The 3rd International Nursing & Health Sciences Students & Health Care Professionals Conference (INHSP) 2019
Más datosThis study identified the risk of diabetic foot complications among type 2 diabetes mellitus patients and their relationship with the patients’ characteristics.
MethodsThis cross-sectional study examined 93 diabetic patients. Participants included in this study were age more than 20 years old, diagnosed with diabetes mellitus type 2, and has no diabetic ulcer. A questionnaire based on the International Working Group on Diabetic Foot guidelines was used to measure diabetic foot complications. The statistical testing was using the Chi-square test.
ResultsThis study found that 53 participants (57%) are at risk of diabetic foot complications. Age and duration of diabetes variables had a significant relationship with the diabetic foot complication (p<0.005), while gender did not have a significant relationship with diabetic foot complications (p>0.005).
ConclusionHalf patients are at risk of diabetic foot complications, and it is related to the patients’ age and duration of suffering diabetic.
Diabetes mellitus (DM) type 2 is the most common category of diabetes in adulthood or adult-onset diabetes, which is characterized by high blood sugar levels.1 Risk factors of diabetic foot complications are part of serious and long-lasting complications that have the potential to threaten the lives of the patients, affecting the community economy, and pathogenetically associated with peripheral neuropathy.2 Diabetic foot is prevalent in type 2 diabetes mellitus.1,3,4 Neuropathy is a common symptom characterized by paresthesia/numbness in the legs, tingling, and broken skin due to poor circulation. The risk of foot disorders in people with diabetes increased mainly due to diabetic neuropathy (nerve damage) or peripheral arterial disease (disturbance in the large blood vessels in inadequate supply), which are at risk for foot repair if prevention and care action is not performed well by patients.1,5–7 The management of foot care is done through the approach of individual awareness to behave properly.8 The training and coaching activities are also a form of behavioral approach in enhancing glycemic control in people with diabetes to minimize complications.9
Globally, an estimated 371 million people aged between 20 and 79 years suffer from diabetes mellitus.6 Diabetic foot is a major complication of diabetes that lasts in a long time, is estimated affecting around 35% of all diabetic clinic hospitals, and causing about 80% of the lower-limb non-traumatic amputation.2 Regarding the peripheral neuropathy symptom of diabetic foot complications, it is estimated that 50% is asymptomatic; therefore, foot treatment is very essential.7 The prevalence of neuropathy is estimated to be around 8% in newly diagnosed patients, and more than 50% in patients with long-term disease.4 The peripheral neuropathy is a significant contributor to the worsening ischemia, including foot ulceration in patients with Peripheral Occlusive Arterial Disease (PAOD). Studies on 52 limbs with PAOD display 82.7% prevalence of peripheral neuropathy and 23.1% prevalence of peripheral neuropathy ischemia. The study also shows that the risk factors for ischemia can be displayed according to time and injury/gangrene.10 The increased incidence of diabetic foot is influenced by several factors such as age, sex, and duration of diabetes.3 Significant risk factors for peripheral neuropathy and peripheral vascular disease (PVD) are male sex, low education, increased duration of diabetes, hypertension, and type 2 diabetes mellitus.11
Previous studies have shown that the prevalence of diabetic foot complications increases with age, duration of diabetes, and sex. Diabetic foot complication is more often seen in patients with type 2 diabetes mellitus, more than 10 years of suffering from diabetes mellitus, patient age higher than 45 years, and male sex.3,11 Therefore, the study identifies the risk of diabetic foot complications among type 2 diabetes mellitus patients and their relationship with the patients’ characteristics.
MethodsDesign and participantsThis study was a quantitative non-experimental study using a cross-sectional. The measurement of variables is conducted at a one-time point.12 Participants were the type 2 diabetes patients in three Public Health Center in Kendari City, Indonesia, in 2018. Ninety-three patients diagnosed with type 2 diabetes participated in this study. The data of the targeted participants were obtained from the medical records of Puskesmas in the city of Kendari. The participants’ recruitment process used a purposive sampling method. In this study, the sampling was conducted continuously until the sample size is met according to the criteria. The inclusion criteria of the study were participants; aged more than 20 years old, diagnosed with type 2 diabetes with fasting plasma glucose (FPG) ≥126mg/dL or 2-hour plasma glucose (2-h PG) ≥200mg/dL, has no diabetic ulcer, and willing to be a participant. The diabetes mellitus criteria are referring to the criteria of the American Diabetes Association (ADA).13
Research instrumentsThis research uses an instrument in the form of an observation sheet containing demographic data of the participants; age, sex, occupation, education, duration of diabetes, and marital status. The research variables on diabetic foot complications use risk assessment guidelines for the International Working Group on Diabetic Foot (IWGDF).
The risk assessment for diabetic foot complications according to the IWGDF guidelines is divided into three categories: (1) category 0 means no neuropathy, and no POAD (peripheral arterial occlusive disease), (2) category 1 means peripheral neuropathy, no POAD and no deformity, (3) category 2 means peripheral neuropathy, deformity, POAD and or deformity (divided in 2, category 2A: peripheral neuropathy and deformity, whereas category 2B: category 2A+POAD), (4) category 3 means peripheral neuropathy, deformity, POAD and wound history foot or lower limb amputation (divided into two categories 3A: peripheral neuropathy, deformity, POAD, history of injury; whereas category 3B: category 3A with history of lower extremity amputations)14. Participant's category 1, 2, and 3 were classified at risk of foot complications, while participants category 0 was classified as no risk.
Data collectionIn this study, researchers conducted data collection by recruiting patients diagnosed with type 2 diabetes based on inclusion criteria through 2 stages. In the initial stage, the researcher introduces himself and explains the purpose, then followed by the signing of the informed consent for participants who are willing to become participants. In the second stage, the researchers began to fill out the observation sheet related to the demographics of the participants, then examined the signs of diabetic foot complications, and the results were recorded on the sheet. For the examination of leg complications, the researchers used the Ipswich Touch Test (IpTT) technique to detect diabetic feet against neuropathy as well as palpate dorsalis pedis and posterior tibial arteries to detect ischemia (angiopathy). For the detection of neuropathy, the researcher is to touch the toes (1st, 3rd, and 5th fingers) and then the patient is asked to show when they feel the touch, while for the detection of ischemia (angiopathy) by palpating the pulses of the dorsalis pedis and posterior tibial arteries. Ipswich Touch Test (IpTT) is a standard neuropathy screening tool that is reliable and ready to be used to detect risky feet.15 One study recommends that the use of IpTT as a screening test to detect sensory loss is done by placing the index finger on the first, third, and fifth fingertips and asking the patient to show when he feels the touch.16 Bilateral palpation of an examiner in the femoral artery, posterior tibialis, and dorsal pedis is a subjective criterion, which is when the pulse less than three is considered abnormal or shows symptoms of peripheral arterial disease.17
Data analysisAfter the researchers collected data from participants, further data analysis was performed. Data analysis was performed in two forms. First, the researcher gives an overview of all variables in the form of frequency distributions. The second is to conduct a test and statistical analysis of several variables related to diabetic foot complications in terms of age, sex, and duration of diabetes. Statistical tests are using Chi-square and phi coefficient statistical analysis. Chi-square test is used to find the relationship between variables between the two variables. The Phi coefficient analysis is used to answer the research question regarding the existence of a relationship between two variables in the form of nominal data.12
Ethical considerationThe ethical clearance for this study was obtained from the Ethical Committee for Health and Medical Research of Hasanuddin University (Number: 184/H4.8.4.5.31/PP36-KOMETIK/2018). A written agreement was also obtained from participants who were willing to participate in this study.
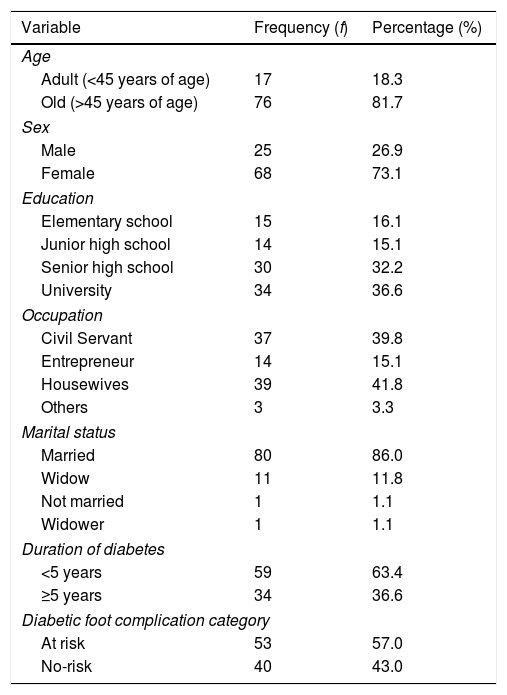
ResultsThe total number of participants is 93 patients. Most of them are elderly (aged more than 45 years old) (81.7%). About 57% of participants are at risk of diabetic foot complications. The characteristics of the participants are presented in Table 1.
Characteristics of the participants (n=93).
| Variable | Frequency (f) | Percentage (%) |
|---|---|---|
| Age | ||
| Adult (<45 years of age) | 17 | 18.3 |
| Old (>45 years of age) | 76 | 81.7 |
| Sex | ||
| Male | 25 | 26.9 |
| Female | 68 | 73.1 |
| Education | ||
| Elementary school | 15 | 16.1 |
| Junior high school | 14 | 15.1 |
| Senior high school | 30 | 32.2 |
| University | 34 | 36.6 |
| Occupation | ||
| Civil Servant | 37 | 39.8 |
| Entrepreneur | 14 | 15.1 |
| Housewives | 39 | 41.8 |
| Others | 3 | 3.3 |
| Marital status | ||
| Married | 80 | 86.0 |
| Widow | 11 | 11.8 |
| Not married | 1 | 1.1 |
| Widower | 1 | 1.1 |
| Duration of diabetes | ||
| <5 years | 59 | 63.4 |
| ≥5 years | 34 | 36.6 |
| Diabetic foot complication category | ||
| At risk | 53 | 57.0 |
| No-risk | 40 | 43.0 |
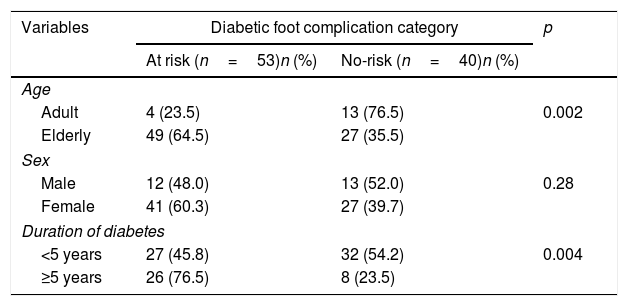
Table 2 presented that in terms of age the most elderly age categories have at-risk feet (64.5%), based on the most sexes, the female sex has the most at-risk of diabetic foot complications (60.3%) and based on the duration of diabetes, more respondents are in the category of foot complications with no-risk status for the people with diabetes <5 years (45.8%). Based on the results of the statistical analysis of the phi coefficient, it shows that the age and duration of diabetes variables have a significant relationship with diabetic foot complications in people with diabetes (p<0.005). In contrast, gender does not have a significant relationship (p>0.005).
Relation between age, sex, and duration of diabetes with the diabetic foot complication (n=93).
| Variables | Diabetic foot complication category | p | |
|---|---|---|---|
| At risk (n=53)n (%) | No-risk (n=40)n (%) | ||
| Age | |||
| Adult | 4 (23.5) | 13 (76.5) | 0.002 |
| Elderly | 49 (64.5) | 27 (35.5) | |
| Sex | |||
| Male | 12 (48.0) | 13 (52.0) | 0.28 |
| Female | 41 (60.3) | 27 (39.7) | |
| Duration of diabetes | |||
| <5 years | 27 (45.8) | 32 (54.2) | 0.004 |
| ≥5 years | 26 (76.5) | 8 (23.5) | |
p, probability using Chi-square test.
Patients with diabetes mellitus (DM) in Kendari city are still in the high enough category, including the incidence of diabetic foot complications, wherefrom the data obtained, the category of at-risk feet is almost 60%. This is due to the majority of patients diagnosed with diabetes already have diabetes, on average, over five years. Diabetes mellitus is classified as a chronic disease with a high prevalence and various complications such as diabetic foot, which can paralyze and create a burden on health, including an impact on the economy of the family and society.2 Type 2 DM sufferers generally experience hazardous microvascular chronic complications that contribute to diabetes neuropathy and have considerable potential for amputation.18 The symptoms of neuropathy are one of the signs of the diabetic foot, including ischemia and infection.19 Neuropathy, which is a common symptom of the diabetic foot, is characterized by symptoms of loss of sensation in the feet and tingling, whereas symptoms of reduced circulation (ischemia) can cause pain, skin discoloration, including deformity.20 An increase in diabetic foot complications such as PAD is more often seen in people with type 2 diabetes, generally occurs along with the increasing age of the patient, duration of diabetes, as well as gender.3,11
The results of the study show that the age category of the elderly is associated with an increased risk of diabetic foot complications. The longer the patient's diabetes duration, the higher the likelihood he will be experiencing peripheral arterial disease, which will result in inadequate supply so that the foot is at risk for injury.6,7 Peripheral arterial disease and diabetic neuropathy attack 1 in 3 diabetics over 50 years of age.5 A study of 500 diabetic patients found that 55 patients suffered diabetic foot complications with an average age of 55 years.21 Another study found that people aged 50–59 years of diabetes had the highest percentage of peripheral neuropathy (36.2%) followed by age >60 years as much as 29.1%, whereas for complications of peripheral vascular disease (PVD) were more prone for people aged >60 years old (54.2%).11 Another study that as many as 74 patients, of which 20 patients with peripheral neuropathy, with an average age of 65 years.17
Furthermore, this study also found that most patients who at risk of diabetic foot complications suffered diabetic for more than five years. Long-suffering from diabetes can increase the risk of diabetic foot complications in patients with type 2 diabetes.22 Diabetic foot is more often seen in patients with type 2 DM with 10 years suffering from diabetes.3 Factors of long-standing diabetes with a duration of >5 years are associated with significant complications in diabetics’ feet as well as neuropathy that leads to ulcers if treatment is not optimal.23 A study that long duration of diabetes can increase the risk of peripheral neuropathy, the results of his study showed that of 513 participants, 39% experienced peripheral neuropathy, and increased duration of diabetes mellitus was associated with peripheral neuropathy.11 Another study that patients with ulcers with PVD showed a significant correlation with the duration of diabetes.17
This study revealed that the risk of diabetes feet has the potential to occur in both male and female sexes. A previous study reported that the ratio of diabetics in men and women with diabetes was 5.8:1.21 Another study concluded that long-suffering from diabetes could increase the risk of peripheral vascular disease, wherein people living with diabetes with male sex are associated with risk factors for peripheral vascular disease, i.e., out of 513 peripheral neuropathy participants sufferer, 59.3% are male, including complications of vascular disease peripheral blood (74.6%).11 In another study of 188 participants (45 men and 143 women), women had more percentages of PVD complications (19.1%). The results of the statistical analysis of PVD diabetic foot complications had a significant relationship with gender. While for peripheral neuropathy complications, the percentage is higher in the male sex. Male and female genders did not show a significant relationship to the major complications of diabetic foot (amputation, ulcer, and infection).23
ConclusionHalf patients are at risk of diabetic foot complications, and it is related to the patients’ age and duration of suffering diabetic. Nurses must provide appropriate interventions to type 2 diabetes patients to prevent diabetic foot complications, particularly for older patients and those who suffered diabetes for more than five years.
Conflict of interestThe authors declare no conflict of interest.
Peer-review process of the 3rd International Nursing & Health Sciences Students & Health Care Professionals Conference (INHSP) 2019 is under the responsibility of the scientific committee of the 3rd International Nursing & Health Sciences Students & Health Care Professionals Conference (INHSP).