proctocolectomy with ileal reservoir is the surgical procedure of choice for patients with ulcerative colitis and familial adenomatous polyposis.
ObjectivesTo evaluate long-term postoperative complications (1994–2019) in patients operated for familial adenomatous polyposis (FAP) and ulcerative colitis (UC) and the degree of satisfaction with the procedure.
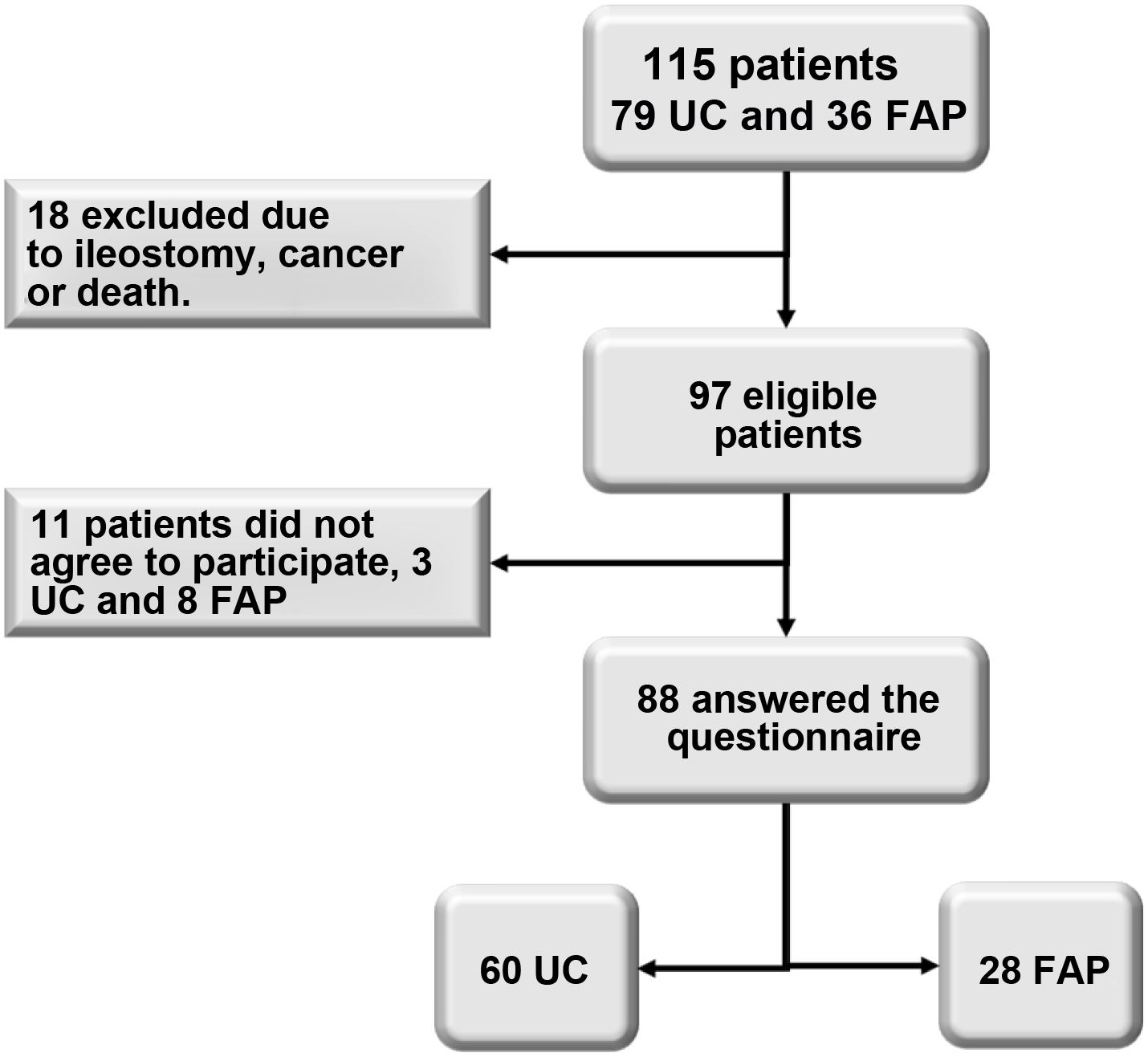
MethodsObservational study based on the analysis of a retrospective database with prospective follow-up in 115 consecutive patients: 79 with UC and 36 with FAP. A total of 88 patients were followed up, 60 with UC and 28 with PFA.
Results48 males (54.4%) with a mean age of 44.8 ± 10.6 years were evaluated. Indications for surgery were intractable disease in 54 patients (47%), dysplasia/cancer in 43 (37%), severe bleeding in 4 (4%) and perforation in 3 (3%). A proctectomy and mucosectomy of the rectal stump was performed in 67 (76.1%), and a double stapling technique in 21. A protective ileostomy was performed in all patients with UC and FAP. No differences were found in early complications between the two groups. Late complications showed a higher rate of reservoritis in UC patients compared to FAP (44.9% vs 14.3% p = 0.001), with more refractory reservoritis in the UC group (13.3% vs 0% p = 0.04) with no differences in bowel obstruction, strictures, or anastomotic fistulas. Overall satisfaction and adaptation were considered good in 87% of UC patients and only 57% in the FAP group (p < 0.01).
ConclusionsProctocolectomy with ileal reservoir has comparable morbidity and mortality, except for the higher rate of reservoritis in patients with a history of UC, despite this contingency there is a better quality of life and greater acceptance of surgery in UC patients than in FAP patients.
La proctocolectomía con reservorio es el procedimiento quirúrgico de elección para los pacientes con colitis ulcerosa y poliposis adenomatosa familiar.
ObjetivosEvaluar las complicaciones postoperatorias a largo plazo (1994–2019) en pacientes operados por poliposis familiar adenomatosa (PFA) y colitis ulcerativa (CU) y el grado de satisfacción con la intervención.
MétodosEstudio observacional basado en el análisis de una base de datos retrospectiva con seguimiento prospectivo en 115 pacientes consecutivos: 79 con CU y 36 con PFA. Se ha realizado el seguimiento de un total de 88 pacientes, 60 con CU y 28 con PFA.
ResultadosSe evaluaron 48 varones (54,4%) con una edad media de 44,8 ± 10,6 años. Las indicaciones para la cirugía fueron enfermedad intratable en 54 pacientes (47%), displasia/cáncer en 43 (37%), sangrado severo en 4 (4%) y perforación en 3 (3%). Se realizó una proctectomía y mucosectomía del muñón rectal en 67 (76,1%), y una técnica de doble grapado en 21. Se realizó una ileostomía protectora en todos los pacientes con CU y PFA. No se encontraron diferencias en las complicaciones tempranas entre los dos grupos. Las complicaciones tardías mostraron una mayor tasa de reservoritis en los pacientes de la CU respecto a la PFA (44,9% vs 14,3% p = 0,001), con más reservoritis refractaria en el grupo de la CU (13,3% vs 0% p = 0,04) sin diferencias en cuanto a obstrucción intestinal, estenosis o fístulas anastomóticas. La satisfacción general y la adaptación se consideraron buenas en el 87% de los pacientes con CU y sólo en el 57% del grupo de PFA (p < 0,01).
ConclusionesLa proctocolectomía con reservorio ileal tiene una morbilidad y mortalidad comparables, excepto por la mayor tasa de reservoritis en los pacientes con antecedentes de CU, a pesar de esta contingencia hay una mejor calidad de vida y mayor aceptación de la cirugía en los pacientes con CU que en los pacientes con PFA.
Restorative proctocolectomy with ileal pouch-anal anastomosis (RP-IPAA) was described in the late 1970s as an alternative to total colectomy with Brooke ileostomy, continent ileostomy or ileorectal anastomosis1. RP-IPAA has become the procedure of choice for the surgical treatment of patients with ulcerative colitis (UC) and familial adenomatous polyposis (FAP), who account for almost 20% of patients with UC2. This procedure combines the goals of removing the affected colon and rectum, reducing the risk of cancer and maintaining gastrointestinal continuity, transanal defecation and continence. Although most patients benefit from a significant improvement in quality of life, with good functional outcomes, RP-IPAA surgery can be associated with a significant number of complications leading to pouch removal or permanent diverting colostomy3,4.
Several studies have examined the short- and long-term reasons for ileal pouch failure and have found that unrecognised Crohn's disease5,6, indeterminate colitis7, pelvic sepsis8, extension of rectal stump mucosectomy9, sclerosing cholangitis10 and fistula formation11 can contribute to poor functional outcomes and lead to a diverting ileostomy, or excision of the pouch12,13. There is much debate regarding functional outcomes. While in the short term they are very satisfactory and remain constant9, some studies have suggested that functional outcomes deteriorate over time14.
The most common complication after an ileal pouch has been created is so-called "pouchitis"15,16. Characteristic, though nonspecific, clinical symptoms include abdominal pain, especially with bowel movements, loose stools with a mixture of mucus and blood, faecal urgency, fever, and diarrhoea that can rapidly lead to severe dehydration17,18. Pouchitis is more common in patients operated on for UC than for FAP. The incidence of pouchitis is reported in up to 45% of patients undergoing RP-IPAA, with a prevalence of 25%, 32%, 36%, 40% and 45% after one, two, three, four and five years following the procedure, respectively15,19. There are several inflammation rating scales; the most commonly used is the Pouchitis Disease Activity Index (PDAI) that evaluates clinical, endoscopic and histological aspects, presented by the Mayo Clinic group in 199420. This has been modified to suppress the histological aspects, making it more practical and with the same sensitivity and specificity21.
This study aims to evaluate not only early and late complications, but also the onset or otherwise of cancer and the functional outcomes and long-term quality of life in patients undergoing RP-IPAA with ileoanal or ileorectal anastomosis for UC or FAP during 25 years of follow-up.
Patients and methodsBetween January 1994 and December 2019, 115 consecutive patients underwent RP-IPAA, 79 for a preoperative diagnosis of UC and 36 for FAP. The surgical procedures were performed in four tertiary-level hospitals in the city of Medellín, in Colombia.
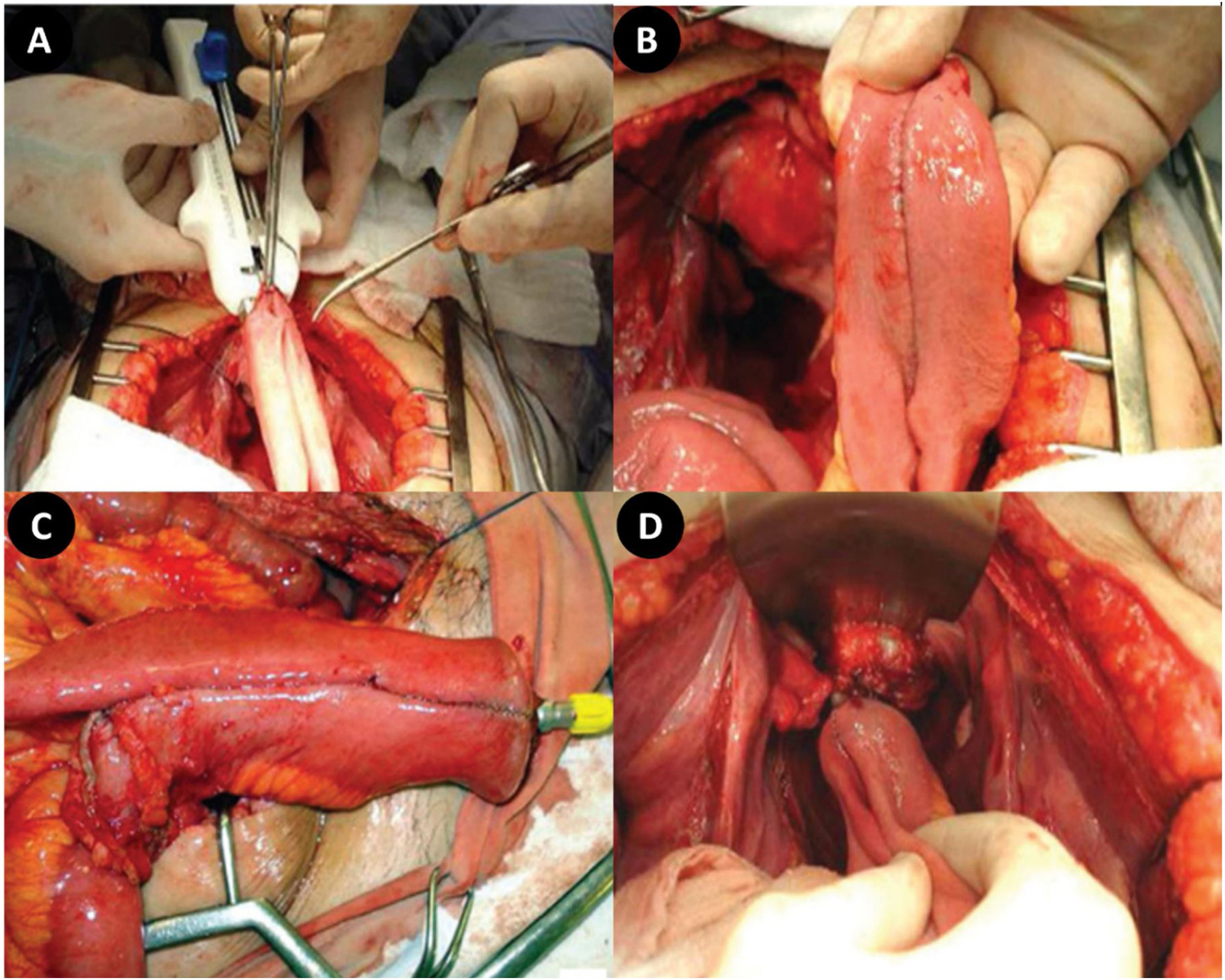
The surgery was elective in all cases. The ileal pouch was always J-shaped with ileoanal or ileorectal anastomosis made by hand or by double stapling technique according to the surgeon's preference (Fig. 1).
A temporary protective loop ileostomy (two-stage technique) was performed in all patients. Ileostomy closure was always preceded by radiographic and/or endoscopic examination and digital examination, with digital dilation of the ileoanal anastomosis when necessary.
The patients' outcome was evaluated by reviewing hospital records, telephone interview, or direct approach during the routine examination in the hospital according to the modified Öresland questionnaire22, which is a structured questionnaire used to assess continence, bowel function and general satisfaction, and consists of 10 categories: the number of bowel movements (day and night), faecal incontinence (day or night), perianal pain, presence of faecal urgency, evacuation difficulties, the use of protective pads, dietary restrictions, frequency of medication use, impact on social participation and whether or not the patient feels better after surgery. Each item is scored as 0/1 or 0/1/2, and the sum of all items ranges from 0 to 15 points. A lower score indicates better function, and scores of 8 or higher are associated with poor pouch function (Table 1).
Modified Öresland score to assess ileal pouches.
| Function | Score | |||
|---|---|---|---|---|
| 0 | 1 | 2 | ||
| Bowel movements | Day | ≤3 | 4–5 | ≥6 |
| Night | 0 | 1 | ≥2 | |
| Faecal incontinence | Day | No | >1 time/week | |
| Night | No | >1 time/week | ||
| Perianal pain | No | Occasional | Permanent | |
| Faecal urgency | No | Yes | ||
| Difficult evacuationa | No | Yes | ||
| Use of perianal protective pad | No | >1 time/week | ||
| Dietary restrictions | No | Yes | ||
| Use of medications | No | Yes | ||
| Worse health | No | Yes | ||
| Worse after surgery | No | Yes | ||
During follow-up, a physical examination was performed in the hospital with special attention to the digital examination in order to evaluate the status of the anastomosis, the anal canal, the pouch, the stricturing and the sphincter mechanism. When symptoms of pouchitis were suspected, an endoscopic study with biopsy was added, and when ileoanal stricture was detected, immediate digital dilation was performed.
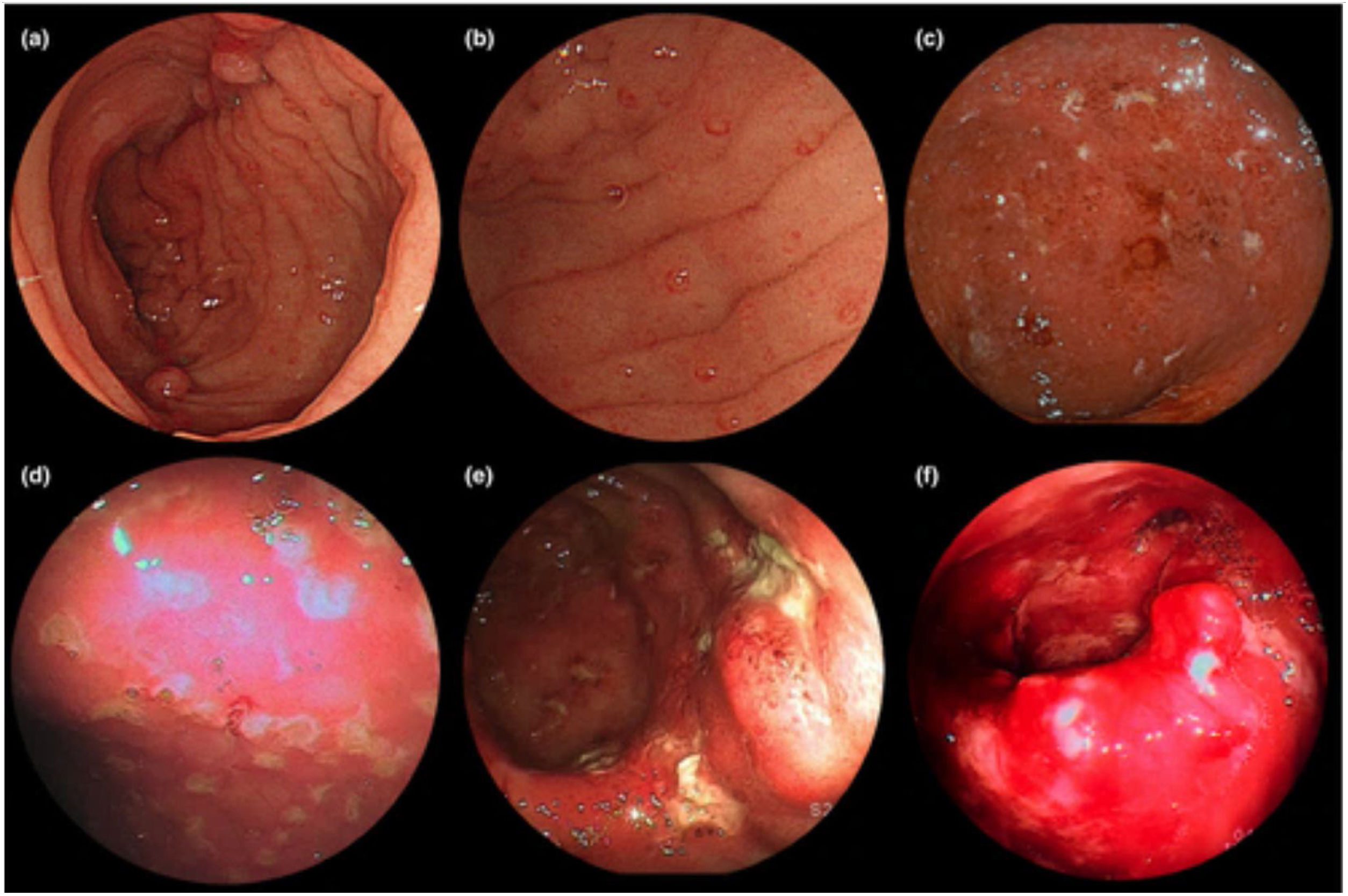
In the vast majority of patients, endoscopic examinations were performed on an outpatient basis with a high endoscope, which facilitates instrumentation. Pouchitis was diagnosed based on the modified PDAI score. The modified PDAI scale is based on a combined evaluation of the clinical and endoscopic findings, without considering the histological changes (the Moskowitz histological index)21. All six endoscopic subcomponent scores (oedema, granularity, friability, loss of vascular pattern, mucus, exudate and ulcer) contributed to the total endoscopic score with a similar degree of magnitude (Fig. 2).
Endoscopic aspects of pouchitis: (a,b) Endoscopic appearance of mild pouchitis. (a) Loss of vascularity and (b) mild redness are seen relatively frequently in patients without pouchitis. (c,d) The endoscopic appearance of moderate pouchitis includes aphthous lesions, erosions, shallow ulcers and mucous exudates. (e,f) The endoscopic appearance of severe pouchitis includes (e) multiple deep ulcers and (f) spontaneous bleeding. Modified from Hata38.
For statistical analysis, functional outcomes were compared using the Yates-corrected χ2 test. A p value <0.05 was considered statistically significant.
The Independent Ethics Committee of the Universidad de Antioquia [University of Antioquia] evaluated the methodological, ethical and legal aspects, in accordance with its objectives of safeguarding the rights, dignity, safety and well-being of both the participants and the investigators, prioritising the well-being of subjects above scientific, academic or community interests, and ensuring that the potential benefits of studies outweigh the expected risks.
ResultsWe performed this retrospective observational study on a prospective follow-up basis in 115 patients: 79 with UC and 36 with FAP. Follow-up findings were recorded for a total of 88 patients, 60 with UC and 28 with FAP (Fig. 3).
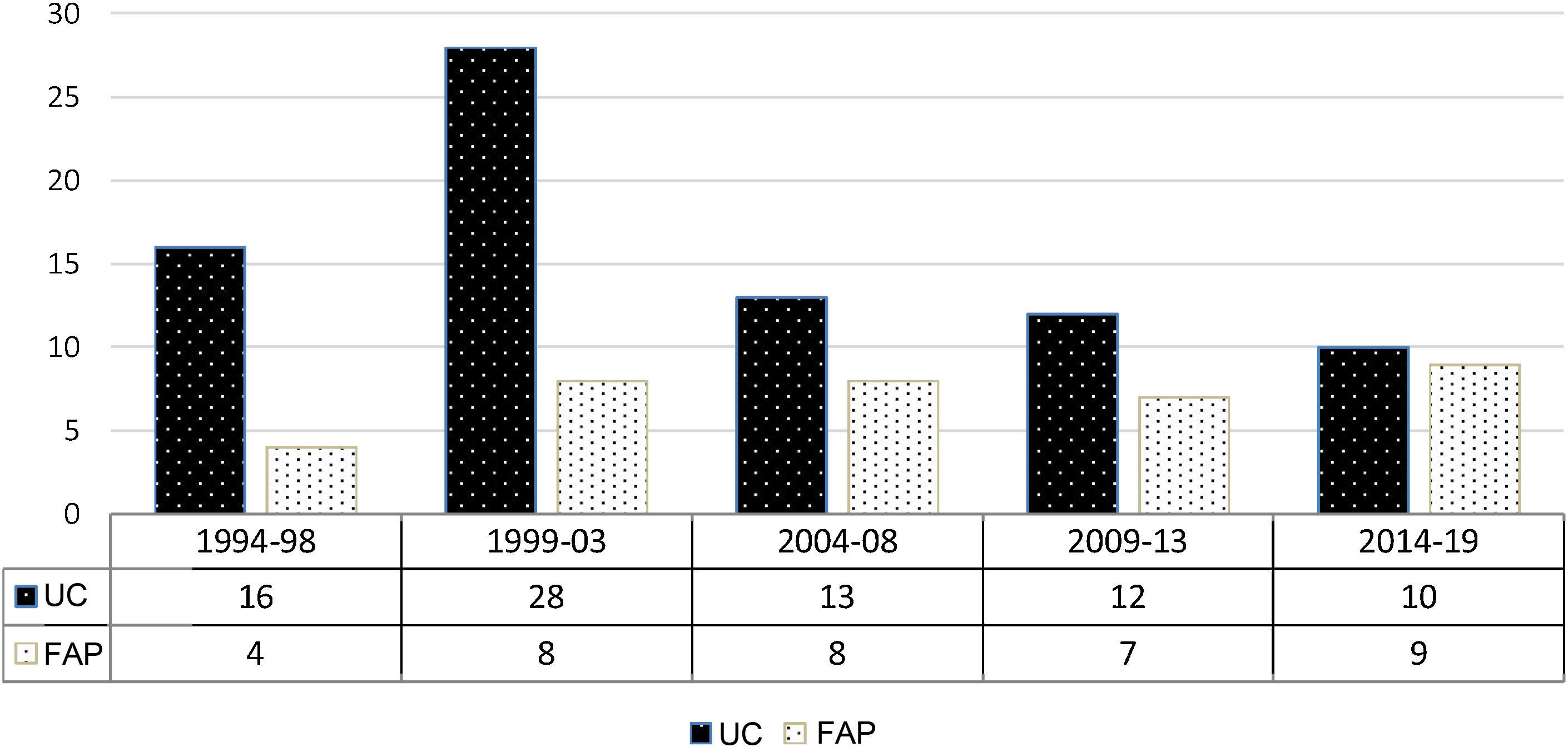
The patients, 48 men (54.4%) and 40 women with a mean age of 44.8 ± 12.7 years (range 19–67 years), underwent the procedure between January 1994 and January 2019 (mean follow-up 84.8 months, range 14–300 months). Indications for surgery were intractable disease in 54 patients (47%), dysplasia/cancer in 43 (37%), major bleeding in four (4%) and perforation in three (3%). The time distribution of the procedures for FAP and UC are shown in Fig. 4.
At the beginning of the experience, a proctectomy and mucosectomy of the rectal stump anastomosed by hand was performed in 68 patients (59%), while more recently and according to the surgeon's preference, the double stapling technique was performed in 47 patients (41%). In all the patients, the pouch was a J-type pouch. The mean length of hospital stay was 11.6 ± 5.8 days (range 6–34 days, median 8). Ileostomy closure was performed between 37 and 312 days after pouch construction (mean 117 ± 58 days).
Long-term follow-up data on the 88 patients (76.5%) were obtained by telephone interview or by filling out a questionnaire during the follow-up visit. Early and late postoperative complications are summarised in Table 2.
Most prevalent early (≤30 days) and late (>30 days) postoperative complications.
| Ulcerative colitis (%) | Familial polyposis (%) | Total (%) | p | ||
|---|---|---|---|---|---|
| Early complications | Wound infection | 13 (21.7) | 3 (10.7) | 16 (18.2) | 0.214 |
| Anastomosis leak | 6 (10.0) | 2 (7.1) | 8 (9.1) | 0.664 | |
| Pelvic sepsis | 5 (8.3) | 2 (7.1) | 9 (7.9) | 0.514 | |
| Intestinal obstruction | 5 (8.3) | 1 (1.7) | 6 (6.8) | 0.409 | |
| Ileostomy dysfunction | 4 (6.7) | 2 (7.1) | 6 (6.8) | 0.162 | |
| Late complications | Pouchitis | 27 (45) | 4 (14.3) | 31 (35.2) | 0.001 |
| Refractory pouchitis | 8 (13.3) | 0 | 8 (9.1) | 0.043 | |
| Intestinal obstruction | 16 (26.7) | 11 (39.3) | 27 (30.7) | 0.236 | |
| Anastomosis stricture | 15 (25) | 4 (14.3) | 19 (21.6) | 0.196 | |
| Anastomosis fistula | 5 (8.3) | 1 (1.7) | 6 (6.8) | 0.409 | |
| Loss of the pouch | 4 (6.7) | 0 | 4 (4.5) | 0.162 | |
| New ileostomy | 3 (5.0) | 0 | 3 (3.0) | 0.228 | |
| Mild dysplasia | 0 | 1 (1.7) | 1 (1.0) | 0.141 | |
| Mortality | 2 (2.3) | 0 | 2 (2.3) | 0.328 |
In six patients with late-onset obstruction (22.2%), laparotomy was required to release adhesions or resect a segment of intestinal stricture (two patients).
The most common late postoperative complication was pouchitis (35.2%). This complication tends to be mild, with an increase in the frequency of bowel movements, abdominal cramps, tenesmus and partial loss of continence, with discomfort and slight temperature. Antibiotic therapy, usually with a combination of ciprofloxacin and metronidazole, and conventional treatment with 5-ASA and steroids led to the resolution of symptoms in a few days in most cases.
A mild anastomotic stricture that normally responded to finger dilation was a common finding in 19 patients, whereas a severe stricture, which required at least mechanical dilation with or without anaesthesia, developed in 11 patients.
Other complications of the procedure were impotence with retrograde ejaculation in two men (2.2%) and pouch-vagina fistula in two women (2.2%). Impotence with retrograde ejaculation only developed in patients who underwent the double stapling technique, but was not detected in our experience in patients who underwent manual proctectomy and mucosectomy of the rectal stump, most likely because resection of the rectal mucosa was performed from inside the rectum.
Long-term follow-up information is available for 88 patients, 60 of 79 patients with UC (75.9%) and 28 of 35 patients with FAP (80%) (Table 3). The median number of bowel movements was 5/24 h in patients with UC, and 4/24 h in patients with FAP, with one per night in both groups. All patients passed stools spontaneously. Dietary restrictions were common in both groups (43.2%), mainly to alter the timing of their meals in order to avoid bowel movements at inappropriate times (during social activities, at night, etc.). A total of 85.2% of the patients had full continence during the day, while 75% only had full continence at night, with the use of nappies in 10.2% and faecal urgency in 12.5%. Overall, there were no significant differences in continence between UC and FAP patients.
Long-term well-being according to the response to the questionnaire.
| Ulcerative colitis (%) | Familial polyposis (%) | Total (%) | p | |
|---|---|---|---|---|
| n | 60 (76.9) | 28 (80) | 88 (76.5) | – |
| Medications | 14 (23.3) | 5 (17.8) | 18 (20.4) | 0.560 |
| Dietary restrictions | 26 (43.3) | 12 (32.1) | 38 (43.2) | 0.966 |
| Bowel movements (day)a | 5 | 4 | – | |
| Bowel movements (night)a | 1 | 1 | – | |
| Continence (day) | 52 (86.7) | 23 (82.1) | 75 (85.2) | 0.577 |
| Continence (night) | 47 (78.3) | 19 (67.8) | 66 (75.0) | 0.290 |
| Faecal urgency | 8 (13.3) | 3 (10.7) | 11 (12.5) | 0.729 |
| Use of nappies | 7 (11.7) | 2 (7.1) | 9 (10.2) | 0.658 |
| Feels better after the operation | 55 (91.7) | 20 (71.4) | 75 (85.2) | 0.012 |
| Overall satisfaction | 52 (86.7) | 16 (57.2) | 68 (77.3) | 0.002 |
Patients with RP-IPAA for UC had a better overall Öresland score (median = 3, interquartile range [IQR] 2–5) than patients with RP-IPAA for FAP (median = 10, IQR 5–15) (p < 0.001).
UC patients judged their quality of life to be better in 90% of cases, while only 71.4% of FAP patients believed that their quality of life had improved after the operation (p = 0.01). General satisfaction and adaptation were considered good in 87% of the UC patients, but only in 57% of the FAP group (p < 0.01) (Table 3).
The presence of mild dysplasia in the pouch that did not progress over time was documented in only one patient, and in no case was cancer in the pouch documented.
DiscussionThe primary objective of the study was to update the follow-up of a cohort of patients that began in 1994, collecting the initial experience with 51 patients who required ileal pouches due to UC or FAP, in whom early and late complications were evaluated23.
Due to the complexity of the operation and the relatively high rate of early and late complications, the indications for this type of surgery were initially conservative. With the advent of laparoscopic and robotic techniques24,25, and the growing experience with the use of the double-stapled J-pouch and the preservation of the anal transitional zone, the indications for surgery have been extended to higher-risk patients, in selected cases without the need for a protective ileostomy26, even for patient over 60 years of age27 or obese28, with satisfactory functional outcomes29.
A meta-analysis of 53 studies with nearly 15,000 patients who underwent RP-IPAA between 2000 and 2010 suggests that the overall pouch failure rate worldwide was approximately 7.5%30, a figure that has hardly changed (7.7%) in the most recent reports31. These positive outcomes are attributed to more careful patient selection, more definitive preoperative diagnosis, more experienced surgeons with better surgical techniques (laparoscopy or robotic surgery), better postoperative care and intensive patient follow-up and education. The main causes of adverse outcomes with pouch failure were directly associated with Crohn's disease or its associated complications, such as fistulas, perianal sepsis, the presence of sinuses, etc. Pelvic sepsis is almost always due to some degree of leakage from the ileoanal anastomosis. In our study, 7.9% of patients developed early postoperative sepsis of pelvic origin, and 9.1% developed anastomotic leaks, all of whom responded to percutaneous drainage and antibiotic therapy. The causes of a new ileostomy in three patients in our study were recurrent severe pouchitis that did not respond to conservative therapy in two patients, and anal sphincter incontinence in one patient.
Pouchitis is the most common complication of RP-IPAA in UC and its management requires a sequential and personalised approach32. The aetiology of pouchitis is unclear, and pouchitis may well represent a further manifestation of idiopathic inflammatory bowel disease. Diagnosis of the disease depends mainly on symptoms, endoscopy and histology. An 18-point pouchitis disease activity index was recently developed, which was later simplified by omitting histological evaluation, with similar sensitivity and specificity21. Mild pouchitis is a long-term complication that occurred cumulatively in up to 35.2% of patients, with severe pouchitis unresponsive to conservative therapy in 9.1%. Mild pouchitis occurred in both UC and FAP patients, while severe pouchitis with complications occurred only in UC patients. This is probably due to the inflammatory nature of UC compared to FAP. Patients with FAP may exhibit incomplete evacuation, dyschezia and increased bowel movement frequency and urgency33.
Postoperative quality of life has become an important measure of the functional outcome of RP-IPAA in patients with UC and FAP. Functional outcome has been reported to be significantly correlated with quality of life after surgery34,35. It has been observed that a considerable number of UC patients who underwent surgery enjoy a significant improvement in postoperative quality of life, with scores sometimes comparable to those of the general population, while the functional outcome in patients with FAP is usually considerably worse compared to preoperative function and to the general population36,37.
The expectations of patients after ileal pouch surgery recently reported in a Delphi consensus study represents the first patient-focused effort in the surgical literature that has sought to identify which functional outcomes patients consider important after pouch surgery, thus defining the amalgamation of symptoms that are specific to an ileal pouch29. The symptoms that previous studies focused on, such as faecal incontinence, spotting, excessive bowel movements and urgency, are important to patients. However, the cited consensus also highlighted several additional key symptoms that were not consistently reported in previous studies, including unpredictable bowel movements, altered patterns of bowel function (fragmentation, incomplete evacuation), nocturnal symptoms and perianal pain. The next challenge is to develop a clinically useful scoring system that can quantify the range and severity of symptoms experienced by patients after ileoanal pouch surgery and its correlation with quality of life parameters. This score would theoretically help to identify in which patients their pouch function symptoms will have a severe negative impact on their quality of life. The proposed score will help identify patients with ileal pouch syndrome who meet a designated threshold score and will also be able to assess the efficacy of medical and surgical interventions in improving quality of life in patients with ileal pouch syndrome. This initiative has received support from the Crohn's and Colitis Foundation and is currently ongoing29.
In this study, only 79 of the 115 patients (68.7%) who underwent RP-IPAA responded to our questionnaire. During the more than 20 years of follow-up since the first operated patient (1994), no significant differences were found between patients with UC or FAP in terms of long-term medication use, dietary restrictions or the average number of bowel movements during the day or night. Although we were unable to detect a significant difference in long-term functional outcomes between the two groups, the quality of life assessment was significantly higher in UC patients compared to FAP patients (86.7% vs 57.2%, p < 0.01). This is easily explained by the fact that most patients with FAP were usually asymptomatic or had minimal preoperative symptoms and normal bowel habits, and the indication for surgery was most often to detect multiple polyposis or for genetic counselling. Overall satisfaction with the surgical procedure was also significantly better in the group of UC patients.
The strength of this study lies in the significant number of patients who were operated on more frequently by only two surgeons and who have had long-term follow-up, while the limitations lie in its retrospective nature, where memory bias is important when filling out the form to assess satisfaction with the procedure, in addition to not having criteria for pouchitis activity or biochemical markers such as calprotectin from the start of the series.
In summary, when comparing the parameters studied between the two groups of patients who underwent RP-IPAA, the clinical course of these patients is very similar. However, inflammatory manifestations of the ileal pouch are more common in patients with UC than in those with FAP. This translates into a better acceptance of surgery and a better quality of life in UC patients over patients with ileal pouches due to FAP. Inflammation of the pouch did not lead to the appearance of more dysplasia or cancer in these patients.
ConclusionsRestorative proctocolectomy with ileal pouch-anal anastomosis provides more satisfactory quality of life and functional outcomes in patients with UC than in those with FAP. Pouchitis continues to be the most common complication, occurring in 61% of patients, with severe pouchitis occurring in 9.6%. This procedure was followed by a significant number of complications, but the number and severity of these have decreased in recent years, with better functional outcomes, a median of four to five bowel movements per day and a significant improvement in quality of life, especially in patients with UC. No cancer occurred in the pouch.
FundingNo funding was received for this study.
Conflicts of interestThe authors declare that they have no conflicts of interest.
This study was carried out with the support of the Proyecto sostenibilidad de la Vicerrectoría de Investigación de la Universidad de Antioquia, Colombia [Sustainability Project of the Research Vice-Rector of the University of Antioquia, Colombia].