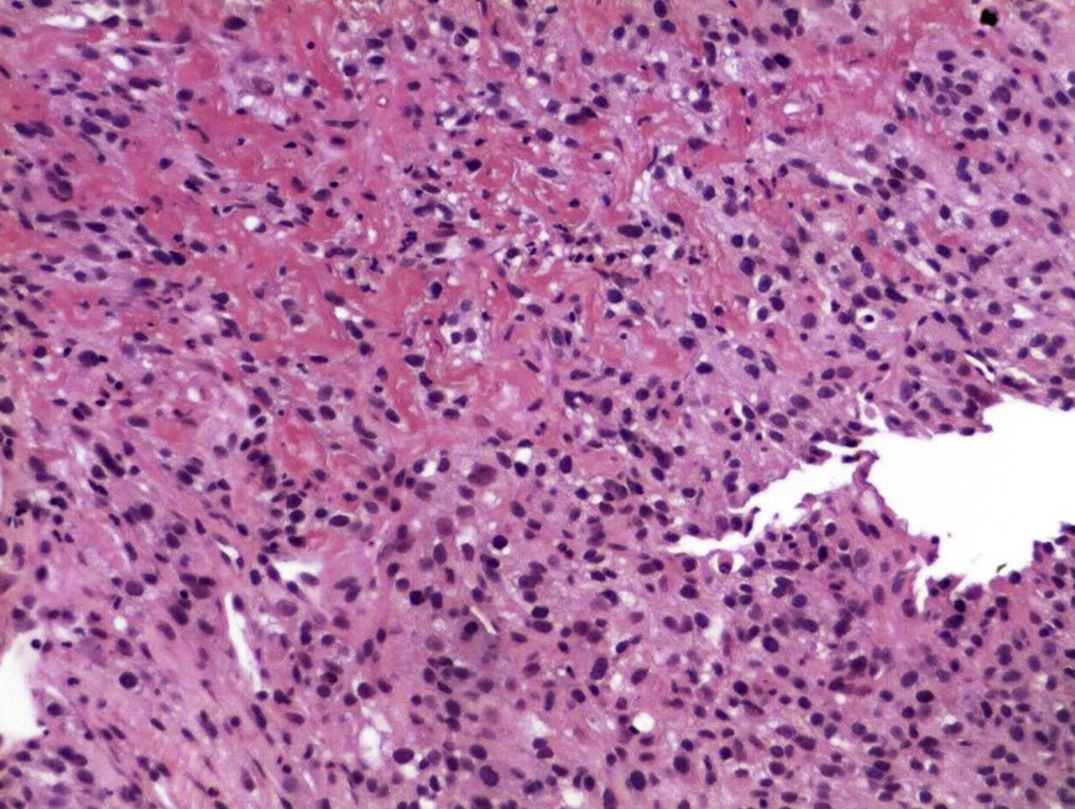
Renal cell carcinoma constitutes 3% of all neoplasms. At the time of diagnosis, 25% of patients have metastasis, reaching 51% in patients with nephrectomy.1 Metastasis presents in the gastrointestinal tract in 0.2–0.7%.2 There are few cases reported with metastasis of renal cell carcinoma to the duodenum, with the minority in women. The most common histology (75–85%) of these neoplasms are clear cells, with the sarcomatoid type variant being associated with poor prognosis.3 There are no reported cases of duodenal metastasis of clear cell renal cell carcinoma (CCRCC) with sarcomatoid differentiation, with this being the first case in a 48-year-old patient who came to the emergency department due to gastrointestinal tract bleeding.
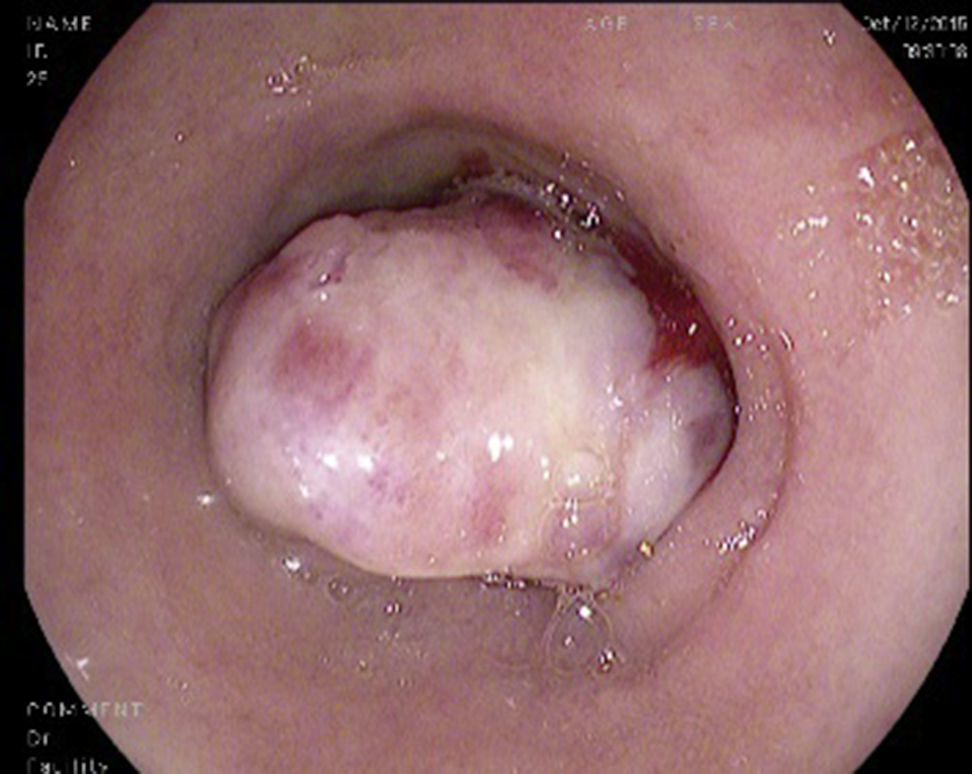
A 48-year-old woman with a history of chronic exposure to wood smoke 200h/year, high blood pressure for the past seven years, and nephrectomy one year prior to her admission due to CCRC carcinoma with sarcomatoid differentiation. She came in with symptoms of one-week evolution characterised by burning and sharp epigastric pain, haematemesis and melaena. At admission she had hypotension, tachycardia, and was febrile. Her admission analysis reported haemoglobin 6.5g/dl, thrombocytosis 797×103/mm3, leukocytosis 14.7×103/mm3 with neutrophilia of 12.9×103/mm3 and elevated C reactive protein of 27.8mg/l. An abdominal computed tomography (CT) was carried out, showing a mass in the second part of the duodenum, measuring 41mm×37mm×56mm. An endoscopy was performed, showing a 10cm tumour of neoplastic appearance in the second part of the duodenum, submucosal, with irregular and ulcerated surface with areas of haemorrhage, with 90% stenosis of the duodenal lumen (Fig. 1). The biopsy reported CCRCC with metastatic sarcomatoid differentiation (Fig. 2). The patient continued with gastrointestinal tract bleeding, requested voluntary discharge, and died one week later.
The most common metastasis locations for CCRCC are: lungs (75%), lymph nodes (36%), liver (18%), brain (8%) and skin (6%).4 It causes invasion in the gastrointestinal tract in less than 1%, and globally represents 7.1% of gastrointestinal tract metastases. Currently, only 30 cases have been reported in the medical literature on duodenal invasion.1
The majority of metastatic CCRCC cases in the gastrointestinal tract are reported in men, with a 1.5:1 ratio to women. Its incidence increases with age, with a mean of 60.7±14 years, with a high percentage of these occurring during the first year post nephrectomy as occurred in our patient, although there are reports of latency of up to 16 years.1 This means that onset has an unpredictable evolution. The majority of cases manifest as episodes of bleeding in the gastrointestinal tract, characterised by the presence of melaena, haematemesis, anaemia and even occlusion. Its dissemination types are: a) peritoneal, b) direct spreading from the neoplasm, c) haematogenous, and d) lymphatic; associated with the presence of parathyroid hormone-related protein.5
At the endoscopic level it manifests as single or multiple ulcerated submucosal masses of various sizes; in this case the patient had a 10cm diameter tumour with characteristics consistent with the above description.
CCRCC of the sarcomatoid type has been described as being associated with a poor prognosis, being described in this way in a series of cases that show the sarcomatoid type related to a decrease in survival and in the metastasis-free period, as well as to resistance to first-line treatment such as IL-2 in metastatic disease.3 This highlights the fact that the disease spreading on its own is ominous, even with the advent of new therapies, such as nivolumab.6 When there is duodenal invasion, the estimated survival time is less than one year. In the mentioned case, due to its complexity and the persistence of the bleeding, a surgical approach would have been difficult, although more conservative management such as an arteriogram with embolisation could have been done merely as a palliative measure due to the patient's poor prognosis.7
The importance of this case resides in it being the first reported case of CCRCC with sarcomatoid differentiation with metastasis to the duodenum. The majority of cases of duodenal invasion by CCRCC occur in men, with only 6 recorded cases in women. Thus, this shows an exceptional case that helps aid knowledge about the unpredictable behaviour of CCRCC and where in this case in particular, due to the presence of the sarcomatoid differentiation, there was a poor prognosis from the beginning.
CCRCC is a neoplasm that has difficult-to-predict behaviour and evolution where, despite treatment, there may be recurrences that can arise years after treatment, which makes us consider that it should be monitored more aggressively. When it metastasises in the gastrointestinal tract, the short- and mid-term prognosis is poor. The sarcomatoid differentiation worsens the prognosis even more.
Please cite this article as: Villela-Segura U, García-Leiva J, Nuñez Becerra PJ. Metástasis a duodeno de cáncer renal de células claras con patrón sarcomatoide: reporte de caso. Gastroenterol Hepatol. 2017;40:530–532.