oncology (SEOR) | Various | http://www.seor.es/ |
| Action guide for people with chronic health conditions and elderly people in a lockdown situation. COVID-19 state of alarm. | Ministry of Health, Spain | Various. | https://www.mscbs.gob.es/ |
| GEICAM document on the management of the patient with breast cancer in the COVID-19 pandemic situation in Spain. | GEICAM Breast Cancer Research Group | Breast | https://www.geicam.org/ |
The measures include various procedures to reduce the risk of infection, such as using personal protective equipment, reducing visits to hospitals and health centres, postponing non-essential visits, implementing telemedicine services, and educating patients on hygiene measures. Furthermore, the ESMO guidelines for cancer patients recommends complete isolation: not leaving your home at all and isolating yourself from family members who have contact with the outside world.14
Other measures include the possibility of delaying cancer treatments, modifying the dose and fractionation schedules in the case of radiotherapy or reducing the dose of some immunosuppressant treatments, as long as these modifications do not pose a risk to patients. To help make these decisions, ESMO has established three priority categories (high, medium or low), based on the current situation of the cancer patient and the potential implications of changes or delays in treatments for the prognosis of their disease.11
For example, for low or medium priority levels, it is advisable to consider the watchful waiting strategy in the case of cancers diagnosed at an early stage, whose treatment could be deferred for up to 8 or 12 weeks, without this significantly affecting patient outcomes.4,11 However, for treatments that are considered high priority (those that have a significant benefit in terms of survival time or quality of life) and whose delay could mean the loss of this benefit, no changes are proposed in treatment plans.4,11
The decision on possible delays or modifications in treatment will, in many cases, be complex, since it will have to be taken quickly and in exceptional circumstances of maximum uncertainty, always communicating with patients to assess the risk-benefit balance in the individual situation of each patient. Within the framework of the doctor-patient relationship, the SEOM Bioethics Section has also issued some ethical recommendations to help professionals make decisions with their cancer patients during the COVID-19 epidemic.15
Open questions about the impact of the pandemic on cancerThe impact of the pandemic on cancer in Spain could be multifactorial, and we will fully understand it once we have data available on healthcare and patient outcomes. First of all, we should evaluate its direct effect on cancer patients. For example, does having cancer increase the risk of SARS-CoV-2 infection or the risk of developing COVID-19? What are the clinical variables that worsen the prognosis of infected cancer patients? Could the infection or its treatment, especially in severe cases, affect cancer progression?
Aside from immunosuppression vulnerability, unavoidable hospital visits could increase the risk of infection6 due to the shortage of protective medical equipment and frequent contact with medical personnel. For example, according to the results of a survey in Italy, in the areas most affected by COVID-19, a large percentage (38-51%) of oncologists have been reassigned to emergency departments or COVID-19.16 For hospitals in our country where the same has had to be done, this would mean either an increased risk of infection for cancer patients due to contact with the professionals involved, or fewer oncologists available to treat and monitor cancer cases.
This last possibility leads us to consider the indirect effects of the pandemic on cancer, which could be manifold. The deployment of the health system to fight the virus, the high percentage of infected health personnel and the general postponement of appointments and non-urgent procedures, means that, despite all the effort, unintended delays in the diagnosis and treatment of cancer could occur. These delays may be due both to changes in the way the health system operates and to decisions made by the patients themselves. For fear of the virus, patients may prefer to avoid visits to health centres, especially for symptoms perceived as less urgent, as are many of the symptoms of cancer. Similar effects of the pandemic have been documented in acute coronary syndromes17 and the Spanish Society of Cardiology has already warned about the reduced number of health care consultations by patients and the reduced number of interventional procedures performed during the pandemic.
Greater delays in diagnosis and treatment would imply an increase in the number of cases diagnosed in later stages, with the implications on survival, quality of life and economic costs that this entails. Temporary suspension of screening programs will likely contribute to this increase.
Also, the pandemic could adversely affect the mental health of cancer patients. Cancer diagnosis already poses a high risk for psychological disorders, such as anxiety, depression, or adjustment disorders.18 Prolonged isolation and added uncertainty could have negative effects on the psychological well-being of the most vulnerable patients.
It is probable that we will observe several negative effects of the pandemic, but it is also possible that some of the modifications introduced, such as the general use of telemedicine, will prove to be very useful and will remain common in clinical practice.4,19
As a scientific community, we should take action to understand and address the effects of the pandemic on cancer, through epidemiological studies and (new or ongoing) multidisciplinary and collaborative national and international research projects.20 Within this framework, the Carlos III Health Institute has announced an outstanding call for research projects on COVID-19, to which 24 million euros have been assigned. At national level, the National Center for Epidemiology, in collaboration with the Spanish Network of Cancer Registries (REDECAN) are in a unique position to estimate the impact of the pandemic on the epidemiological indicators of cancer in Spain and in each of the different autonomous communities.
Considerations on cancer researchThe pandemic could also affect the development of ongoing clinical trials. In the case of the treatment that is administered within a clinical trial, SEOM recommends following the protocol, using the possibilities of delaying or adjusting the doses and reminds us of “the obligation of the researcher to make the most appropriate decisions for health and patient safety at all times".12 The Spanish Agency of Medicines and Medical Devices (AEMPS) recommends considering interrupting the recruitment of new patients for trials involving treatment with immunosuppressants,21 which suggests that several clinical trials in the field of cancer have been discontinued. In addition, general changes in health care, such as the change to telemedicine and the shortage of personnel and medical equipment, would also affect the protocols of some clinical trials,19 with implications for its success and the validity of the derived results.
Finally, we would have to consider the economic implications of the pandemic. Compared to other leading European countries in cancer research, which increased their spending on R + D+i (Research, development and innovation) and after the last economic crisis, Spain currently spends even less (∼286 euros/inhabitant per year) than it did in 2007.22 The first report on cancer research and innovation in Spain indicates that, due to this previous crisis, cancer research in Spain had already suffered a significant loss of research talent and a worsening of some cancer research and innovation indicators.22
Predictions of a new and more serious economic crisis and the possible diversion of part of the spending on R + D+i towards new infectious diseases, such as COVID-19, indicate that we could expect a significant reduction in the public funds available for cancer research. In addition to the public sector, philanthropic foundations, such as the Spanish Association against Cancer, have been another driving force behind the research.22 However, they are also likely to experience cuts: Cancer Research UK, the largest cancer research charity, has already announced that it expects to loose 20–25% of its income next year due to the pandemic.23
The positive fact that we must hold on to is that cancer researchers in Spain have always done "much with little": despite having half (or less) the expenditure of other European countries, their scientific production has been comparable and even better in some indicators.22 Cancer will continue to be one of the most important health, social and economic problems and, therefore, a priority for our country.
ConclusionAlthough the data is still sparse, the first available studies confirm the suspicion of increased vulnerability to COVID-19 in cancer patients, confirming the need for extraordinary measures taken by various Scientific Societies to protect cancer patients. The pandemic will have a multifactorial effect on cancer in our country, since it could transform clinical practice, influence patient clinical outcomes, complicate clinical trials and have an impact on the budget available for cancer research. Once the most serious crisis and state of alarm is behind us, we should focus on understanding and addressing the direct and indirect effects of the pandemic on clinical practice and cancer patient outcomes.
FundingWithout funding.
Conflict of interestsThe authors declare no conflict of interest.
We wish to thank Dr. Eloisa Bayo-Lozano and Dr. David Vicente Baz, from the Radiation Oncology and Medical Oncology Departments of the Virgen Macarena University Hospital in Seville, for their contributions and valuable comments.
Please cite this article as: Petrova D, Pérez-Gómez B, Pollán M, Sánchez M-J. Implicaciones de la pandemia por COVID-19 sobre el cáncer en España. Med Clin (Barc). 2020;155:263–266.