Casos Clínicos en Gastroenterología y Hepatología
Más datosSevere Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection can present several gastrointestinal manifestations.1,2 Cases of acute pancreatitis (AP) have been reported in patients with severe respiratory manifestations associated to SARS-CoV-2.3 However, there are few publications of AP as the main manifestation of infection.4 Also, the period between SARS-CoV-2 infection diagnosis and AP presentation and the role of possible risk factors are not well established.1
We report two cases of AP as the main manifestation of SARS-CoV-2 infection with different presentation after infection diagnosis.
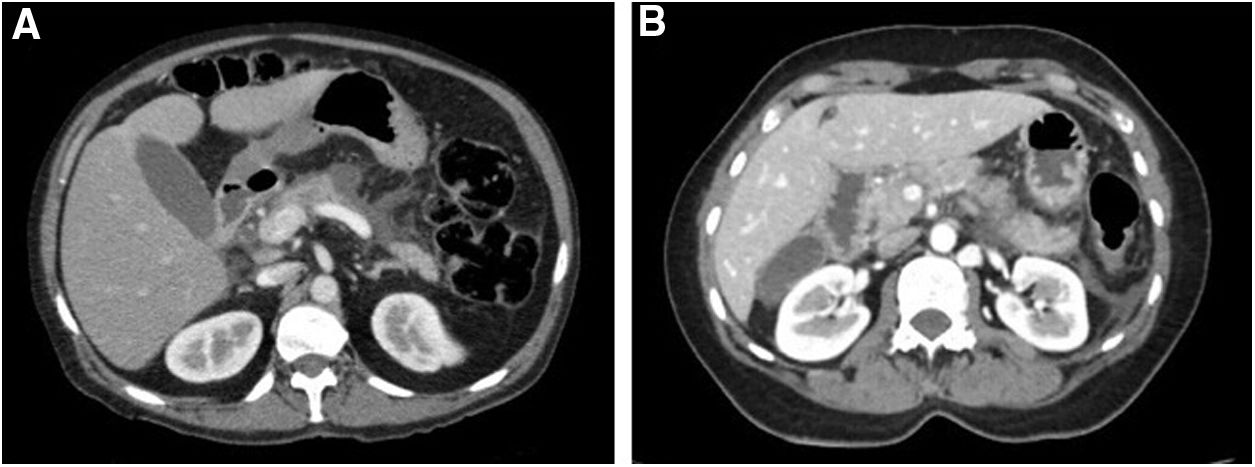
Case 1A 42-year-old woman with no medical history (including no history of previous AP), toxic habits or medication was admitted for severe epigastric pain associated with vomiting of 24h of evolution. On physical examination, she was afebrile and presented diffuse abdominal pain. Laboratory test showed amylase 2263U/L, lipase 2799U/L, C-reactive protein (CRP) 4.21mg/dl and leukocytes 14.7k/μl. Liver enzymes on admission and throughout hospitalization as lipids and calcium values were also normal. A nasopharyngeal swab for SARS-CoV-2 performed at the emergency department was positive. Abdominal computed tomography (CT) showed AP with Balthazar score D (Fig. 1A). A magnetic resonance cholangiopancreatography (MRCP) showed no abnormalities in the biliary and pancreatic tract. The final diagnosis was a moderately severe AP associated to SARS-CoV-2 infection.5 She presented an uncomplicated hospitalization and was discharged 9 days after admission.
Case 2A 65-year-old active smoker (20 cigarettes/day) woman with history of type 2 diabetes and asthma was diagnosed with asymptomatic SARS-CoV-2 infection due to a close contact. She denied intake of alcohol, toxics or new medications and history of AP. She remained at home and 13 days after diagnosis she was admitted to emergency department due to severe epigastric abdominal pain and vomiting. She denied fever and dyspnea. On examination, the patient was afebrile and presented epigastric pain. Laboratory tests showed amylase of 470U/L, lipase 1950U/L, CRP 4.92mg/dl and leukocytes of 13.3k/μl. Evaluation of liver enzymes, lipids, serum immunoglobulin G4 and calcium were within normal limits. A chest CT scan showed normal findings. Abdominal CT showed signs of AP with Balthazar score C (Fig. 1B). MRCP showed a normal gallbladder and absence of abnormalities of bile or pancreatic ducts. The patient presented an uncomplicated hospitalization for moderately severe AP without developing respiratory symptoms and was discharged 8 days after admission.5
Different series have shown that about 10% of patients with severe SARS-CoV-2 pneumonia may present elevated pancreatic enzymes or AP.4 However, in some studies only the increase in pancreatic enzymes was evaluated without considering the presence of characteristic abdominal pain or imaging findings.1 In the present cases, AP was considered according to the Atlanta classification including clinical, laboratory and radiological criteria.5 Differently from the present reported cases, a great proportion of cases of AP related to SARS-CoV-2 infection published were of mild severity and in the context of a moderate-severe respiratory involvement of thoracic CT exams.3,4
Both patients had no history of AP and the etiological study was negative for gallstones, toxics, high values of triglycerides or calcium, or trauma. Furthermore, none of the patients had previously consumed any medication other than their usual medication. A limitation of the present report is that endoscopic ultrasound was not available, therefore microlithiasis cannot be fully excluded as etiology. However, this cause is unlikely as liver enzymes were normal during admission and MRCP did not show biliary abnormalities.
AP was presented at the same time of SARS-CoV-2 infection diagnosis in one case. In the other case, AP was diagnosed almost at the second week of the infection, which was asymptomatic until that moment. This difference could be due to other unknown mechanisms, as active smoking, that may present a role on the development of AP in the context of SARS-CoV-2 infection.
In conclusion, we report two cases of AP as the main manifestation of SARS-CoV-2 infection with a different temporal relationship between the infection and the clinical presentation of AP. In this current epidemiological context, all patients admitted for a diagnosis of AP should be evaluated for SARS-CoV-2 infection, regardless of the presence of fever or respiratory symptoms.
Authors’ contributionRicardo Ame and Domingo Balderramo wrote the manuscript. Both authors approved the submitted version.
FundingThe present manuscript was performed without any financial support or grant.
Conflict of interestNone of the authors have any potential conflicts (financial, professional, or personal) to disclosure.