The aim of this article is to summarize published information on systemic infective complications of tattoos to gain an update of the current picture.
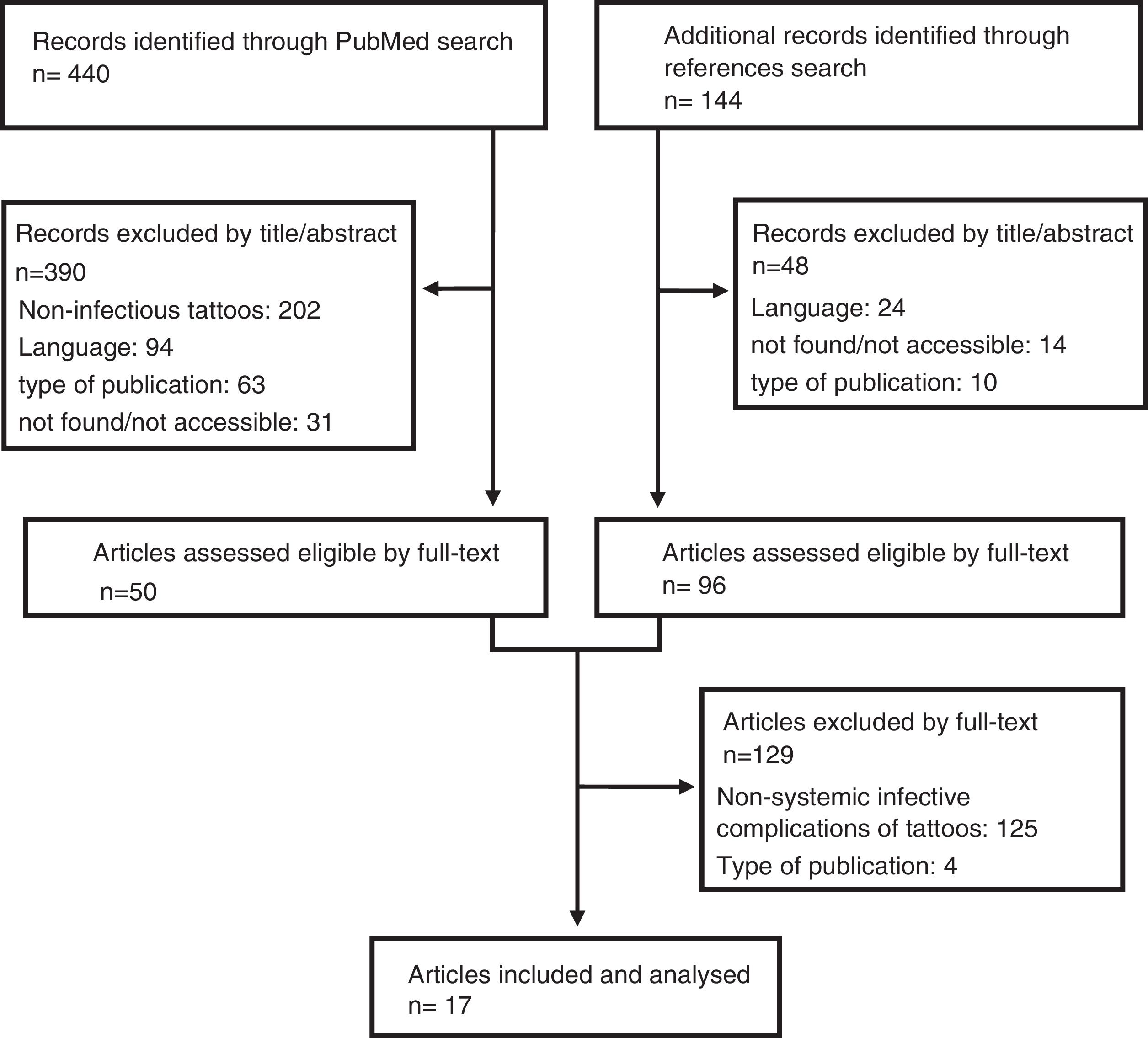
MethodsA literature search was performed in PubMed database (2009–2019), and compared with a search without year restriction. Eligibility criteria were studies on systemic tattoo-related infections, including case reports, case series, outbreak investigations, reviews, and systematic reviews.
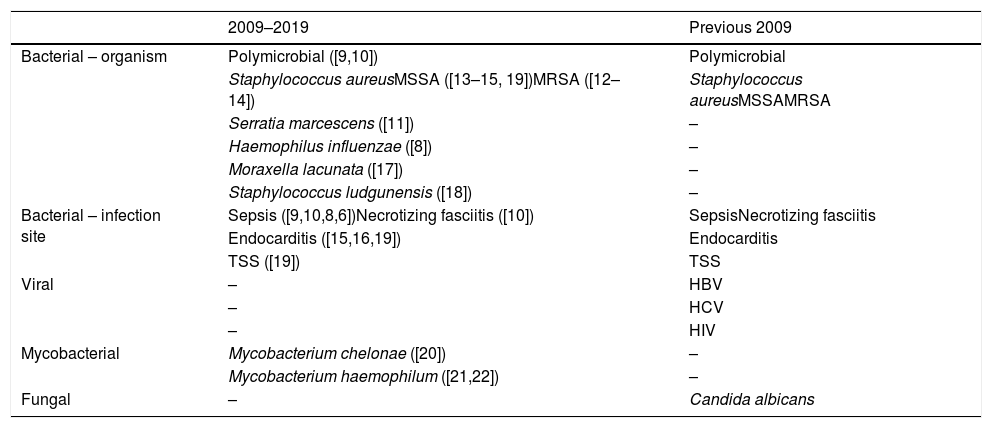
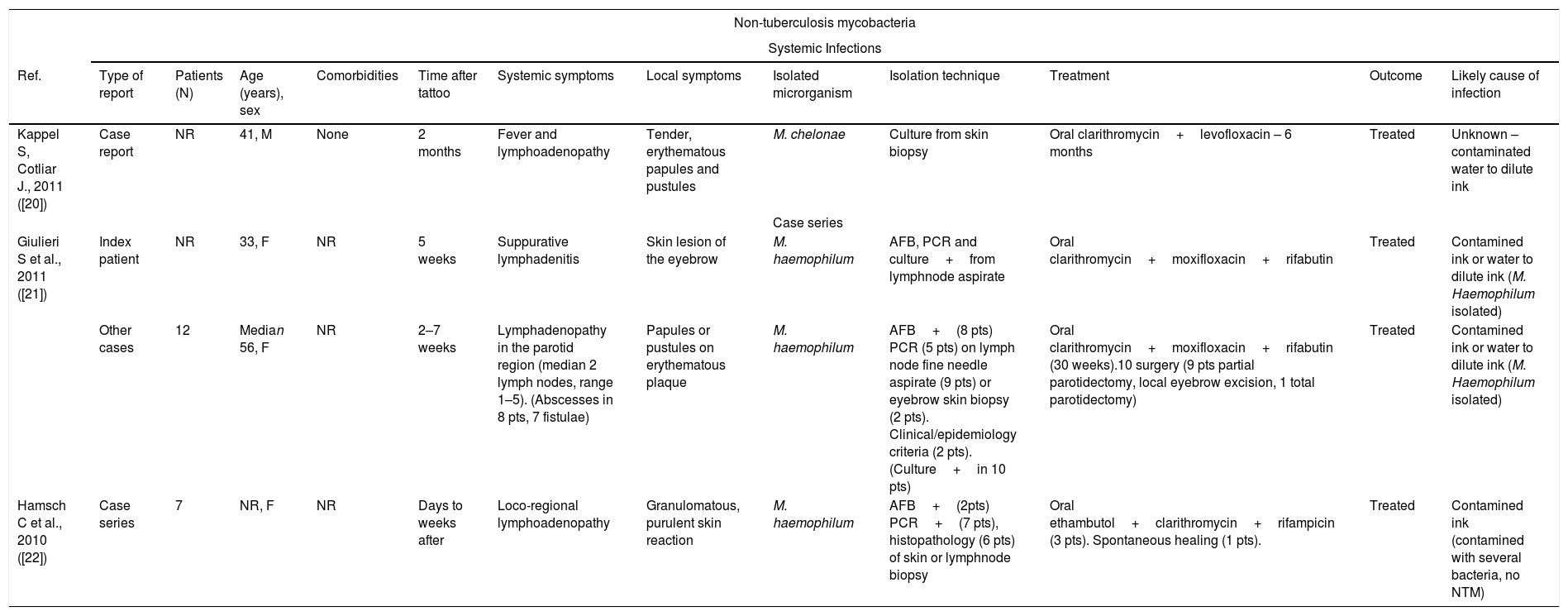
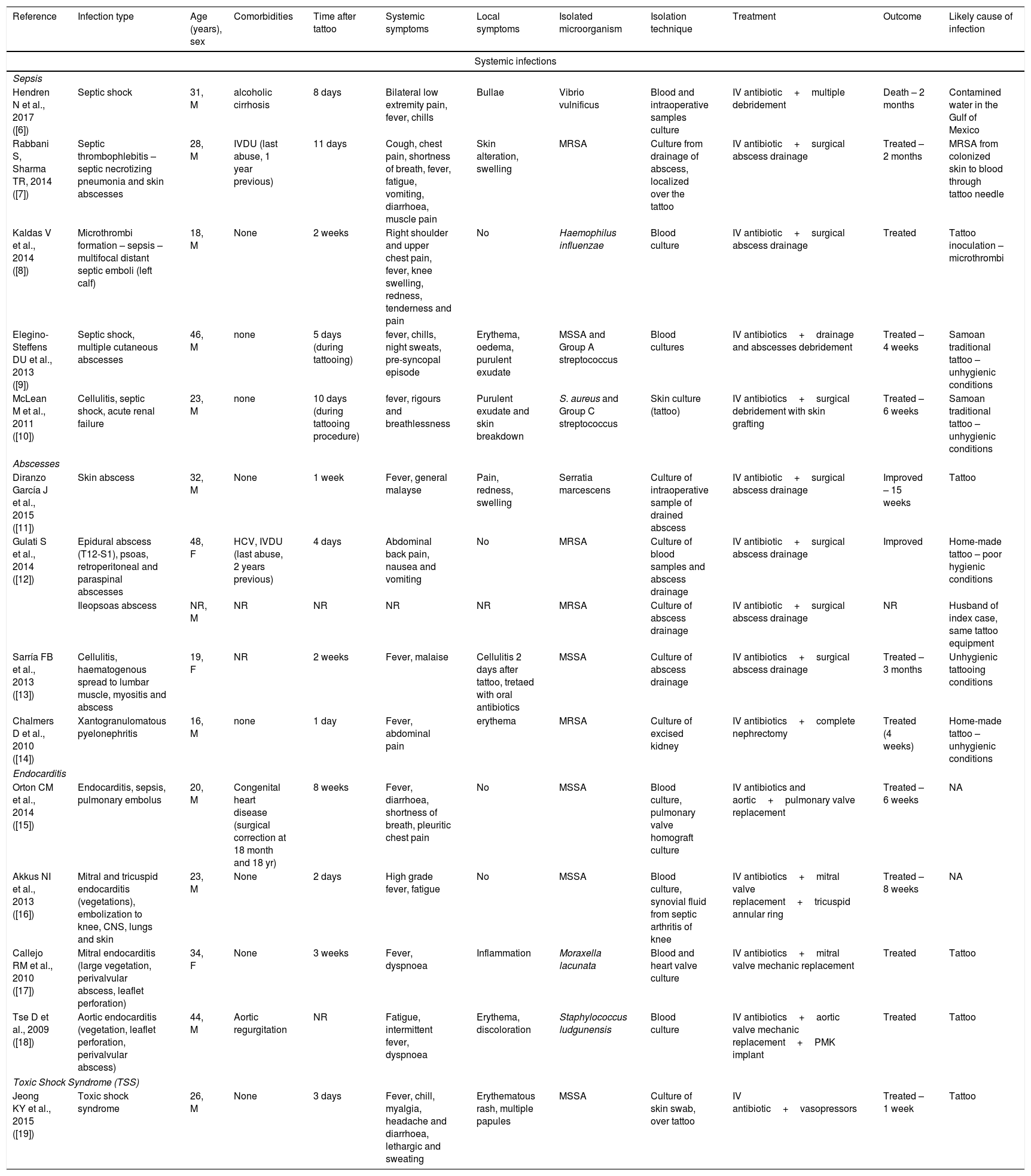
ResultsWe identified 17 manuscripts with systemic infections between 2009 and 2019, with one reported fatality. In contrast to the historical records, no reports of systemic tuberculosis, syphilis or viral (hepatitis or HIV) infections were reported within the study period. A few sporadic cases or Mycobacterium leprae (India) or regional lymphadenopathy associated with skin lesions in non-tuberculosis mycobacteria were identified. Persistent fever with rigour was common in bacterial bloodstream infections. One episode of staphylococcal toxic shock syndrome and several episodes of septic shock were reported, associated with cellulitis or necrotizing fasciitis within two weeks of the procedure, predominantly caused by pyogenic bacteria (S. aureus or streptococcus). Identification of lung or systemic embolisms in the absence of local symptoms, was indicative of (right or left) infective endocarditis.
ConclusionsBacterial bloodstream infections should be considered in subjects developing fever and rigour after tattoos, regardless of local symptoms. A shift in causative organisms has been documented, when comparing with historical reports. NTM are emerging organisms causing lymphadenopathy. Strict hygiene conditions are essential when performing a tattoo.
El objetivo de este artículo es resumir la información publicada sobre las complicaciones infecciosas sistémicas de los tatuajes para tener una actualización de la situación actual.
MétodosSe realizó una búsqueda de literatura en la base de datos PubMed (2009-2019), que se comparó con una búsqueda sin restricción de año. Los criterios de elegibilidad fueron estudios sobre infecciones sistémicas relacionadas con tatuajes, incluidos informes de casos, series de casos, investigaciones de brotes, revisiones y revisiones sistemáticas.
ResultadosSe identificaron 17 manuscritos con infecciones sistémicas entre 2009 y 2019, y se informó de una muerte. A diferencia de los registros históricos, no se notificaron informes de tuberculosis sistémica, sífilis ni infecciones viíricas (hepatitis o VIH) durante el período de estudio. Se identificaron algunos casos esporádicos de Mycobacterium leprae (India) o de linfadenopatías regionales asociadas con lesiones cutáneas en micobacterias no tuberculosas. La fiebre persistente con escalofríos era común en las infecciones bacterianas del torrente sanguíneo. Se informó un episodio de síndrome de choque tóxico estafilocócico y varios episodios de choque séptico, asociados con celulitis o fascitis necrosante dentro de las 2 semanas posteriores al procedimiento, predominantemente causada por bacterias piógenas (S. aureus o estreptococo). La identificación de embolias pulmonares o sistémicas en ausencia de síntomas locales fue indicativa de endocarditis infecciosa (derecha o izquierda).
ConclusionesLas infecciones bacterianas deben considerarse en sujetos que desarrollen fiebre y escalofríos después de los tatuajes, independientemente de los síntomas locales. Se ha documentado un cambio en los organismos causales y las micobacterias no tuberculosas constituyen organismos emergentes. Las condiciones higiénicas adecuadas son fundamentales a la hora de realizar un tatuaje.