The management of patients with atrial fibrillation (AF) after an intracerebral haemorrhage (ICH) is controversial. We analysed the cumulative rates of ICH, ischaemic stroke (IS) and mortality in a cohort of patients with ICH + AF and compared them according to the treatment chosen.
MethodsRetrospective single-centre study of patients with ICH + FA. Patients were classified into two groups: "no anticoagulation restart" (non-AR) and "anticoagulation restart" (AR). The primary endpoint was the cumulative rate of ICH, IS, any intra/extracranial bleeding (AB), any ischaemic or haemorrhagic episode (AE) or death during 2 years of follow-up.
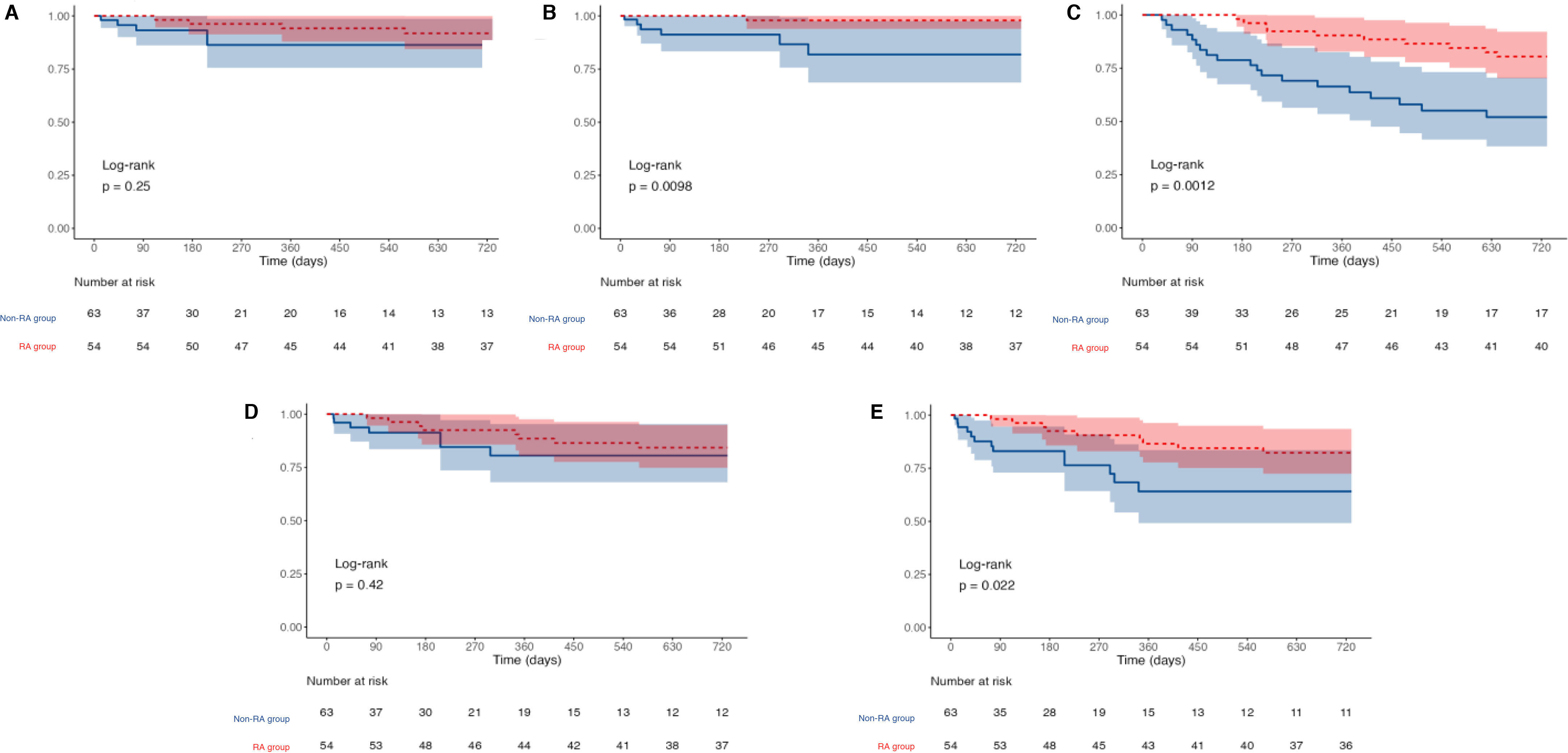
Results117 patients included, non-AR group: 63 patients (53.8%), AR: 54 (46.5%). Mean age 79.4 years (SD 7.9), 73 males (62.4%). No significant differences in baseline characteristics were observed between the 2 groups. Mortality (30 days after ICH) was 31.8% and higher in non-AR vs AR group: 48% vs 19.5% (p = 0.001). The cumulative ICH rate was 10.9% and AB 18%, with no difference between AR and non-AR. The IS rate was 8.3%, higher in the non-AR group (18.1 vs 2.1%, p = 0.010). The AE rate was 25.4% and higher in the non-RA group (35.9% vs. 17.7%, p = 0.022). Non-AR was an independent factor for increased risk of death (HR 5.38 (95%CI 2.30−12.56) and AE: HR 6.16 (1.87−20.25).
ConclusionsPatients with ICH + FA are at an increased risk of death or IS or new ICHs. AR does not increase the risk of rebleeding while non-AR is associated with an increased risk of IS and death.
El tratamiento de pacientes con fibrilación auricular (FA) tras una hemorragia intracraneal (HIC) es controvertido. Analizamos las tasas acumuladas de HIC, ictus isquémicos (IS) y mortalidad de una cohorte de pacientes con HIC + FA, y las comparamos según el tratamiento elegido.
MétodosEstudio unicéntrico retrospectivo de pacientes con HIC + FA. Los pacientes se clasificaron en dos grupos: “no reinicio de anticoagulación” (No-RA) y “reinicio de anticoagulación” (RA). El objetivo principal fue la tasa acumulada de HIC, IS, cualquier sangrado intra/extracraneal (CS), cualquier episodio isquémico o hemorrágico (CE) o muerte durante 2 años de seguimiento.
Resultados117 pacientes incluidos, grupo No-RA: 63 pacientes (53,8%), RA: 54 (46,5%). Edad media 79,4 años (DE 7,9), 73 varones (62,4%). No se observaron diferencias significativas en las características basales entre los 2 grupos. La mortalidad (pasados 30 días de la HIC) fue 31,8% y mayor en grupo no-RA vs RA: 48% vs 19,5% (p = 0,001). Las tasas acumuladas de HIC fue 10,9% y de CS 18%, sin diferencias entre RA y no-RA. La tasa de IS fue 8,3%, mayor en el grupo no-RA (18,1 vs 2,1%, p = 0,010). La tasa de CE fue 25,4% y mayor en el grupo no-RA (35,9% vs 17,7%, p = 0,022). No-RA fue factor independiente de mayor riesgo de fallecer (HR 5,38 (IC95% 2,30−12,56) y de sufrir CE: HR 6,16 (1,87−20,25).
ConclusiónLos pacientes con HIC + FA tienen elevado riesgo de fallecer o sufrir IS o nuevas HICs. RA no aumenta el riesgo de nuevos sangrados mientras no-RA asocia mayor riesgo de IS y fallecimiento.