Long-term childhood cancer survivors (CCS) are at risk for adverse late effects. However, not all of them are well understood. The present study addressed loneliness, a previously under-researched mental health risk in cancer survivor populations. We assessed the prevalence of loneliness and its impact on psychological symptoms over time. Method: A registry-based sample of N=633 adult long-term CCS underwent medical and psychological assessments and took part in a follow-up survey 2.5 years later. Psychological symptoms (somatic, anxiety, depression symptoms, and suicidal ideation) were measured using the Patient Health Questionnaire. We calculated linear regression models of symptoms at follow-up to investigate the impact of loneliness over time (controlling for symptoms at baseline and relevant confounders). Results: Loneliness was reported by 17.70% of CCS. In multivariate linear regression analyses, loneliness was still predictive of more severe anxiety symptoms and suicidal ideation over two years later. Loneliness did not predict somatic and depression symptoms at follow-up (which increased with age). Conclusions: Loneliness affected a significant number of CCS and was a risk factor for persistent anxiety symptoms and suicidal ideation. The extent to which young cancer patients’ re-integration into society is successful could thus have important implications for well-being in adulthood.
Los sobrevivientes a largo plazo de cáncer infantil (SCI) están en riesgo de sufrir efectos tardíos. Evaluamos la prevalencia de la soledad y su impacto en los síntomas psicológicos a lo largo del tiempo. Método: Una muestra de N=633 adultos con un pasado de SCI se sometió a evaluaciones médicas y psicológicas y participó en una encuesta de seguimiento 2,5 años después. Los síntomas psicológicos se midieron mediante el Patient Health Questionnaire. Calculamos modelos de regresión lineal de síntomas en el seguimiento para investigar el impacto de la soledad a lo largo del tiempo (controlando los síntomas al inicio y los factores de confusión relevantes). Resultados: La soledad fue reportada por el 17,70% de SCI. La soledad seguía siendo predictiva de síntomas de ansiedad más graves e ideación suicida dos años después. La soledad no predijo los síntomas somáticos y de depresión durante el seguimiento (que aumentaron con la edad). Conclusiones: La soledad fue un factor de riesgo para síntomas de ansiedad persistente e ideación suicida. La medida en que la reintegración de los pacientes jóvenes con cáncer en la sociedad tenga éxito podría tener importantes implicaciones para el bienestar en la edad adulta.
Cancer is a disruptive life experience. Besides physical late sequelae, many survivors report psychological distress (Bellver-Perez et al., 2019; Ichikura et al., 2020; Kuba et al., 2019). Especially survivors of childhood cancer face difficulties regarding psychosocial development as they still need to cope with essential developmental tasks when they fall ill (Brinkman et al., 2018; Friend et al., 2018; Nathan et al., 2018). By interfering with school demands and friendships alike, the disease complicates societal attainment as well as social integration (Stam et al., 2005).
Large-scale cohort studies showed that adverse psychosocial outcomes affected survivors for all their lives (Brinkman et al., 2018; Howard et al., 2014; Nathan et al., 2018). For instance, a greater percentage of Canadian survivors had no close friends than control participants (Barrera et al., 2005). Decades after diagnosis and treatment, childhood cancer survivors were less likely to be in a relationship, to live together with a partner, or to be married than adults of the same age (Burghardt et al., 2019; Stam et al., 2005).
Assessments of survivors’ subjective perceptions regarding the quality of their social interactions have shown variation. For instance, there is evidence for positive changes due to the disease, such as increases in compassion for others, greater appreciation and deepening of relationships (Lehmann et al., 2014; Mattsson et al., 2007). Survivors viewed themselves as more empathic and sensitive than before their illness (Karian et al., 1998). These aspects are often conceptualized as posttraumatic growth (Foley et al., 2006; Kim, 2017), a psychological concept which posits that traumatic life events can entail positive adaptations. By contrast, these studies have reported survivors’ subjective experience of disconnection from others. Adolescent cancer survivors in a Swedish study identified “difficulties interacting with others” as a negative social outcome of their disease (Lehmann et al., 2014). In a Canadian study, survivors were less likely than control participants to confide in their friends. Survivors reported to feel socially isolated (Howard et al., 2014) and as if they did not “fit in”(Foley et al., 2006).
The subjective perception of social connectedness might be harder to quantify than e.g. living conditions, but it has shown important relations to (mental) health outcomes. In particular, loneliness has recently come to the fore of epidemiological and psychological research (Cacioppo & Cacioppo, 2018). Loneliness describes the subjective mismatch between the social connections one wishes for and those currently available. It is an emotionally painful experience of the absence of social contact, belongingness, or a sense of isolation (Beutel et al., 2017) that cannot be equated with the physical presence or absence of others. Some groups of the population were disproportionately affected by loneliness: There was a peak in adolescence, when social acceptance and reciprocity in peer relationships becomes of paramount importance (Hawkley & Capitanio, 2015). It was also more common in women, participants living without a partner, and those without children (Beutel et al., 2017). Loneliness has been increasingly recognized as a mental health problem. For instance, in a longitudinal population study, it was predictive of depression symptoms 5 years later (Cacioppo, Hawkley, & Thisted, 2010).
Childhood cancer and its treatment entail long periods of reduced peer contact (due to hospitalization), changes in physical appearance and related experiences of stigmatization (e.g., hair loss), repetition of school classes, and other experiences setting CCS apart from their peers. These might make it difficult to (re-)integrate socially, with short- and long-term repercussions on forming friendships, partnerships and starting families (Desjardins et al., 2019; Newton et al., 2020). In any case, childhood cancer is a special and rather rare life event which can cause survivors to feel different from others (Zebrack & Chesler, 2001). It has been noted that not being able to relate to the people around one is the most painful form of social isolation (Cacioppo, Fowler, & Christakis, 2009). However, no study has investigated prevalence rates of loneliness, or determined the effects of loneliness over time in a large sample of long-term childhood cancer survivors (CCS) using established symptom measures. This presents a research gap as survivors’ social outcomes (e.g., fewer friends, lower rates of marriage) might make them particularly susceptible to experiencing loneliness.
We drew on a large, registry-based sample of German long-term CCS who had been investigated at two time points 2.5 years apart. Our aims were twofold: (1) To determine the prevalence of loneliness in a large sample of CCS; (2) To investigate whether loneliness was independently predictive of CCS’ psychological symptoms over time.
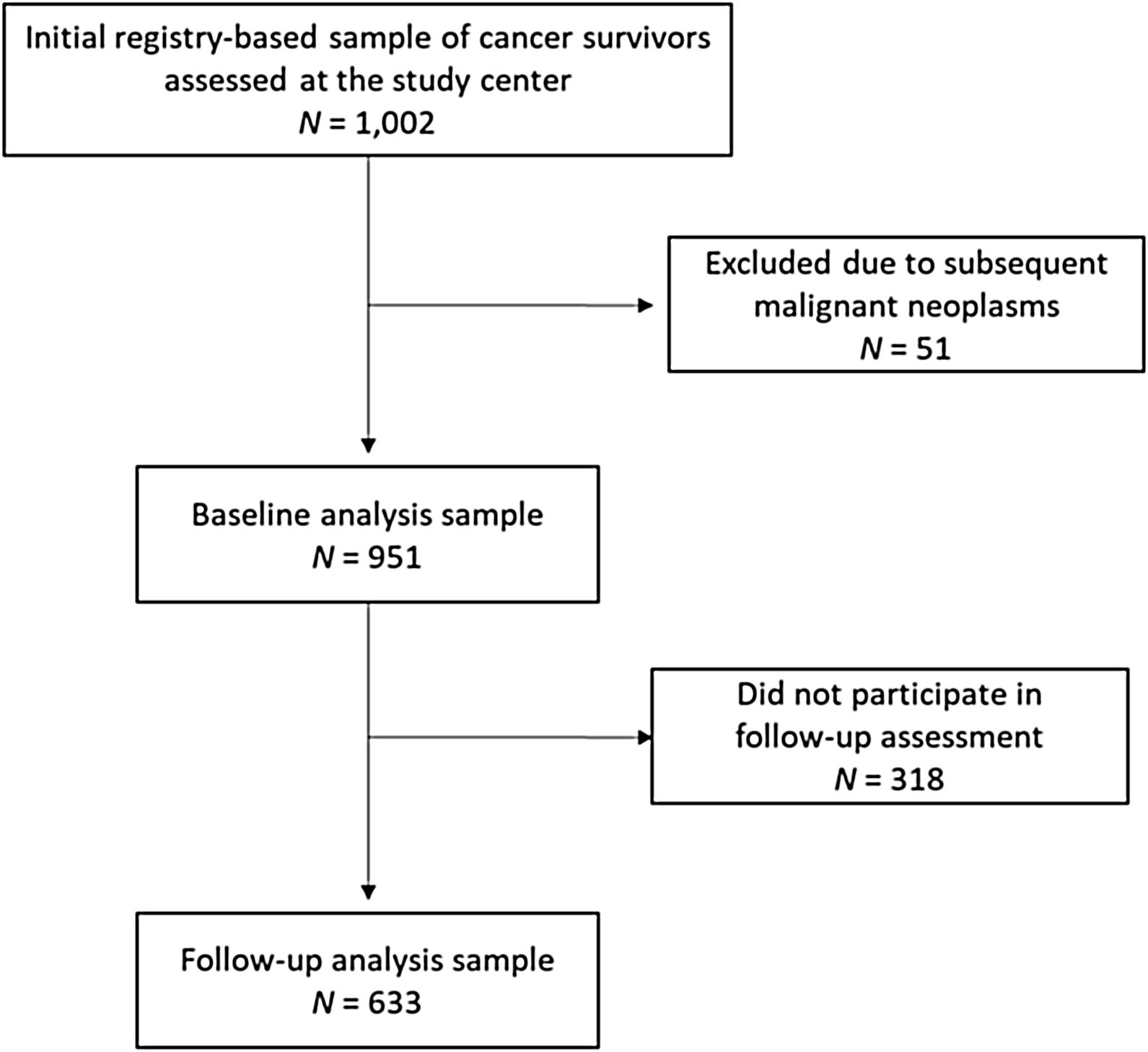
MethodParticipantsData reported here was collected as part of the studies CVSS (Cardiac and Vascular late Sequelae in long-term Survivors of Childhood Cancer, clinicaltrials.gov-nr.: NCT02181049) and PSYNA (Psychosocial long-term effects, health behavior and prevention among long-term survivors of cancer in childhood and adolescence). Participants were recruited in cooperation with the German Childhood Cancer Registry (GCCR) which systematically documents patients with childhood cancer residing in Germany since 1980. CCS were eligible for participation if diagnosed with neoplasia according to the International Classification of Childhood Cancer (ICCC-3; Steliarova-Foucher et al., 2005) between 1980 and 1990, before the age of 15, and if they had received antineoplastic treatment at one of 34 participating pediatric cancer centers. Survivors of Hodgkin lymphoma and a small group of former nephroblastoma patients could not be enrolled as they had taken part in other trials. A total of 2,894 eligible survivors were invited. Between 2013/09 and 2016/02, 1,002 CCS were examined at the study center. We excluded 51 individuals due to subsequent malignant neoplasms (as treatment of second tumors could potentially have additive negative effects on physical and mental health outcomes), arriving at a sample of 951 individuals. Characteristics of this baseline sample have been reported (Burghardt et al., 2019). A second assessment 2.5 years later (follow-up) consisted of a computer-assisted personal interview and a mailing of questionnaires. It was completed by 633 individuals who constitute the analysis sample of this investigation. Figure 1 shows the participant flow.
CVSS and PSYNA are carried out in accordance with the ethical standards of the institutional research committee (approved by the ethics review committee of the Rhineland-Palatinate Chamber of Physicians, nr. 837.453.13(9138-F)) and with the Declaration of Helsinki. All participants gave written informed consent for study participation and data retrieval.
MeasuresCancer-related data. CCS’ illness- and treatment-related information was abstracted from primary health records of former treating medical centers and/or centrally documented individual therapy data available at the Society for Pediatric Oncology and Hematology’s (GPOH) study centers. It was validated by trained medical staff. Sociodemographic information was assessed via self-report as part of a computer-assisted personal interview (CAPI). Socioeconomic status (SES) was defined according to Lampert et al. (2012). The aggregated index ranges from 3 (lowest) to 21 (highest), based on the level of education, profession, and income.
Physical health and health behavior. Participants completed a highly standardized 5.5-h examination including cardiovascular and clinical phenotyping (carried out by certified medical technical assistants according to standard operating procedures) which has also been described in more detail elsewhere (Faber et al., 2018). The study assessment comprised pulmonary disease (asthma or chronic bronchitis), kidney disease, cardiovascular disease (CVD) (summarizing myocardial infarction (MI), heart failure (HF), stroke, deep vein thrombosis (DVT), pulmonary embolism (PE), and peripheral arterial disease (PAD)), and diabetes (definite diagnosis of diabetes by a physician, intake of antidiabetic medication within the past two weeks, or a blood glucose level of ≥126mg/dl after an overnight fast of ≥8 hours or a blood glucose level of >200mg/dl after a fasting period of ≥8 hours). These conditions were summarized and are referred to as physical illnesses in this manuscript. Alcohol consumption was assessed via self-report in the context of the CAPI. Participants reported how often, how many, and which kinds of beverages they consumed in certain quantities. Following a standardized procedure, the number of grams/day was calculated from these responses. For Germany, recommended limits are 10grams/day for women and 20grams/day for men.
Participants were asked whether they smoked. Their responses were dichotomized into non-smokers (never smokers and ex-smokers) and smokers (occasional and frequent smokers).
Participants’ height was measured and they were weighed. Obesity was defined as a BMI>30kg/m2. Physical activity was inquired with the Short Questionnaire to Assess Health-Enhancing Physical Activity (SQUASH; Wendel-Vos et al., 2003). It comprises commuting, leisure time, household, work and school activities. Sleeping, lying, sitting and standing were classified as inactivity.
Loneliness was assessed using a single-item measure previously used in the representative Gutenberg Health Study (GHS; Beutel et al., 2017). Participants responded to the question “I am frequently alone/have few contacts” on a Likert scale: 0=no, does not apply, 1=yes it applies, but I do not suffer from it, 2=yes, it applies, and I suffer slightly, 3=yes, it applies, and I suffer moderately, 4=yes, it applies, and I suffer strongly. In line with previous work, the answers were recoded (0 and 1=no loneliness; 2=slight, 3=moderate, and 4=severe loneliness) and also summarized using a binary coding (0 and 1=no loneliness; 2-4=loneliness).
Somatic symptoms were inquired using the PHQ-15. This module of the Patient Health Questionnaire assesses the severity of 15 different somatic symptoms over the last four weeks. Participants rate each symptom on a Likert-scale (0=not bothered, 1=bothered a little, 2=bothered a lot). The sum score ranges from 0 to 30 (≥10 indicating increased symptom burden). The PHQ-15 showed a sensitivity of 78% and specificity of 71% in detecting DSM-IV diagnoses of somatoform disorder in primary care (Kocalevent, Hinz, & Brähler, 2013a; Kocalevent, Hinz, & Brähler, 2013b; Kroenke, Spitzer, & Williams, 2002). In our sample, it showed good internal consistency (ω=.83).
Anxiety symptoms were assessed with the GAD-2 which comprises two items of the Generalized Anxiety Disorder Scale (Hinz et al., 2017). Participants rated “Feeling nervous, anxious or on edge” and “Not being able to stop or control worrying” over the last two weeks (0=not at all, 1=several days, 2=more than half the days, 3=nearly every day). The sum score ranges from 0-6. A cut-off of ≥3 assessed generalized anxiety disorder with good sensitivity (86%) and specificity (83%) (Kroenke et al., 2007). It showed good internal consistency (ω=.78).
Depression symptoms were measured using the Patient Health Questionnaire’s Depression Module (Kocalevent et al., 2013a, 2013b). This questionnaire quantifies the frequency of being bothered by 9 diagnostic criteria of Major Depression and showed good internal consistency (ω=.87 in our sample). For each item, occurrence over the past two weeks is rated from 0 to 3: 0=not at all, 1=several days, 2=more than half the days, 3=nearly every day. The sum score ranges from 0-27. The PHQ-9 includes suicidal ideation (assessed by the item “Over the past two weeks, how often have you been bothered by thoughts that you would be better off dead or of hurting yourself in some way?”). Clinically relevant symptoms have been defined by a cut-off-score of ≥10 for the PHQ-9 (Kocalevent et al., 2013b) as well as for the PHQ-8 (excluding the suicidal ideation item) (Spangenberg et al., 2012). In the following, depression symptoms relate to the PHQ-8. The PHQ-8 is widely used, particularly in research settings (Kroenke et al., 2010). We investigated suicidal ideation separately as there is evidence for its independence from other depression symptoms (Teismann et al., 2018).
Statistical procedureFor the main analyses, we considered several adjustment variables as prevalence and severity of psychosocial late effects varied depending on diagnosis group, sex, and age (Brinkman et al., 2018). We aimed to control for such potentially confounding factors as well as for living circumstances. To avoid overfitting, we first tested sociodemographic, cancer-related, and health behavior variables with respect to their uni-/bivariate associations with the four kinds of symptoms of interest at follow-up. We then only included those variables into the models for which there were statistically significant associations. This pertained to living together with a partner, sex, age, and type of diagnosis, but not to age at diagnosis, current physical illness (such as diabetes or cardiovascular disease) or health behavior. We used continuous scores of all symptom measures at baseline and follow-up to take into account subclinical levels of symptoms and potential changes within this range. All regression models included the potential predictors type of diagnosis, age, female sex, living with partner, the respective symptom level at baseline (i.e., the regression model of somatic symptoms at follow-up included somatic symptoms at baseline as a predictor), and loneliness.
Assuming a moderate effect size (f2=0.15), the sample was large enough to carry out the planned linear regression models with six predictors each (the minimum required sample size being N=97). Given the small proportion of missing data (<2% per variable), no imputation methods were used. P-values correspond to two-tailed tests. Analyses were performed using SPSS 24 for Windows.
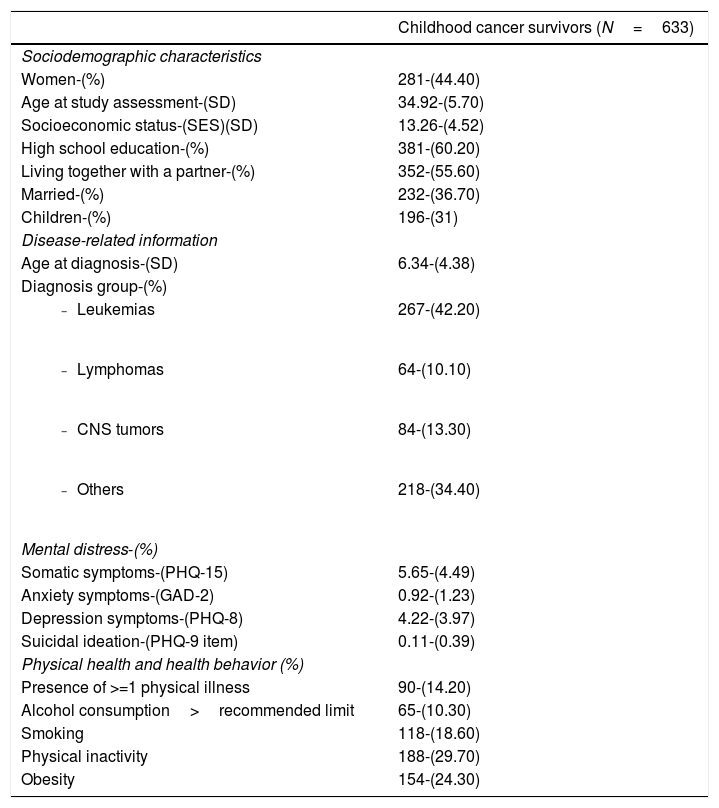
ResultsLoneliness at baselineAt baseline, 112 participants (17.70% of the sample) reported some degree of loneliness. Among them, 58 participants (9.20%) reported mild loneliness, 41 (6.50%) reported moderate loneliness, and 13 (2.10%) reported severe loneliness. Table 1 shows characteristics of the sample at baseline. The only differences between those who reported (any degree of) loneliness and those who did not report loneliness of at least medium effect size were observed for psychological symptoms: Loneliness co-occurred with more somatic (d=.79), anxiety (d=.72), and depression symptoms (d=.88).
Characteristics of study participants at baseline.
| Childhood cancer survivors (N=633) | |
|---|---|
| Sociodemographic characteristics | |
| Women-(%) | 281-(44.40) |
| Age at study assessment-(SD) | 34.92-(5.70) |
| Socioeconomic status-(SES)(SD) | 13.26-(4.52) |
| High school education-(%) | 381-(60.20) |
| Living together with a partner-(%) | 352-(55.60) |
| Married-(%) | 232-(36.70) |
| Children-(%) | 196-(31) |
| Disease-related information | |
| Age at diagnosis-(SD) | 6.34-(4.38) |
| Diagnosis group-(%) | |
| 267-(42.20) |
| 64-(10.10) |
| 84-(13.30) |
| 218-(34.40) |
| Mental distress-(%) | |
| Somatic symptoms-(PHQ-15) | 5.65-(4.49) |
| Anxiety symptoms-(GAD-2) | 0.92-(1.23) |
| Depression symptoms-(PHQ-8) | 4.22-(3.97) |
| Suicidal ideation-(PHQ-9 item) | 0.11-(0.39) |
| Physical health and health behavior (%) | |
| Presence of >=1 physical illness | 90-(14.20) |
| Alcohol consumption>recommended limit | 65-(10.30) |
| Smoking | 118-(18.60) |
| Physical inactivity | 188-(29.70) |
| Obesity | 154-(24.30) |
Note. Table shows baseline data.
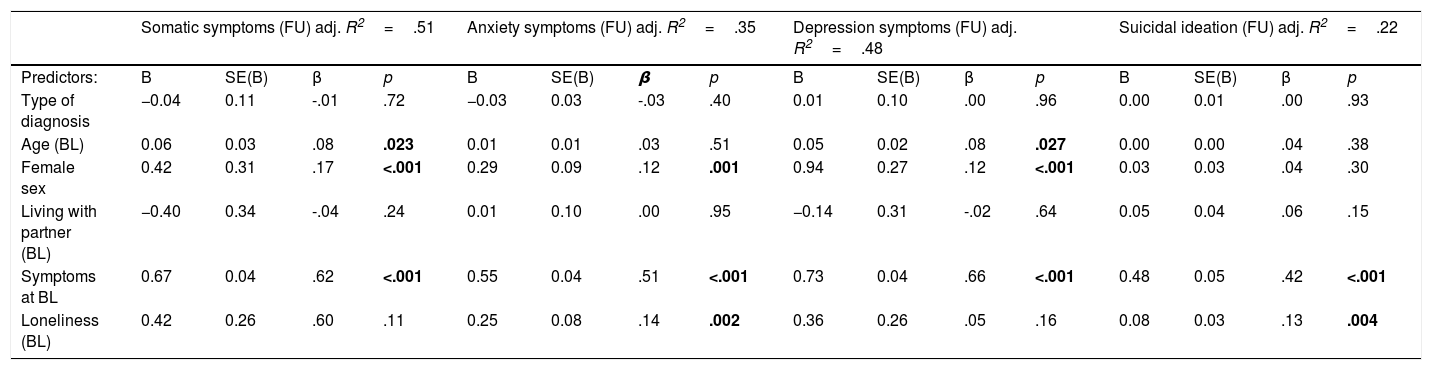
Loneliness at baseline was moderately correlated with symptoms at follow-up (somatic symptoms: r(630)=.34, p<.001; anxiety symptoms: r(629)=.33, p<.001; depression symptoms: r(630)=.39, p<.001; suicidal ideation: r(630)=26, p<.001). All four linear regression models yielded a highly significant statistical prediction of the investigated symptoms (Table 2). The model predicting somatic symptoms explained the largest proportion of variance. Loneliness at baseline was associated with more anxiety symptoms (β=.14, p=.002) and suicidal ideation (β=.13, p=.004) at follow-up. Loneliness had no effect in the models predicting somatic and depression symptoms at follow-up. Symptom burden at follow-up also varied by age and sex: Somatic and depression symptoms were associated with higher age. All symptoms except suicidal ideation were also positively associated with female sex. In all models, baseline symptom burden was positively associated with symptom burden at follow-up.
Results of the linear regression models of four kinds of mental distress at follow-up.
| Somatic symptoms (FU) adj. R2=.51 | Anxiety symptoms (FU) adj. R2=.35 | Depression symptoms (FU) adj. R2=.48 | Suicidal ideation (FU) adj. R2=.22 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictors: | B | SE(B) | β | p | B | SE(B) | β | p | B | SE(B) | β | p | B | SE(B) | β | p |
| Type of diagnosis | −0.04 | 0.11 | -.01 | .72 | −0.03 | 0.03 | -.03 | .40 | 0.01 | 0.10 | .00 | .96 | 0.00 | 0.01 | .00 | .93 |
| Age (BL) | 0.06 | 0.03 | .08 | .023 | 0.01 | 0.01 | .03 | .51 | 0.05 | 0.02 | .08 | .027 | 0.00 | 0.00 | .04 | .38 |
| Female sex | 0.42 | 0.31 | .17 | <.001 | 0.29 | 0.09 | .12 | .001 | 0.94 | 0.27 | .12 | <.001 | 0.03 | 0.03 | .04 | .30 |
| Living with partner (BL) | −0.40 | 0.34 | -.04 | .24 | 0.01 | 0.10 | .00 | .95 | −0.14 | 0.31 | -.02 | .64 | 0.05 | 0.04 | .06 | .15 |
| Symptoms at BL | 0.67 | 0.04 | .62 | <.001 | 0.55 | 0.04 | .51 | <.001 | 0.73 | 0.04 | .66 | <.001 | 0.48 | 0.05 | .42 | <.001 |
| Loneliness (BL) | 0.42 | 0.26 | .60 | .11 | 0.25 | 0.08 | .14 | .002 | 0.36 | 0.26 | .05 | .16 | 0.08 | 0.03 | .13 | .004 |
Note. BL: Baseline, FU: Follow-up. Symptoms at BL and FU as well as Loneliness at BL were entered as continuous scores. Symptoms at BL correspond to the symptoms at FU that are the dependent variable (e. g. in the model statistically predicting the sum of somatic symptoms at FU, the sum of somatic symptoms at BL was entered as a predictor).
The aims of the present study were to investigate the prevalence of loneliness as well as its relation with psychological symptoms over time in a large, registry-based sample of German cancer survivors that included all major diagnoses. Almost a fifth of participants (17.70%) reported some degree of loneliness. These numbers are higher than in population-based samples, for instance from Singapore (reporting 6.40%) (Ge et al., 2017). A German study which used the same single-item measure in a representative sample reported 10.50% (Beutel et al., 2017).
Although this is the first investigation of loneliness in a large sample of long-term CCS, the results are in line with previous reports from smaller qualitative (Howard et al., 2014; Lehmann et al., 2014) and bigger cohort studies which have shown negative social outcomes (Brinkman et al., 2018; Howard et al., 2014). Nevertheless, the majority of CCS in our study did not report loneliness, mirroring earlier research which reported that most long-term CCS are well-adjusted, but that some are struggling with negative sequelae of different kinds (Allen et al., 2018).
We examined somatic, anxiety, and depression symptoms as well as suicidal ideation. As these are common complaints (Brinkman et al., 2018; Burghardt et al., 2019; von Brachel et al., 2019), the present investigation is relevant for survivors’ lived outcomes. It reveals that subjective aspects of social integration play a role for CCS’ well-being over time, even when controlling for disease-related aspects, structural indicators of social integration, and symptom levels at baseline. The study corroborates reports from other populations which showed that the subjective feeling of loneliness was related to psychological symptoms such as anxiety symptoms and suicidal ideation irrespective of a partnership (Beutel et al., 2017; Curran, Rosato, Cooper, Mc Garrigle, & Leavey, 2019; Muyan et al., 2016; Schinka, Van Dulmen, Bossarte, & Swahn, 2012). Thus, living together with others might not always engender a sense of connectedness.
However, there were no significant effects of loneliness within the models of depression and somatic symptoms, contrasting previous research which found associations of loneliness and depression symptoms spanning multiple years (Cacioppo et al., 2010). These two models were also the only ones showing age effects. An explanation for these diverging patterns could be that the PHQ-8 and PHQ-15 capture somatic-affective symptoms (disturbed sleep and tiredness/loss of energy). By contrast, the GAD-2 assesses nervousness and worrying, and suicidal ideation is a cognitive symptom. Thus, depression and somatization could be part of a symptom complex whose severity increases as CCS grow older. Physical health conditions cumulate with age, and depression and somatic symptoms worsened over time and were associated with survivors’ declining subjective health ratings (Brinkman et al., 2013). Hence different kinds of symptoms might be shaped by different biological and social variables over the life span.
Importantly, the statistically significant predictors of psychological symptoms match results of previous studies in population and clinical samples: Symptoms at baseline were associated with symptoms at follow-up (Post, 2007), indicating that those who are distressed likely remain distressed/suffer a relapse in the future. Independent of symptom levels at baseline, women had a higher risk for most kinds of psychological symptoms than men, mirroring previous findings (Tibubos et al., 2019). Explanation models of sex/gender-dependent vulnerabilities have comprised genetic-biological, hormonal, and societal/gender-role related influences (Kuehner, 2017). Thus, in summary, disease-related and sociodemographic risk factors for mental health previously established in other contexts also affected CCS.
While we conceptualized loneliness as a predecessor of distress symptoms (Cacioppo et al., 2010; Saeri, Cruwys, Barlow, Stronge, & Sibley, 2018), it is important to note that psychological morbidity might also bring about loneliness, i. e. that there are bidirectional effects (Nuyen et al., 2020). Future research should investigate the direction of effects in cancer survivors to identify the most promising targets for prevention and intervention efforts.
In clinical practice, there are different ways to foster social connectedness in cancer patients and survivors: During hospital stays, technological means such as social media could offer a way for young patients to remain in contact with their peers. Later on, education and information work against potential stigma in their surroundings could counteract exclusion and victimization (Kim et al., 2018). Health professionals should offer low-threshold psychological support. Besides counseling/psychotherapy (Peikert et al., 2018), self-help groups and other activities with other young survivors might be sources of empowerment (Bashore & Bender, 2017; Dominguez & Sapina, 2017).
The study’s results have to be interpreted in light of its limitations. The specific sample might limit the findings’ generalizability. Perhaps childhood cancer patients face less stigma and better psycho-oncological support today compared to when our study participants were treated. There have also been technological advances which might help young cancer patients to stay connected with their peers. Thus, the maintenance of social contact or re-integration might be easier. We had no information about our participants’ social integration from the time of diagnosis and treatment.
We cannot ascertain whether the present sample is representative of the whole cohort with regard to psychosocial characteristics. As described, only a third of invited CCS took part in the study and not all of them completed the follow-up. These participation rates are slightly lower than in previous questionnaire surveys of German long-term survivors (Seitz et al., 2010). A comparison of study participants with the eligible source population showed a lower frequency of retinoblastoma and a higher frequency of leukemia. However, study participants and invited non-participants were comparable with respect to most demographic and cancer-related characteristics (Schneider et al., unpublished results).
ConclusionsThe present study demonstrated that psychosocial aspects such as loneliness are relevant health problems across cancer survivors’ life span. Lonely CCS were at a greater risk for suicidal ideation and anxiety symptoms over two years later. Thus, there is a need to raise awareness of young cancer survivors’ challenges and to provide targeted support.
Funding and AcknowledgementsWe thank all former childhood cancer patients who underwent clinical examination for this study, all participating and supporting medical centers, the study centers of the GPOH, the staff of the GHS, and the staff of the treatment data retrieval team. The CVSS is funded by the German Research Foundation (DFG) (SP1381/2-1&2, FA1038/2-1&2, WI3881/2-1&2). PSYNA is funded by the German Cancer Aid (DKH) (70112165, 70113623). P.S. Wild is funded by the Federal Ministry of Education and Research (BMBF01EO1503).