Mental health and well-being are closely related to age. Complete mental health includes psychopathological symptoms (negative mental health) and subjective well-being (positive mental health). The aim was to compare indicators of complete mental health across the lifespan cross-culturally. Method: We tested age trends in measures of resilience, social support and positive and negative mental health, including the subscales depression, anxiety and stress using data from national representative samples from Germany, Russia and the United States (U.S.) ranging in age from 18 to 100 (N=6,303). Results: The effects of age differed in each country. Today's older Germans experienced more positive and less negative mental health whereas today's older Russians experienced less positive and more negative mental health than the younger people. In the U.S., positive mental health was higher among the older adults, but there was no effect of age for negative mental health. Age also had significant linear and curvilinear effects on resilience and social support. Conclusions: The pattern of mental health across the lifespan is clearly dependent on the nation.
La salud mental y el bienestar están relacionados con la edad. La salud mental completa incluye síntomas psicopatológicos (salud mental negativa) y bienestar subjetivo (salud mental positiva). El objetivo es una comparación transcultural de los indicadores de salud mental completa a lo largo de la vida. Método: Hemos probado las tendencias de edad en medidas de resiliencia, apoyo social y salud mental positiva y negativa, incluyendo depresión, ansiedad y estrés, utilizando datos de muestras nacionales representativas de Alemania, Rusia y Estados Unidos con edades entre 18 y 100 años (N=6.303). Resultados: Los efectos de la edad diferían en cada país. Los alemanes mayores experimentaron una salud mental más positiva y menos negativa, mientras que los rusos mayores experimentaron una salud mental menos positiva y más negativa que los jóvenes. En Estados Unidos, la salud mental positiva fue mayor entre los adultos mayores, pero no hubo efectos de la edad para la salud mental negativa. La edad también tuvo efectos lineales y curvilíneos significativos sobre la resiliencia y el apoyo social. Conclusiones: El patrón de salud mental a lo largo de la vida depende claramente de la nación.
The definition of mental health postulates a comprehensive physical, psychological and social well-being rather than the mere absence of disease or psychopathological symptoms (World Health Organization, WHO, 2001). On this basis, research about the positive dimension of mental health has intensified. The number of publications on positive mental health (PMH) and well-being increased exponentially in the last years (e.g. Miret et al., 2015). Two broad theories describe the key components of PMH and the concept of well-being (e.g. Deci & Ryan, 2008). The hedonic tradition comprises the emotional element, i.e. happiness and satisfaction with life while the eudaimonic tradition includes human potential and optimal functioning. As both approaches can be combined, PMH is conceptualized as the reflection of general emotional, psychological and social well-being (Keyes, 2007; Keyes, Shmotkin, & Ryff, 2002). The two-continua model of mental health suggests that mental health and mental illness, or positive and negative mental health (NMH), are two correlated but distinct factors (Huppert & Whittington, 2003; Keyes, 2007; Wang, Zhang, & Wang, 2011; Weich et al., 2011; Westerhof & Keyes, 2010). Accordingly, PMH can be altered or focused in interventions, albeit a psychopathological diagnosis was not present. It is commonly assumed that certain aspects of PMH are associated with greater levels of satisfaction with life and general functioning (Seow et al., 2016). Besides, lower levels of PMH are accompanied by more severe symptoms of depression, anxiety and stress across different cultures (Schönfeld, Brailovskaia, Bieda, Zhang, & Margraf, 2016).
According to the World Health Organization (WHO, 2016), the global population is ageing progressively. Although social support has been shown to be a considerable buffering factor for mental health (e.g., Milner, Krnjacki, Butterworth, & LaMontagne, 2016), research on the effects of ageing is rare. In a study on U.S. veterans, different facets of social support affected mental health of younger and older men differently (Weiner, Monin, Mota, & Pietrzak, 2016). Contrary to the socioemotional selectivity theory (Carstensen, 2006), which assumes increasing mental health and social support along with increasing age, perceived support was only related to mental health among the younger but not among the older persons (Weiner et al., 2016). Resilience has also been found to be beneficial for adaptive functioning across the adult lifespan (Lerner et al., 2012) and to be protective for people aging with disability (Silverman, Molton, Alschuler, Ehde, & Jensen, 2015). However, the effect of age on resilience in a cross-cultural comparison is not yet clearly outlined. In an Australian cohort study, the risk for suicidality was enhanced in midlife, yet, the relation to resilience was significant across the whole lifespan (Liu, Fairweather-Schmidt, Roberts, Burns, & Anstey, 2014). Since research on the effects of age on mental health is based on samples varying in their national affiliation, there is no general consensus. For instance, a study showed lower prevalence of post-traumatic stress disorder among the older-aged and fewer traumatic experiences compared with young and middle-aged adults (Reynolds, Pietrzak, Mackenzie, Chou, & Sareen, 2016). Likewise, in a large Australian population-based survey, perceived mental health increased with age (Happell & Koehn, 2011). Similar pattern has been reported on data from the U.S., where increasing age was associated with higher subjective and psychological well-being (Keyes et al., 2002). From a lifespan perspective, the dual-factor model of mental health was investigated for the first time in a large sample of Dutch adults, where older adults reported to have less psychological symptoms and to have fewer mental illness problems than the younger-aged adults (Westerhof & Keyes, 2010). However, the fact that there were no variations across age in PMH supports the relative independence of the two dimensions. Interestingly, in a large nationally survey from Japan, the course of happiness and life-satisfaction was U-shaped, which could be explained by the more rigid social structures and predestined professional carriers, at the expense of the middle-aged adults (Tiefenbach & Kohlbacher, 2013). Studies from so-called transition countries showed similar results (Lelkes, 2006; Namazie & Sanfey, 2001). People's expectations, value systems and strategies to deal with stress and political changes develop as a function of their generation. Although indicators of mental health and well-being increased with age in most of the aforementioned studies, a European survey based on data from Great Britain reported Mental health across the lifespan: Cross-cultural comparison that women's negative well-being increased and positive well-being decreased while men's positive well-being also decreased but the negative well-being was the highest among midlife and lowest among the oldest (Huppert & Whittington, 2003). Such heterogeneity was also found in Croatia and Romania, where the subjective well-being rather declined across the age groups, which, in this case, might have been due to monetary reasons (Bălţătescu, 2014; Kaliterna & Burusic, 2014). As younger people are more flexible in their opportunities to adapt to economical and social transitions, they might have an advantage compared to older people. Russia likewise showed a U-shaped function of subjective well-being (Uglanova, 2014). This Eastern country, which is recently undergoing essential developments of political systems, might be particularly affected by cohort effects. Moreover, variations in mental state across age might have occurred because of contemporary socioeconomic conditions. Due to economic and political challenges in Eastern countries such as in Russia, the effects of age on mental health might be different than in Western countries. However, based on these inconsistent findings, we question the global validity of the positivity shift in the old age postulated in the socioemotional selectivity theory of Carstensen (2006). The general positive effect of age on mental health might not be applicable around the world.
While each country or study uses its specific set of indicators to assess mental health across the lifespan (see also Steptoe, Deaton, & Stone, 2015), the study's main objective was to compare the effects of age cross-culturally using the same scales measuring PMH, NMH, social support and resilience in Germany, Russia and the U.S. We hypothesized that in a country which experiences substantial political changes, such as Russia, younger people would be in a better mental state than the older. Conversely, analogue to previous studies from Western countries (e.g., Keyes et al., 2002), we expected that the effect of age would be positive in Germany and the U.S. or even inverted-U shaped with a decline at oldest adulthood. This would also be in line with previous research based on national population samples from Europe (Webster, Westerhof, & Bohlmeijer, 2012; Westerhof & Keyes, 2010).
MethodSamples and proceduresData for the present study was drawn from the BOOM (Bochum Optimism and Mental Health) study, which aim was to reveal protective and risk factors for PMH and NMH in cross-cultural terms (Maercker et al., 2015; Margraf & Schneider, 2017). In total, three population-based samples from Germany (N=1,031), Russia (N=2,485), and the U.S. (N=2,787) were used. In total, 6,303 participants completed the survey. Representativeness for the adult residential populations was due to register-assisted census data from 2011 regarding age, gender and education, was assured by systematized sampling procedures. Collection of the data was between November 2012 and February 2014 using the following methods in the German representative sample: face-to-face and online interviews, online survey, and a mixed-method, which introduced to answer the questionnaires either online or via set-top box, i.e. the opportunity to participate through a television and a remote control via a device. In the U.S. and Russia telephone interviews were used. The recruitment of all participants was via telephone and performed by trained professional interviewers from three professional research institutes (CATI; Computer Assisted Telephone Interview). Participants were provided information about the purpose of the study and an assurance of their anonymity in participation, and gave written informed consent in order to participate. Language specific versions of the different instruments were administered using the conventional translation-back-translation method. In case of discrepancies, the procedure was repeated until complete agreement was achieved. All procedures received research and ethics committee approval by the Ethics Committee of the Faculty of Psychology at Ruhr-Universität Bochum.
MeasuresThe commonly used Depression Anxiety and Stress Scales (DASS-21; Lovibond & Lovibond, 1995) were used to assess NMH. The DASS-21 covers a wide range of psychological distress symptoms. Subjects were asked to rate basic symptoms of negative emotional states during the past week on a 4-point Likert scale ranging from 0 (“did not apply to me at all”) to 3 (“applied to me very much or most of the time”). Responses can be averaged across all items for a total item score or three subscales can be constructed with seven items per scale. Psychometric properties are well established in both clinical and non-clinical samples (Crawford & Henry, 2003; Fung, Tsang, Corrigan, Lam, & Cheng, 2007).
To assess PMH, the unidimensional Positive Mental Health Scale (PMH; Lukat, Margraf, Lutz, van der Veld, & Becker, 2016) was used. The PMH-scale is a person-centered instrument consisting of nine non-specific judgments and was developed to measure emotional, psychological and social aspects of well-being. Targeted at general psychological functioning, subjects were ask to indicate their agreement on a 4-point Likert scale ranging from 0 (“do not agree”) to 3 (“agree”). One example is “I am often carefree and in good spirits”. High internal consistency, good retest-reliability as well as good and discriminant validity were confirmed in a series of six studies comprising samples from students, patients and general populations (Lukat et al., 2016).
The shortened Resilience Scale 11 (RS-11; Schumacher, Leppert, Gunzelmann, Strauß, & Brähler, 2005) was developed on the basis of the RS-25 (Wagnild & Young, 1993) and consists of 11 statements, each ranging on a 7-point Likert scale (1=”disagree” to 7=”agree”). Good reliability and validity indices of this version have been approved before (Schumacher et al., 2005). To calculate a total score, the responses are summed up. One example is “I feel that I can handle many things at a time”.
For the assessment of the level of social support the Questionnaire Social Support (F-SozU K-14; Fydrich, Sommer, Tydecks, & Brähler, 2009) was used. It measures individual's subjective experienced and the anticipated support from his social network. On a 5-point Likert scale, participants rated 14 items from 1 (“not at all true”) to 5 (“very true”), i.e., “I can easily find someone who will look after my apartment when I am not there”.
Statistical analysesWe calculated absolute frequencies for categorical variables as well as means and standard deviations for continuous variables. Polynomial regression models were then conducted to investigate the predictive value of age in association to PMH, resilience, social support, NMH and the domain-specific subscales depression, anxiety and stress as dependent variables. In sum, seven 2-step hierarchical ordinary least square regression analyses were carried out per country. In Model 1, sex and school were used as independent variables, so that they are included as control variables in the second step. In Model 2, age and age-squared were added to reveal linear and curvilinear relationships. Age was centered on the mean in order to counteract collinearity with age-squared. Curve estimation procedures were illustrated in scatterplots by using trends in the age by mental health relationship.
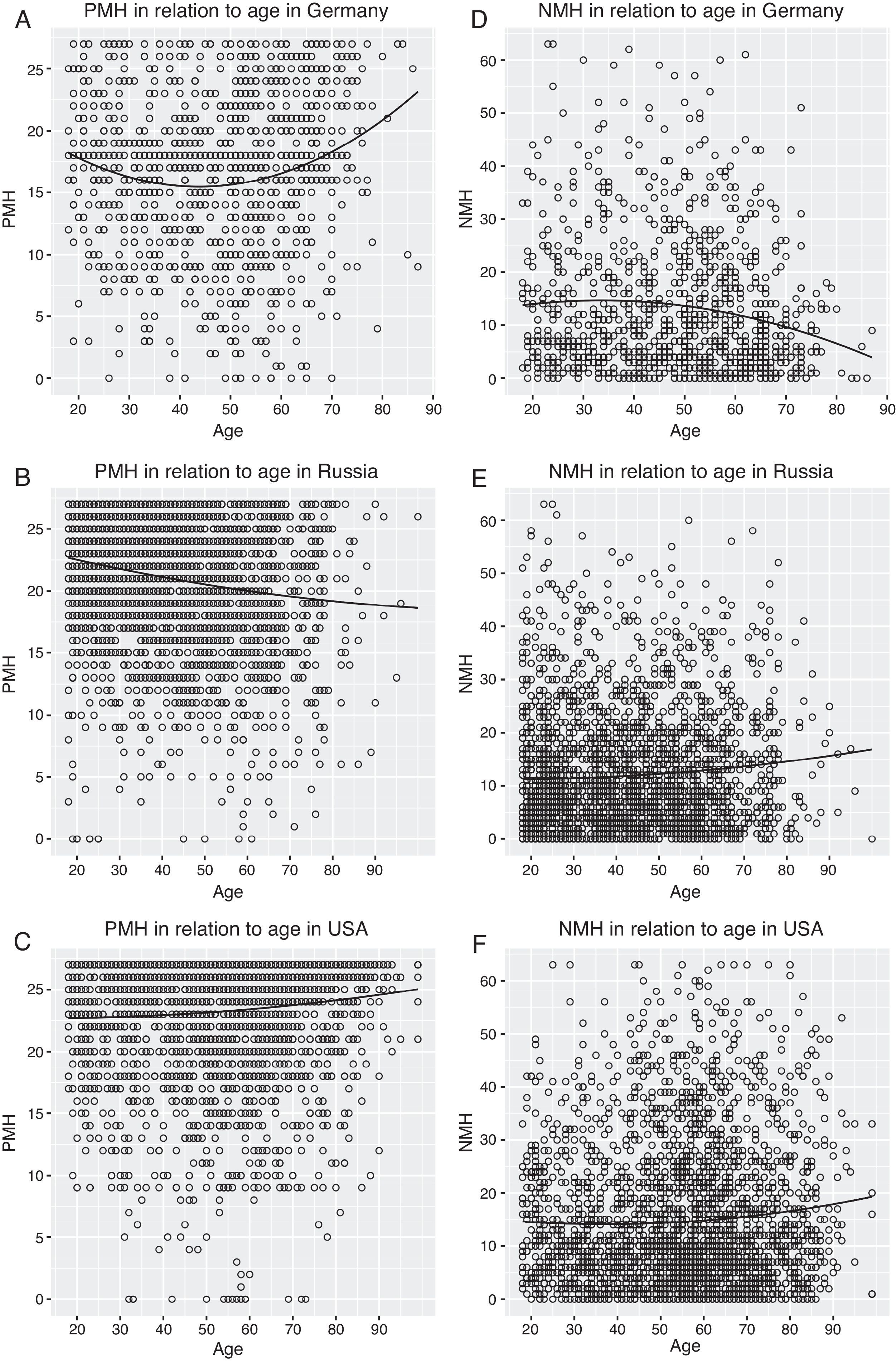
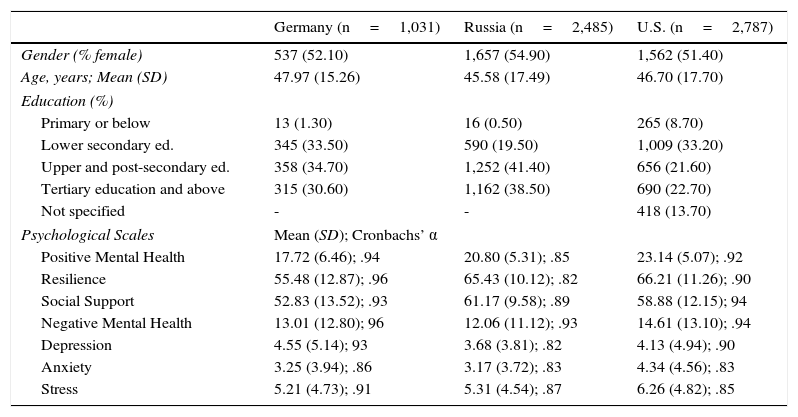
ResultsCharacteristics of the samplesIn Germany, a total sample of 1,031 subjects aged 18-100 years (52.1% female, Mage= 47.97, SDage= 15.26) completed the full battery of self-report questionnaires. Additionally, population-based samples were gathered from Russia (N=2,485, 54.9% female, Mage= 45.97, SDage= 17.49) and the U.S. (N=2787, 51.4% female, Mage= 46.70, SDage= 17.70) to compare the age-related pattern of mental health aspects in each nation. Sociodemographic characteristics, descriptive statistics and coefficients of internal consistency of the scales are shown in Table 1. There was a lower proportion of those with a primary educational level or below in each sample. On average, positive as well as NMH were the highest in the U.S. sample.
Characteristics of the participants by sample.
| Germany (n=1,031) | Russia (n=2,485) | U.S. (n=2,787) | |
|---|---|---|---|
| Gender (% female) | 537 (52.10) | 1,657 (54.90) | 1,562 (51.40) |
| Age, years; Mean (SD) | 47.97 (15.26) | 45.58 (17.49) | 46.70 (17.70) |
| Education (%) | |||
| Primary or below | 13 (1.30) | 16 (0.50) | 265 (8.70) |
| Lower secondary ed. | 345 (33.50) | 590 (19.50) | 1,009 (33.20) |
| Upper and post-secondary ed. | 358 (34.70) | 1,252 (41.40) | 656 (21.60) |
| Tertiary education and above | 315 (30.60) | 1,162 (38.50) | 690 (22.70) |
| Not specified | - | - | 418 (13.70) |
| Psychological Scales | Mean (SD); Cronbachs’ α | ||
| Positive Mental Health | 17.72 (6.46); .94 | 20.80 (5.31); .85 | 23.14 (5.07); .92 |
| Resilience | 55.48 (12.87); .96 | 65.43 (10.12); .82 | 66.21 (11.26); .90 |
| Social Support | 52.83 (13.52); .93 | 61.17 (9.58); .89 | 58.88 (12.15); 94 |
| Negative Mental Health | 13.01 (12.80); 96 | 12.06 (11.12); .93 | 14.61 (13.10); .94 |
| Depression | 4.55 (5.14); 93 | 3.68 (3.81); .82 | 4.13 (4.94); .90 |
| Anxiety | 3.25 (3.94); .86 | 3.17 (3.72); .83 | 4.34 (4.56); .83 |
| Stress | 5.21 (4.73); .91 | 5.31 (4.54); .87 | 6.26 (4.82); .85 |
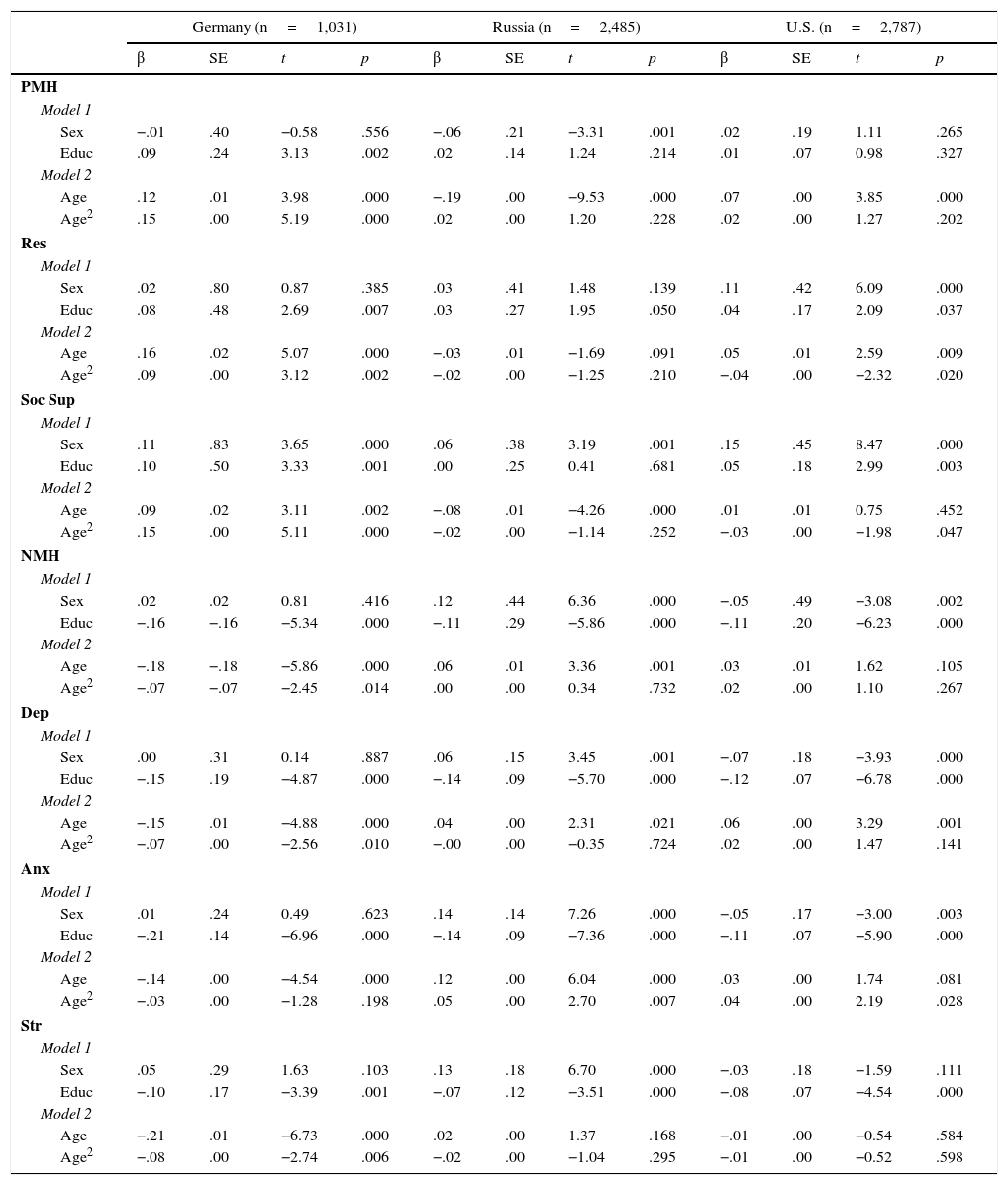
We conducted a series of multiple hierarchical regression analyses with estimated curve procedures to assess linear and quadratic trends in age by mental health associations separately for each indicator of mental health (Table 2). In the German sample the overall model including gender, education level and age accounted for 4.2% of variance for PMH, F (4, 1026)=12.35, p<.001. As shown in Table 2, age and age-squared had significant positive effects on PMH, which indicates a U-shaped curve for PMH in Germany. In Figure 1A, the trends are displayed in a scatterplot, showing a slight decrease of PMH until midlife and thereafter an increase. For resilience (F (4, 1026)=10.20, p<.001, R 2= .035) and social support (F (4, 1026)=13.81, p<.001, R2=.050) the overall models were also significant. The course of both resilience and social support was also U-shaped, evidenced in significant curvilinear effects of age. With an accounted variance of 5.5%, the model controlling for sociodemographic variables was also significant for NMH, F (4, 1026)=16.99, p<.001. There was a negative linear but also curvilinear effect of age, indicating an inverted-U function. As portrayed in Figure 1D, the level of NMH initially slightly increases, after which it declines during older adulthood. For the subscales depression (Model 2: F (4, 1026)=13.11, p<.001, R2=.045) and stress (Model 2: F (4, 1026)=16.06, p<.001, R2=.055), the linear and curvilinear effects of age were negative. On anxiety (F (4, 1026)=17.73, p<.001, R2=.061), the effect of age was also linear negative, indicating a general decrease from younger to older adulthood.
Ordinary least square regressions of age on positive and negative mental health.
| Germany (n=1,031) | Russia (n=2,485) | U.S. (n=2,787) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | t | p | β | SE | t | p | β | SE | t | p | |
| PMH | ||||||||||||
| Model 1 | ||||||||||||
| Sex | −.01 | .40 | −0.58 | .556 | −.06 | .21 | −3.31 | .001 | .02 | .19 | 1.11 | .265 |
| Educ | .09 | .24 | 3.13 | .002 | .02 | .14 | 1.24 | .214 | .01 | .07 | 0.98 | .327 |
| Model 2 | ||||||||||||
| Age | .12 | .01 | 3.98 | .000 | −.19 | .00 | −9.53 | .000 | .07 | .00 | 3.85 | .000 |
| Age2 | .15 | .00 | 5.19 | .000 | .02 | .00 | 1.20 | .228 | .02 | .00 | 1.27 | .202 |
| Res | ||||||||||||
| Model 1 | ||||||||||||
| Sex | .02 | .80 | 0.87 | .385 | .03 | .41 | 1.48 | .139 | .11 | .42 | 6.09 | .000 |
| Educ | .08 | .48 | 2.69 | .007 | .03 | .27 | 1.95 | .050 | .04 | .17 | 2.09 | .037 |
| Model 2 | ||||||||||||
| Age | .16 | .02 | 5.07 | .000 | −.03 | .01 | −1.69 | .091 | .05 | .01 | 2.59 | .009 |
| Age2 | .09 | .00 | 3.12 | .002 | −.02 | .00 | −1.25 | .210 | −.04 | .00 | −2.32 | .020 |
| Soc Sup | ||||||||||||
| Model 1 | ||||||||||||
| Sex | .11 | .83 | 3.65 | .000 | .06 | .38 | 3.19 | .001 | .15 | .45 | 8.47 | .000 |
| Educ | .10 | .50 | 3.33 | .001 | .00 | .25 | 0.41 | .681 | .05 | .18 | 2.99 | .003 |
| Model 2 | ||||||||||||
| Age | .09 | .02 | 3.11 | .002 | −.08 | .01 | −4.26 | .000 | .01 | .01 | 0.75 | .452 |
| Age2 | .15 | .00 | 5.11 | .000 | −.02 | .00 | −1.14 | .252 | −.03 | .00 | −1.98 | .047 |
| NMH | ||||||||||||
| Model 1 | ||||||||||||
| Sex | .02 | .02 | 0.81 | .416 | .12 | .44 | 6.36 | .000 | −.05 | .49 | −3.08 | .002 |
| Educ | −.16 | −.16 | −5.34 | .000 | −.11 | .29 | −5.86 | .000 | −.11 | .20 | −6.23 | .000 |
| Model 2 | ||||||||||||
| Age | −.18 | −.18 | −5.86 | .000 | .06 | .01 | 3.36 | .001 | .03 | .01 | 1.62 | .105 |
| Age2 | −.07 | −.07 | −2.45 | .014 | .00 | .00 | 0.34 | .732 | .02 | .00 | 1.10 | .267 |
| Dep | ||||||||||||
| Model 1 | ||||||||||||
| Sex | .00 | .31 | 0.14 | .887 | .06 | .15 | 3.45 | .001 | −.07 | .18 | −3.93 | .000 |
| Educ | −.15 | .19 | −4.87 | .000 | −.14 | .09 | −5.70 | .000 | −.12 | .07 | −6.78 | .000 |
| Model 2 | ||||||||||||
| Age | −.15 | .01 | −4.88 | .000 | .04 | .00 | 2.31 | .021 | .06 | .00 | 3.29 | .001 |
| Age2 | −.07 | .00 | −2.56 | .010 | −.00 | .00 | −0.35 | .724 | .02 | .00 | 1.47 | .141 |
| Anx | ||||||||||||
| Model 1 | ||||||||||||
| Sex | .01 | .24 | 0.49 | .623 | .14 | .14 | 7.26 | .000 | −.05 | .17 | −3.00 | .003 |
| Educ | −.21 | .14 | −6.96 | .000 | −.14 | .09 | −7.36 | .000 | −.11 | .07 | −5.90 | .000 |
| Model 2 | ||||||||||||
| Age | −.14 | .00 | −4.54 | .000 | .12 | .00 | 6.04 | .000 | .03 | .00 | 1.74 | .081 |
| Age2 | −.03 | .00 | −1.28 | .198 | .05 | .00 | 2.70 | .007 | .04 | .00 | 2.19 | .028 |
| Str | ||||||||||||
| Model 1 | ||||||||||||
| Sex | .05 | .29 | 1.63 | .103 | .13 | .18 | 6.70 | .000 | −.03 | .18 | −1.59 | .111 |
| Educ | −.10 | .17 | −3.39 | .001 | −.07 | .12 | −3.51 | .000 | −.08 | .07 | −4.54 | .000 |
| Model 2 | ||||||||||||
| Age | −.21 | .01 | −6.73 | .000 | .02 | .00 | 1.37 | .168 | −.01 | .00 | −0.54 | .584 |
| Age2 | −.08 | .00 | −2.74 | .006 | −.02 | .00 | −1.04 | .295 | −.01 | .00 | −0.52 | .598 |
Note. Sex (1=males, 2=females); Educ=education level; Age2=age squared; PMH=positive mental health; Res=resilience; Soc Sup=social support; NMH=negative mental health; Dep=depression; Anx=anxiety; Str=stress.
Scatterplots of the regression models. Quadratic function of PMH in relation to age (A) in Germany, (B) in Russia, and (C) in the U.S.; quadratic function of NMH in relation to age (D) in Germany, (E) in Russia, and (F) in the U.S.
Note. PMH=Positive mental health; NMH=Negative mental health
In Russia, the total model on PMH accounted for 3.8% of variance (F (4, 2480)=25.83, p<.001). By contrast to Germany, the linear coefficient of age had a negative sign, which demonstrates an overall decline of PMH. Figure 1B illustrates the linear trend according to which today's younger Russians experience the highest levels of PMH, whereas such high levels are found less often for the elderly. For resilience, we found no effects of age or other demographic variables (F (4, 2480)=2.94, p<.05, R2=.003), indicating no variations across the cohorts. However, age was predictive for social support, F (4, 2480)=8.09, p<.001, R2=.011. As can be seen in Table 2, the linear coefficient was negative which shows that perceived social support decreased with increasing age. In terms of NMH, the overall model accounted for 3.0% of variance (F (4, 2480)=20.49, p<.001) and there was a significant linear but non-significant squared effect of age. Moreover, sex and the level of school education significantly predicted NMH; being female and lower educated was associated with higher levels of NMH. Figure 1E illustrates the relationship between age and NMH with younger Russians reporting milder symptoms. There were no linear or curvilinear effects of age on the subscale stress (Model 2: F (4, 2480)=14.16, p< .001, R2=.021). For depression, we found a linear, yet low, positive effect of age and for anxiety also curvilinear effects.
The U.S. sample once more shows a different pattern regarding the relation between age and mental health. We found a linear positive effect of age on PMH (Model 2: F (4, 2782)=5.43, p< .001, R2=.006; Figure 1C). Moreover, there were linear as well as quadratic associations with resilience (Model 2: F (4, 2782)=12.28, p< .001, R2=.016), indicating an inverted U-shaped curve. Likewise, for social support (Model 2: F (4, 2782)=20.01, p< .001, R2=.027) the trend was inverted U-shaped with a peak in the younger and a decline in older adulthood, evidenced in the effects of age-squared. By contrast, there were no linear or curvilinear associations with NMH. As demonstrated in the scatterplot of Figure 1F, differentiations of NMH occurred equally across all ages. Yet, the overall model was significant (F (4, 2782)=12.40, p< .001, R2=.016) because sex and school education were important predictors. Here, again lower educational level and, surprisingly, male gender was associated with higher levels of NMH. Nevertheless, while there were no effects of age on stress (F (4, 2971)=6.54, p< .001, R2=.009), the linear negative effect on depression (F (4, 2782)=18.13, p< .001, R2=.024) indicated lower symptoms of depression in older adulthood. With regard to anxiety, a convex form was evidenced in quadratic effects. All regression coefficients of age and sociodemographic variables are presented in Table 2.
DiscussionWe primarily intended to examine age effects on PMH, perceived social support and resilience as well as NMH, including symptoms of depression, anxiety and stress in a cross-cultural comparison. Substantial differences between Eastern and Western countries were disclosed, evidenced in a series of age effects varying in sign and size. Cross-sectional population-based surveys from Germany, Russia and the U.S. were used in order to plot the level of the psychological scales in relation to age. Supporting divergences from previous research, which derived from national-different samples (e.g., Happell & Koehn, 2011; Uglanova, 2014), our results also indicate heterogeneous functions of age and indicators of mental health depending on the nationality of the sample.
The present study has some major strengths that extent prior research in this field. Aiming at assessing complete mental health across the whole adult lifespan, it is the first survey implementing the same scales in three different countries. Moreover, in accordance with a previous representative survey considering the two components of mental health (Westerhof & Keyes, 2010), this study included both dimensions of mental health, based on the assumption that the mere absence of psychopathologies represents an inferior outcome (e.g., Deci & Ryan, 2008; Keyes et al., 2002).
Unlike in Russia, where the effect of age was linear negative, we found positive effects of age in Germany and the U.S. for PMH. In terms of NMH, a contrary trend was found, with negative effects of age among the Germans and positive effects among the Russians. In Germany, there were additional squared effects for PMH and NMH, indicating a peak of mental health problems and a low of well-being at the middle of adulthood. For the U.S.-American sample, the overall psychopathological symptoms were constant across cohorts. Thus, contrary to our expectations, older Americans reached higher scores on PMH than younger adults, whereas there was no such an effect of age for total NMH. These findings support the dual-factor model of mental health (e.g., Keyes et al., 2002; Weich et al., 2011). Westerhof and Keyes (2010) likewise investigated the two-continua model in adult development in a representative Dutch survey and found fewer mental illness problems for the older adults, who, however, were not in better PMH. As a major result confirming our hypothesis, there is a contrast between the nations, that today's older Russians experience more NMH and less PMH, whereas today's older Germans and U.S.-Americans experience more PMH. This is in line with previous research from Europe and the U.S. (Reynolds et al., 2016; Westerhof & Keyes, 2010), demonstrating fewer mental illness problems and traumatic symptoms among older adults. The socioemotional selectivity theory (Carstensen, 2006) explains this pattern by a positivity shift in old age: A selective focus on negative information in early life change to a focus on positive stimuli in later life due to limited resources. However, as found in the Russian sample, previous studies also have demonstrated a decline of emotional and psychological well-being among higher age groups (Bălţătescu, 2014; Kaliterna & Burusic, 2014). One explanation could be the relation between mental health and social factors or purpose in life, which decreases in later life due to personal losses, such as widowhood or retirement (Pinquart, 2002). Life course issues, such as loss of independence, loneliness, limited mobility or physical health problems and chronic pain are special challenges of old the age. Poor economic and social conditions of a nation can result in mental impairments. Likewise, adverse effects of age on PMH and consumption of polypharmacy have been shown among patients with chronic physical health problems (Lluch-Canut, Puig-Llobet, Sánchez-Ortega, Roldán-Merino, & Ferré-Grau, 2013).
We further examined linear and curvilinear trends of NMH by investigating age effects for depression, anxiety and stress separately. In relation to symptoms of depression, today's younger adults reported higher symptoms than older adults of Germans, which is in line with previous research (Keyes & Westerhof, 2012), whereas in Russia and the U.S., the effects were positive. Furthermore, in terms of anxiety, results indicated a slight convex form across the cohorts. Interestingly, another U.S.-American cohort study found an inverted-U-shaped pattern across age for components of empathy (O’Brien, Konrath, Grühn, & Hagen, 2012). This peak in the middle adulthood is discussed with the dynamic integration theory arguing with emotional representations that growing cognitive capabilities promote emotional functioning (Labouvie-Vief, Grühn, & Studer, 2010). It is not yet clear how these findings might relate and if they were caused rather by cohort effects or by developmental changes. By contrast, we found a positive effect in Russia and a negative effect in Germany. Different pattern occurred for symptoms of stress, which were constant in Russia and the U.S., whereas the quadratic effect of age in Germany indicates a minor peak during midlife and lowest scores in older adulthood. Based on these findings, instead of predicting psychopathological symptoms as a whole, those specific indicators should be considered, since each subscale has its specific pattern within each country.
Finally, for resilience as an important protective factor for affective components and subjective well-being (Sagone & De Caroli, 2014), similar patterns were shown in the German and U.S. sample with squared effects of age, indicating lowest levels in midlife. By contrast, in Russia the level of resilience was constant across the cohorts. However, variations of contextual and economic conditions during lifetime affect the relationship between personal resources and age (see Lerner et al., 2012).
Although it is widely acknowledged that the perceived social support plays a crucial role for psychological distress (e.g., Markwick, Ansari, Sullivan, & McNeil, 2015), only few studies have examined on its course across the lifespan. While stress-buffering effects of social support have been found in diverse cultures, for instance in Taiwan (Li, Chen, Chang, Chou, & Chen, 2015), China (Lu et al., 2015) Italy and Switzerland (Fiorilli et al., 2015), the role of age still remained unclear. Among the older people in the present study, we found higher levels in Germany and lower levels in Russia. In the U.S., higher levels have been found in midlife and a decline in later life. Cohort-dependent effects of social support on the promotion of mental health have shown that community integration was more important for older adults, whereas functional support was more important for younger adults in order to promote mental health (Weiner et al., 2016).
Conclusions and future directionsFrom a global perspective, this study shows that complete mental health, resilience and social support across the lifespan varies substantially depending upon the particular economic and social circumstances each nation is exposed to. Different cohorts are subjected to different historical and political influences, which may also have caused the effects. As people from Eastern and Western countries are subjected to different socioeconomic conditions, causal conclusions based on the age are insecure. Although the discussed mechanisms indeed contribute to the cross-cultural differences, the extent of the effects being explained through additional macrosocial factors, such as the integration into the country-specific political system and society or the importance of traditions remains unclear. Ethnic identity development and cultural values, for example, can impact psychopathological symptoms (see Chandra, Arora, Mehta, & Radhakrishnan, 2015). Future research should focus on national characteristics and conditions that might identify more factors explaining those country-dependent age effects. For instance, life circumstances such as monetary or health care systems could be relevant, especially in old age.
Limitations occur due to the study's cross-sectional design so that it is not possible to distinguish between cohort and developmental effects. It is yet difficult to assess mental health longitudinally from a developmental lifespan perspective including the entire age range and to additionally compare several countries. Despite that further studies are needed to draw causal conclusions on adult development, our study elucidated substantial cross-cultural differences of mental health patterns. Both psychopathological symptoms and the emotional, psychological and social well-being should be emphasized in the relation between age and mental health of populations.
This study was supported by the Alexander von Humboldt Professorship awarded to Jürgen Margraf by the Alexander von Humboldt-Foundation.