Idiopathic adulthood ductopenia (IAD) is a rare disease whose etiology is not known. It is a chronic cholestatic liver condition which appears at an adult age; in which there is loss of bile ducts in more than 50% of portal tracts.1 Several conditions are associated with a decrease in the number of intrahepatic bile ducts of small and medium size. Some result in development failure and others are disorders that lead to acquired ductopenia, some of which are associated with destruction of the bile duct epithelium and for others there is no apparent inflammatory process.2,3
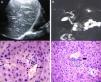
A male, 20 years old, previously healthy, with no history of jaundice at birth or in childhood, denies alcoholism, smoking or other addictions, no previous use of drugs or herbal products, was referred to the Mexico's General Hospital with symptoms of 6 months of evolution characterized by fatigue, weakness, itching, routine laboratory tests were performed finding persistent cholestasis. Physical examination was normal, with no stigmata of chronic liver disease. The laboratory tests showed Total Bilirubin (BT) 0.8mg/dL (0.3–0.9mg/dL), alkaline phosphatase (ALP) 618U/l (44–147U/L), Gamma glutamyltranspeptidase (GGT) 912U/l (40–78U/L), aspartate aminotransferase (AST) 213U/L (8–40U/L), alanine aminotransferase (ALT) 433U/L (7–33U/L). Viral Hepatitis Panel for B, C and HIV were performed and were negative. Serologic tests for anti-nuclear, anti-mitochondrial, anti-smooth muscle, anti-LKM1 antibodies were negative. The ceruloplasmin and copper in 24-h urine were normal. An abdominal ultrasound performed showed no abnormalities in liver morphology, portal vein and hepatic permeable, unaltered hepatic artery, without dilatation of the intrahepatic or extrahepatic bile ducts. The CPMRI was unaltered. Percutaneous liver biopsy was performed reporting: preserved liver architecture, sparse chronic inflammatory infiltrate, bile duct not observed in over 50% of portal tracts observed (see Fig. 1).
Ultrasonographic and CPMRI examinations. (A) Liver ultrasound: unchanged liver morphology. (B) CPMRI showing anormal bile ducts. (C, D) Histologic findings on liver biopsy specimen with Hematoxylin–eosin and PAS staining respectively demonstrate that branches of the hepatic artery (white arrow) and portal vein (black arrow) are present in the portal tract, but interlobular bile ducts are absent. There is a mild lymphocytic inflammatory infiltrate (thick arrow).
The patient was diagnosed with idiopathic adult ductopenia, treatment was started with a dose of ursodeoxycholic acid (13–15mg/kg/day) 250mg every 12h, mild improvement in symptoms and liver function tests was observed after 6 months of treatment (see Table 1).
Evolution of Liver function test profiles (LFT), at the beginning of treatment and during follow-up at 3, 6 and 12 months.
| LFT | Diagnosis | Beginning of treatment | 3 months | 6 months | 12 months |
| TBIL (mg/dL) | 0.8 | 0.7 | 0.7 | 0.7 | 0.7 |
| ALT (UI/L) | 433 | 420 | 380 | 312 | 300 |
| AST (UI/L) | 213 | 210 | 190 | 189 | 189 |
| ALP (UI/L) | 618 | 630 | 600 | 558 | 500 |
| GGT (UI/L) | 912 | 950 | 920 | 870 | 820 |
TBIL, total bilirubin; ALT, alanine aminotransferase; AST, aspartate aminotransferase; ALP, alkaline phosphatase; GGT, gamma glutamyl transpeptidase.
Ductopenia describes the loss of septal and interlobular bile ducts for any reason with the possibility of the development of biliary cirrhosis or hepatic insufficiency.4 However, there have been several clinical cases of non-progressive IAD.1 The most common causes of chronic cholestasis are primary biliary cirrhosis diseases (PBC) and primary sclerosing cholangitis (PSC), in 90% of cases, representing the IAD in only 1% of cases.5–7 In IAD there may be evidence of ductopenia in the biopsy, but there are no clinical, biochemical or serological findings indicating a specific cause.2 It affects young adults, with a male predominance3 with an average year of appearance at 30 for men and 26 for women.5,6 The current diagnostic criteria include biochemical cholestasis and histopathological evidence of ductopenia in the absence of primary sclerosing cholangitis or inflammatory bowel disease.4,8 The diagnosis must be made on the loss of septal or interlobular bile ducts in at least 50% of portal tracts, to be considered significant, at least 20 or more portal tracts, and the absence of granulomatous cholangitis or a florid duct lesion.4,9 The clinical course is variable, some patients may be asymptomatic, other patients may have episodes of jaundice and itching and with elevated serum liver enzymes. Two types of IAD have been recognized, each with different prognosis, the patients who develop type 1 are asymptomatic or manifest symptoms of chronic cholestatic disease, tend to have less destruction of bile ducts in liver biopsy specimens. In contrast with type 2 where patients can have initial symptoms of decompensated biliary cirrhosis, extensive destruction of intrahepatic bile ducts can be found, and liver biopsy is often required.9 In a review of 25 patients with the diagnosis of IAD, it was found that bilirubin levels could be up to 26mg/dL, the ALP and GGT values ranged from 3 to 16 and 14 times the normal upper limit respectively, and the levels of aminotransferases could vary from normal to an elevation of 10 times the upper limit.4,10 In about half the cases reported the IAD appears to have a benign course, while the rest of the IAD were mortal or merited liver transplantation.3
Although the cause has not been determined, several hypotheses have been made, such as, that the destruction of the bile ducts is caused by an unknown virus or a toxic metabolite. Host factors may contribute to susceptibility to developing the disease, in a study by Garcia-Jimenez et al. with genes HLA-DR, no significant association between HLA-DRB1 alleles and disease was found, but suggests that IAD may have immunogenetic basis in its development.9 The degree of ductopenia is variable, when it is mild, it may be overlooked during histopathology.2
The IAD is a rare disease, with unknown pathogenesis and evolution. The uncertainties about the etiology preclude a specific treatment; in a non-aggressive disease (type 1 IAD) ursodeoxycholic acid (UDCA) can be used for treatment. A beneficial effect has been suggested but it is unknown its effect on disease progression.4,6 Sometimes only liver transplantation offers a cure, especially in cases where cholestatic symptoms are intractable like the severe itching or when there are symptoms of liver failure.5,6
In conclusion, it would be important to perform a research to identify possible causes and pathogenesis of the disease, to predict the likely clinical course, and to offer appropriate treatment according to the presentation of the IAD.
Conflict of interestThe authors have no conflict of interest to declare.
Eduardo Perez Torres, M.D., Chief of Gastroenterology Division and Gerardo Aristi Urista, M.D., Pathology Department.