Hepatic steatosis, also known as non-alcoholic fatty liver (NAFL), is the most frequent liver disease in obese children. Due to an increase in infantile obesity, it is experiencing a significant increment in incidence. Our objectives are: estimate the prevalence of NAFL in children with excess weight and obesity using the glutamate pyruvate transaminase (GPT) value as a biochemical test and an abdominal ultrasound, and correlate the presence of hepatic steatosis with various anthropometric and biochemical parameters.
Patients and methodCross-sectional prevalence study which includes children with excess weight and obesity between the ages of 5 and 15 years, between the years 2004 and 2012. The independent variables included were: age, sex, weight, size, body mass index (BMI), waist circumference (WC), waist size index (WSI), insulinemia, Homeostasis model assessment-insulin resistance (HOMA-R), total cholesterol, triglycerides (TG), high density lipoproteins (HDL), low density lipoproteins (LDL), glutamic-oxaloacetic transaminase (GOT), GPT and gamma-glutamyl transpeptidase (GGT).
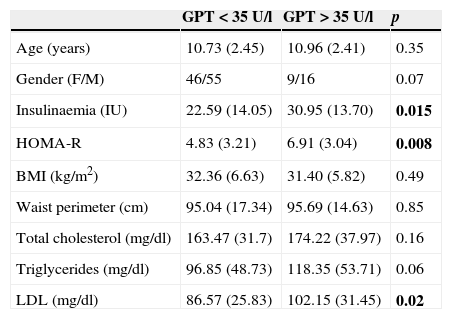
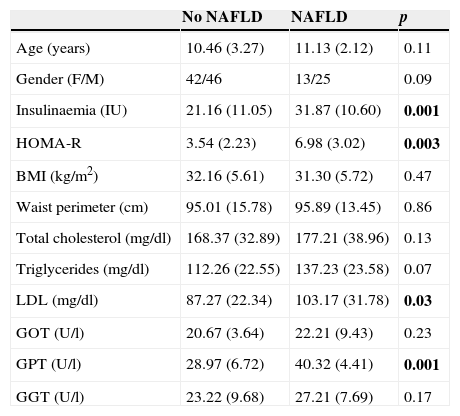
ResultsOne hundred and twenty-six patients, with an average age of 11.94 (3.12) years were recruited. A percentage of 19.66 of the patients presented elevated GPT pathology. Of the 126 abdominal ultrasounds performed, 38 patients presented hepatic steatosis (30.15%). The levels of insulinemia, HOMA-R and LDL were significantly higher in patients with altered GPT, compared to those with normal GPT values (P=.015, P=.008 and P=.002, respectively). The patients with an objective HGNA in ultrasound, also showed greater levels of insulinemia, WC, WSI, total cholesterol, TG, LDL, GLT, GPT and GGT than the patients with normal ultrasounds, thereby achieving statistical significance in insulinemia, HOMA-R, LDL and GPT values.
ConclusionsNAFL is a relatively frequent disorder in obese children and adolescents. In our study, 2 of 10 children – using GPT – and 3 of every 10 – using abdominal ultrasound – present the same. The biochemical marker which best defines it is an elevation in GPT. A modification in lifestyle which includes weight loss as a principal means of avoiding complications in adult life, is essential and necessary.
La esteatosis hepática, también denominada hígado graso no alcohólico (HGNA), es la enfermedad hepática más frecuente en niños obesos y está sufriendo un incremento importante en su incidencia debido al aumento de la obesidad infantil. Los objetivos de nuestro trabajo son: estimar la prevalencia de HGNA en niños con sobrepeso y obesidad utilizando el valor de la glutamate pyruvate transaminase (GPT, «transaminasa glutámico-pirúvica») y la ecografía abdominal, así como correlacionar la presencia de HGNA con distintos parámetros antropométricos y bioquímicos.
Pacientes y métodoEstudio transversal de prevalencia que incluye pacientes con sobrepeso y obesidad, con edades entre 5 y 15 años, reclutados entre 2004-2012. Las variables independientes incluidas fueron: edad, sexo, peso, talla, índice de masa corporal, perímetro de cintura (PC), índice cintura-talla (ICT), insulinemia, Homeostasis model assessment-insulin resistance (HOMA-R), colesterol total, triglicéridos (TG), high density lipoproteins (HDL, «lipoproteínas de alta densidad»), low density lipoproteins (LDL, «lipoproteínas de baja densidad»), glutamic-oxaloacetic transaminase (GOT, «transaminasa glutámico-oxalacética»), GPT y gamma glutamil transpeptidasa (GGT).
ResultadosSe seleccionaron 126 pacientes, con una edad media (DE) de 11,94 (3,12) años. El 19,66% presentó elevación patológica de GPT. Treinta y ocho pacientes (30,15%) presentaron esteatosis hepática utilizando la ecografía abdominal. Los valores de insulinemia, HOMA-R y LDL fueron significativamente mayores en pacientes con alteración de GPT (p=0,015, p=0,008 y p=0,002, respectivamente). Los pacientes con HGNA observado en ecografía también mostraron mayores valores de insulinemia, PC, ICT, colesterol total, TG, LDL, GOT, GPT y GGT que los pacientes con ecografía normal, alcanzándose la significación estadística en valor de insulinemia, HOMA, LDL y GPT.
ConclusionesLa esteatosis hepática es un trastorno relativamente frecuente en niños y jóvenes con obesidad. Dos de cada 10 niños –utilizando GPT– y 3 de cada 10 –utilizando la ecografía abdominal– la presentan, y el marcador bioquímico que mejor la define es una elevación de la GPT. Es imprescindible y necesaria una modificación en el estilo de vida que incluya la pérdida de peso como medida principal para evitar complicaciones en la vida adulta.