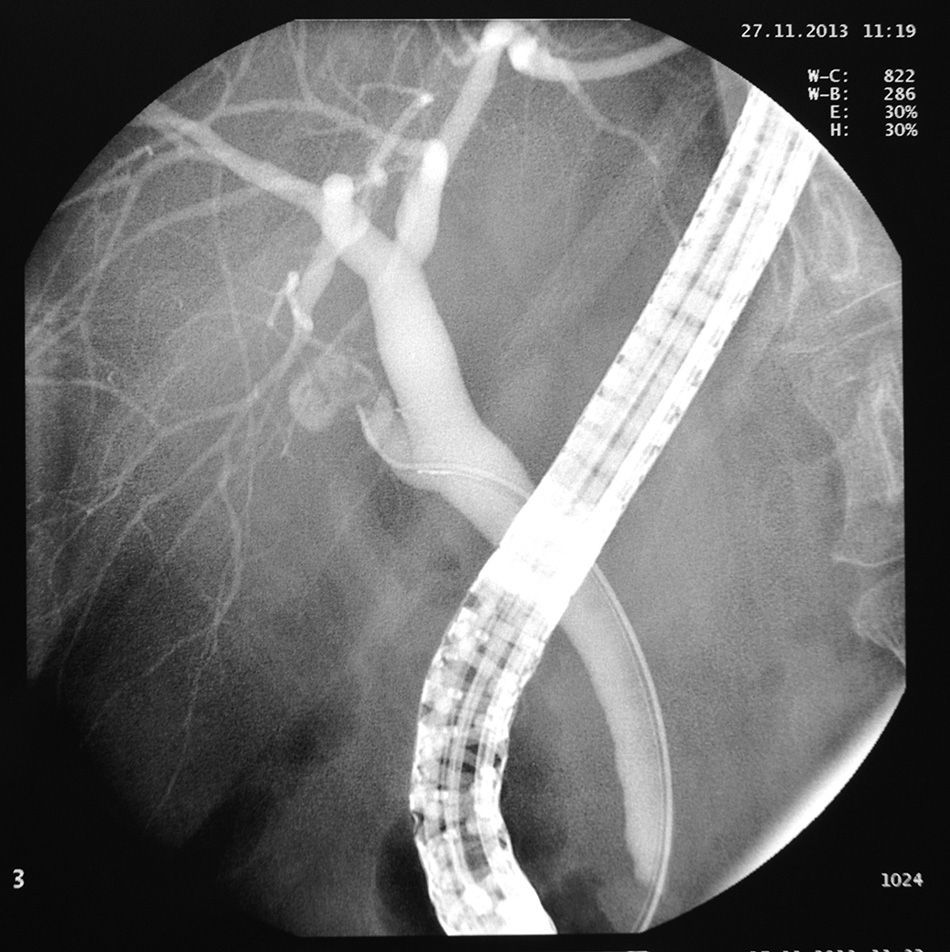
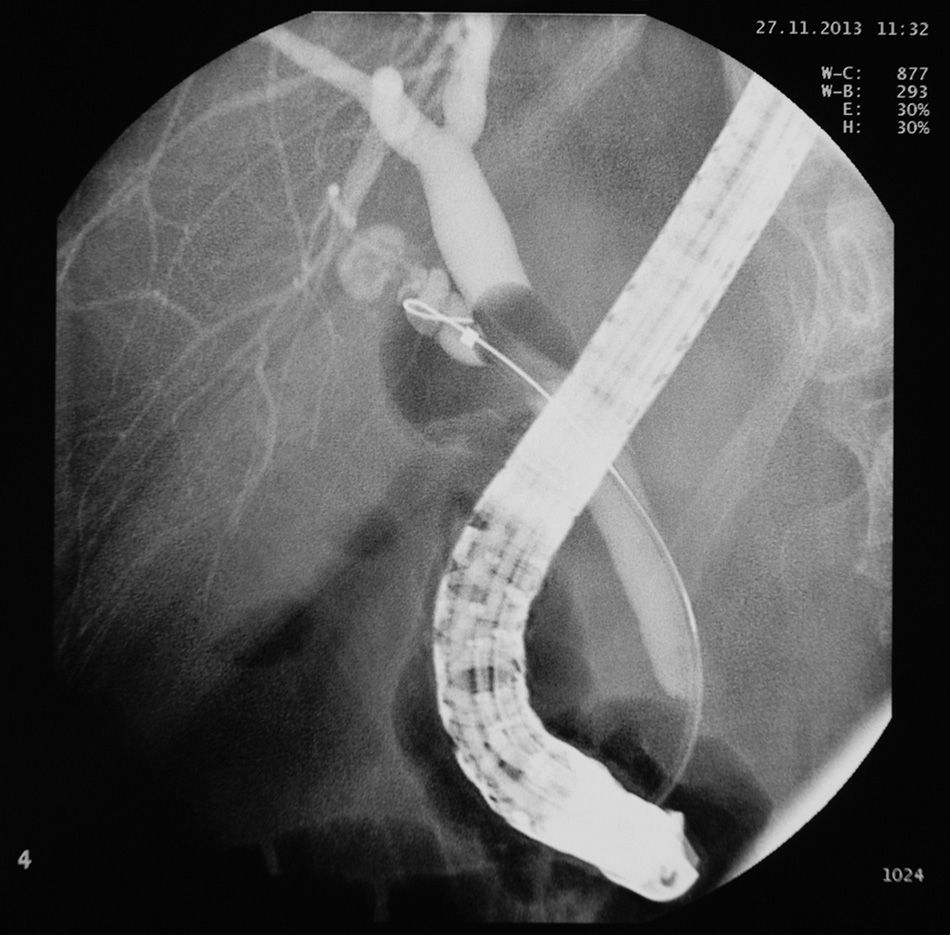
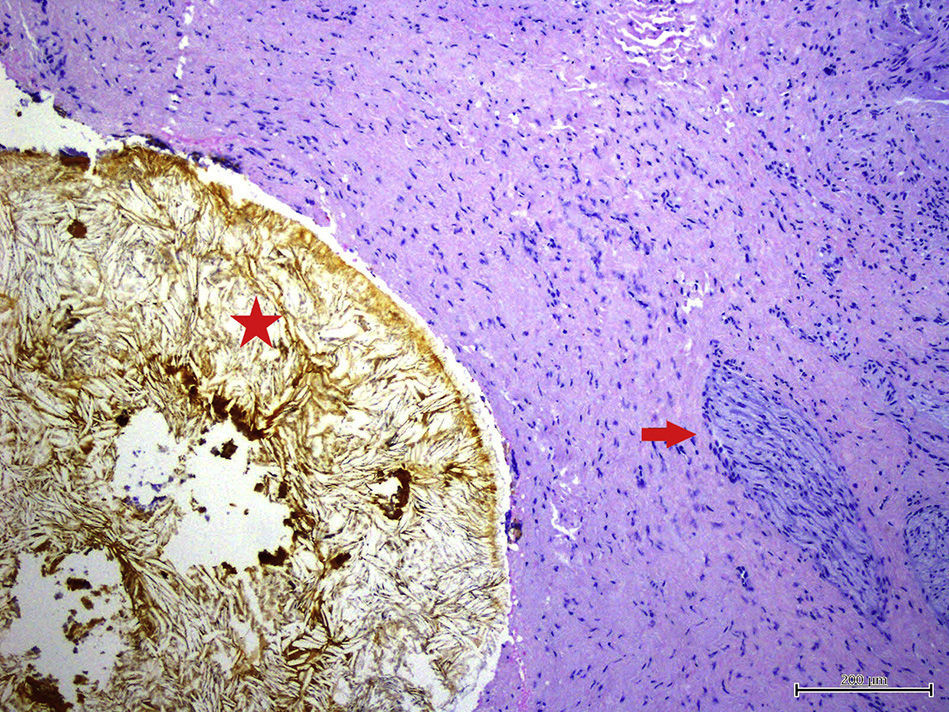
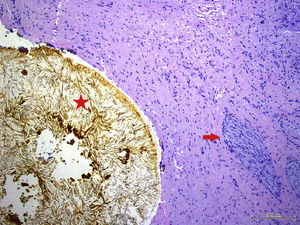
We present the case of a 59-year-old woman, with no history of interest, except for surgery for biliary colic 7 years previously in another hospital, where she underwent laparoscopic cholecystectomy converted to open surgery. She was seen for recurrent episodes of colicky pain in the last few months, occasionally related with eating, which began in the back and radiated to the right epigastrium and hypochondrium, with an accompanying vagal reaction. Initially suspecting a biliary rather than gastroduodenal origin, blood tests with liver profile, ultrasound and gastroscopy were performed, all of which were normal. Due to the persistence of symptoms, biliary magnetic resonance cholangiography (MRC) was performed to rule out biliary anatomical abnormalities and residual choledocholithiasis, with normal findings. The study was completed with endoscopic ultrasound (EUS), observing a cystic duct stump of around 15mm in length with a hyperechoic arciform structure with posterior acoustic shadowing measuring 4–5mm in diameter in the proximal portion, with local inflammatory signs and cystic wall thickening (1.5mm). In view of these findings and the suspicion of cystic duct remnant syndrome (CDRS), it was decided by consensus with the general surgery department to attempt calculus removal by endoscopic retrograde cholangiopancreatography (ERCP). In this procedure, a Fogarty balloon probe is passed through the endoscope to pressure-inject contrast medium into the cystic duct remnant. Calculi were not initially observed in the stump, but after filling the entire structure with contrast medium following guide wire cannulation, the presence of an irregular filling defect at proximal level of at least 5–7mm in diameter was confirmed; however, endoscopic extraction was not possible (Figs. 1 and 2). Open surgery was then performed, finding a cystic duct stump embedded in a fibrotic mass in the gallbladder resection bed; the stump was mobilized and opened, revealing calculi within, and the cystic remnant was resected (Fig. 3). The patient progressed satisfactorily and currently remains asymptomatic.
It is currently estimated that between 5% and 40% of patients who undergo cholecystectomy can present episodes of abdominal pain. These can be similar to the symptoms that led to this indication, or appear after the intervention, and are grouped under the term “post-cholecystectomy syndrome” (PCS).1 As this syndrome tends to become chronic and therefore extremely costly in terms of healthcare resources, a good diagnostic approach is crucial.
The aetiology of this syndrome is very diverse, and it can be secondary to biliary causes (organic and functional), such as residual choledocholithiasis, bile duct stenosis or leakage, neuroma in the scar tissue, biliary dyskinesia and Oddi sphincter dysfunction, among others. It is also essential to assess extra-biliary diseases not suspected before the surgery.2 CDRS is one of the least common organic biliary disorders, with a prevalence of less than 2.5% in patients who have undergone cholecystectomy.
The cystic duct remnant is defined as a residual cystic duct greater than 1cm in length, which in the presence of calculi may produce symptoms.3 CDRS can present in the immediate postoperative period or even years after surgery. Its clinical presentation can mimic biliary colic produced by distension of the cystic remnant, sometimes accompanied by abnormal liver function tests and/or biliary obstruction.
It is important to note that the increasingly widespread use of laparoscopic gallbladder surgery has led to an increase in iatrogenic bile duct injuries. Most bile duct injuries are due to poor interpretation of the anatomy, as well as the presence of anatomical variants. The prevention of CDRS should be based on proper dissection and anatomical identification of the junction of the cystic and bile ducts.
The main diagnostic element in PCS is a good anamnesis and medical history, investigating previous symptoms and indication for the cholecystectomy, as well as details related with the procedure. Extra-biliary causes including irritable bowel syndrome, gastro-oesophageal reflux, peptic ulcer and chronic pancreatitis must first be ruled out, as these are the most common causes of PCS. The aforementioned organic and functional biliary abnormalities should then be assessed. Full laboratory tests should be carried out, including liver profile, and when symptoms persist, complementary tests such as ultrasound and computed tomography should be done. When there is high suspicion of aetiology secondary to biliary abnormalities, MRC is the non-invasive technique of choice for evaluation of the biliary tree.4 An alternative to this is endoscopic ultrasound, which is basically more sensitive for the detection of choledocholithiasis <5mm, with ERCP relegated to a strictly therapeutic technique.5
Once extra-biliary causes have been ruled out, and with compatible symptoms and imaging tests showing a long cystic remnant containing calculi, the diagnosis of CDRS should be made.
The therapeutic approach includes ERCP with sphincterotomy and possible stent placement to aid drainage of the main bile duct, together with definitive surgical treatment by resection of the bile duct remnant. This should be indicated in patients with recurrent symptoms and evidence of residual calculi in the remnant.6,7 The laparoscopic approach would be ideal, but the existence of fibrotic changes between the remnant and main bile duct can increase the risk of iatrogenic injury with respect to open surgery.8 Resection of the remnant seems to resolve symptoms in most cases. Another alternative to surgical and endoscopic treatment is extracorporeal shock wave lithotripsy, which has been successful in some published studies.9
Conflict of interestsThe authors declare that they have no conflict of interests.
Please cite this article as: Ruiz-Clavijo García D, Vila Costas J, Prieto Martínez C, Elizalde Apesteguía I, Tarifa Castilla A, Mercado Gutiérrez M, et al. Síndrome del muñón cístico como causa de síndrome poscolecistectomía. Gastroenterol Hepatol. 2016;39:722–724.