Sporadic primary hyperparathyroidism (pHPT) with normal parathormone (PTH) levels is an uncommon disorder. While normocalcemic and hypercalcemic states with elevated PTH levels are well recognized, less is known about this condition. Herein, we present our experience in pHPT with normal PTH levels.
We performed a retrospective review of 70 consecutive parathyroidectomy. Selected patients were those who presented all PTH levels within the laboratory's normal range meeting other biochemical parameters such as elevated serum and urine calcium and normal PTH related peptide (PTHrp). We analyzed the following data: age, symptoms, serum PTH, calcium, 25-hydroxy vitamin D (25(OH)D) and phosphorus levels, preoperative localization studies, single gland disease, histopathological features and follow up. Patients were considered symptomatic if presenting typical symptoms: urolithiasis, osteoporosis with bone pain, neurological disorders, or cardiovascular diseases. Curation was defined as normalization of calcium serum levels.
Applying the criteria described, we have identified two patients (2.9%) with all determinations of serum PTH values in normal range out of 70 patients with diagnosis of sporadic pHPT.
A 71 y-o woman with calcic renal lithiasis which have required lithotripsy. The patient presented in the last 5 years, with an elevation of calcium and corrected calcium for serum albumin [12.3mg/dL (normal value (NV): 8.5–10.5mg/dL)]. Laboratory test also showed a normal 25(OH)D level [45ng/mL (NV 10–55ng/mL)], low level of phosphorus [2mg/dL (NV 2.5–5mg/dL)]. The PTH value was 55pg/mL (NV 25–120ng/mL). All image tests were negative.
Bilateral cervical examination was done revealing an adenoma.
The second case is a 61 y-o man with a 10-year hypercalcemia [11.5mg/dL (NV: 8.5–10.5mg/dL)]. Blood test showed normal phosphorus [3.1mg/dL (NV: 2.5–5mg/dL)], 25(OH)D [16ng/dL (NV: 10–55ng/mL)] and PTH levels [53pg/mL (NV: 25–120ng/mL) and normal PTH related peptide (NV<14pg/mL)]. US did not identify the adenoma, but the MIBI identified a right inferior gland hyper-uptake. Surgical intervention was decided, intraoperatively a real-time 99mTC sestamibi scintigraphy with mini-gamma camera was done with adenoma identification.
The pathological report confirmed the presence of a parathyroid adenoma in both cases. During follow-up, both presented a normalization of calcium values, and a lower level of PTH (21 and 12pg/mL respectively).
Sporadic primary hyperparathyroidism is the most common cause of hypercalcemia and should be considered in any person with an elevated serum calcium level. The finding of hypercalcemia on routine biochemical testing is typically the initial clue to the diagnosis of primary hyperparathyroidism.1 The total serum calcium level, adjusted for the level of albumin, and PTH is mandatory for diagnosis. An elevated (or non-suppressed) level of PTH simultaneous with an elevated calcium level generally indicates a diagnosis of primary hyperparathyroidism.
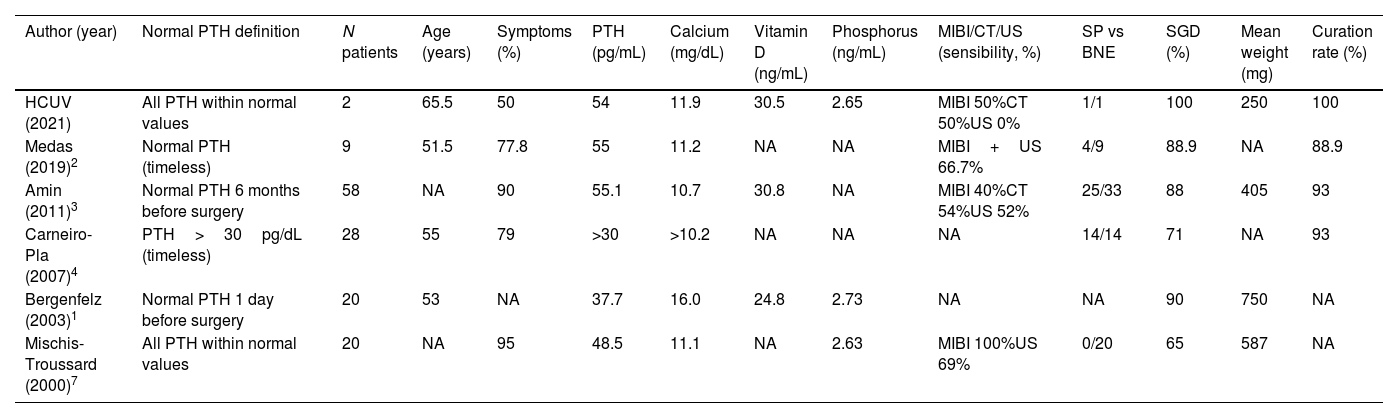
However, it has been seen than up to 20% of patients with sporadic pHPT have a normal PTH level, usually in the context of other documented elevated PTH levels, but less common with only normal PTH levels in the course of the disease.3 There are very few studies in the literature and all with limited numerical samples and ill-defined criteria for pHPT with normal PTH level term (Table 1).1–5
Demographic, preoperative data, surgical procedure and results.
| Author (year) | Normal PTH definition | N patients | Age (years) | Symptoms (%) | PTH (pg/mL) | Calcium (mg/dL) | Vitamin D (ng/mL) | Phosphorus (ng/mL) | MIBI/CT/US (sensibility, %) | SP vs BNE | SGD (%) | Mean weight (mg) | Curation rate (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HCUV (2021) | All PTH within normal values | 2 | 65.5 | 50 | 54 | 11.9 | 30.5 | 2.65 | MIBI 50%CT 50%US 0% | 1/1 | 100 | 250 | 100 |
| Medas (2019)2 | Normal PTH (timeless) | 9 | 51.5 | 77.8 | 55 | 11.2 | NA | NA | MIBI+US 66.7% | 4/9 | 88.9 | NA | 88.9 |
| Amin (2011)3 | Normal PTH 6 months before surgery | 58 | NA | 90 | 55.1 | 10.7 | 30.8 | NA | MIBI 40%CT 54%US 52% | 25/33 | 88 | 405 | 93 |
| Carneiro-Pla (2007)4 | PTH>30pg/dL (timeless) | 28 | 55 | 79 | >30 | >10.2 | NA | NA | NA | 14/14 | 71 | NA | 93 |
| Bergenfelz (2003)1 | Normal PTH 1 day before surgery | 20 | 53 | NA | 37.7 | 16.0 | 24.8 | 2.73 | NA | NA | 90 | 750 | NA |
| Mischis-Troussard (2000)7 | All PTH within normal values | 20 | NA | 95 | 48.5 | 11.1 | NA | 2.63 | MIBI 100%US 69% | 0/20 | 65 | 587 | NA |
HCUV: Hospital Clínico Universitario de Valencia; MIBI: 99mTc-Sestamibi scan; CT: computed tomography; US: ultrasound; SP: selective parathyroidectomy; BNE: bilateral neck exploration; SGD: single-gland disease; NA: not available.
Less than 200 cases of hypercalcemia and normal PTH levels due to parathyroid adenoma have been reported in the literature, most of them as clinical cases or short reports, and only 6 studies have investigated this uncommon pathology, being the cohort of Amin et al.5 with 58 pHPT patients the largest series in the literature to date.
The definition and criteria for pHPT with normal PTH is not clear, as shown in Table 1, some studies defined it as normal PTH the day before surgery, and other as all normal PTH values.
In our series, following the criteria of pHPT with all normal PTH values we have identified 2 cases, but if we identify patients who have some normal PTH values during the study of pHPT the number rises to 7 cases (10%).
Patients trend to be younger but equally symptomatic compared with classic pHPT. Blood test could just show a hypercalcemia, with normal 25(OH)D and preserved renal function. Image tests have demonstrated similar or lower sensibility in pathological gland location. Treatment is parathyroidectomy but surgeons should be aware that adenomas trend to be smaller, and 10–35% of cases could present a multi-gland disease representing a challenge for endocrine surgeons.
Ethical approvalAll procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee.
Informed consentInformed consent of all patients was obtained prior to surgery, but according to our local ethic committee specific formal consent for this study was not required.
FundingThis study has not been supported by any fund.
Conflict of interestDr. Lapeña, Dr. Alfonso and Dr. Cassinello declare that they have no confict of interest.