This study aims to determine the relationship of nurses’ knowledge and attitudes with nurses’ behavior in providing spiritual nursing care in the inpatient room at Citra Sari Husada Hospital, Karawang.
MethodThis study used an analytic descriptive design with a cross-sectional approach with a population of 115 and the sample used was 85 people. Data were collected by distributing questionnaires. Questionnaires were used assess about nurses’ knowledge, nurses’ attitudes, and nurses’ behavior in providing spiritual nursing care.
ResultsThe results of bivariate analysis found a relationship between knowledge and behavior of nurses in the provision of spiritual nursing care with p value 0.010 (α=0.05). But there is no relationship between attitudes with nurses’ behavior in providing spiritual nursing care with p value 1.000 (α=0.05).
ConclusionNurses’ knowledge of nursing care can influence nurses’ behavior in providing spiritual nursing care to patients.
Around the world, spiritual care in nursing is a critical part of providing holistic care, but within the nursing profession, there is a lack of certainty over the meaning of spirituality and delivery of spiritual care, including nurses thinking process that consider spirituality as religion.1,2 In providing holistic nursing care, a nurse must consider various aspects both physical, social, emotional, cultural and spiritual aspects in order to meet client needs.3
Spirituality is the presence of a relationship with a Higher Power, a response to a deep and mysterious human yearning for self-transcendence and surrender, a yearning to find our place and the search for the existential.4,5 Spiritual care is a practice and procedure must be performed by nurses on patients to meet the spiritual needs of patients.6 According to Meehan7 spiritual care is an activity in nursing to help patients deal through the attitudes and actions of nursing practice based on the values of spiritual nursing that recognize human dignity, kindness, compassion, calmness and gentleness. Chan8 and McSherry and Jamieson4 said that spiritual care is an integral and fundamental aspect of care where nurses show concern for patients. Spiritual care focuses on respecting patients with friendly and sympathetic interactions, listening attentively and giving strength to patients in dealing with their illnesses.9 Spiritual care does not promote religion, or it is not a practice to convince patients of their religion but rather gives patients the opportunity to express their values and needs, and empower them in relation to their illness.10,11
There has been considerable debate internationally across disciplines about the precise meaning of spirituality and the need for/possibility of reaching a definition.12 Internationally the WHO13 identifies 8 domains of spirituality which are reflected in definitions adopted in healthcare practice in the USA,14 in the UK15 and in Europe by the EAPC. The EAPC offers the following definition which guided this investigation: “Spirituality is the dynamic dimension of human life that relates to the way persons (individual and community) experience, express and/or seek meaning, purpose and transcendence, and the way they connect to the moment, to self, to others, to nature, to the significant and/or the sacred.”16 Spiritual care is at the heart of everyday nursing/midwifery practice.17 It is a core value running through nursing/midwifery practice.
The first aspect that must be considered by nurses in meeting the client's spiritual needs is the increase in nurses’ knowledge related to spiritual care to the client and its benefits, because one's positive and negative attitude toward an object is largely determined by the level of knowledge. To realize professional behavior in professional nurses is to have a strong scientific foundation, good psychomotor abilities and professionalism (giving empathy to clients) in providing nursing care to clients.18
According to Notoatmodjo,19 knowledge is a very important domain for the formation of actions and has several levels of knowledge including know, understand and application. Similarly, Eder et al.20 explain that attitude is a reaction or response of a person to a stimulus or object. Attitudes consist of 4 levels, namely being able to receive (receiving), able to respond (responding), and appreciate (valuing) and be responsible (responsible). Human behavior is very complex and has a broad scope. The formation of a new behavior, especially in adults starts from the cognitive domain, in the sense that the subject first understands the stimulus in the form of material or external objects, giving rise to new knowledge and attitudes on the subject.21
Previously, spiritual care was not considered as a dimension of nursing therapeutic, but with the emergence of holistic nursing, spiritual care has become an aspect that must be considered and the study of the spiritual needs of patients is developed which is considered as legitimate activities in the nursing domain.22 Nurses are people who are always present when someone is sick, during birth, and in death. In these life events spiritual needs often stand out, in this case the nurse's role is to provide spiritual care.23
Toney-Butler and Thayer24 conclude that nurses play a role in the nursing process by conducting assessments, formulating nursing diagnoses, preparing plans and implementing nursing and evaluating the spiritual needs of patients. Nurses also play a role in the communication process with patients, other health teams and clinical/educational organizations, and maintaining ethical issues in nursing.25
Based on the description above, the researcher was encouraged to conduct a study entitled the present study.
MethodThe method used in this study uses descriptive analytic design with cross-sectional approach. The population in this study is the number of nurses in the inpatient room with a total of 115 respondents. The research samples obtained were 85 nurses with stratified random sampling technique with inclusion criteria, namely nurses in the inpatient room at Citra Sari Husada Hospital in Karawang and willing to become respondents. The instrument in this study was a questionnaire. This study aims to determine the relationship of nurses’ knowledge and attitudes with nurses’ behavior in providing spiritual nursing care in the inpatient room at Citra Sari Husada Hospital, Karawang.
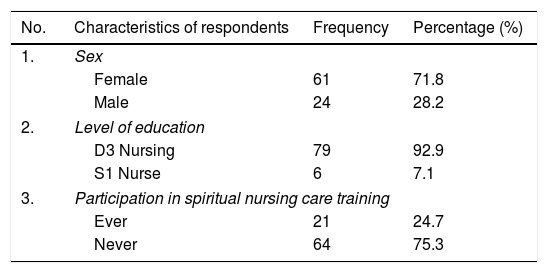
ResultsCharacteristics of respondents by sex, level of education, age, years of service and participation in trainingBased on Table 1, the results show that of the 85 respondents most were female with a total of 61 people (71.8%). The last education of the respondents was D3 Nursing as many as 79 people (92.9%). In this study, most of the respondents had never attended spiritual nursing care training, as many as 64 people (75.3%).
Frequency distribution of characteristics of respondents at Citra Sari Husada Hospital, Karawang.
| No. | Characteristics of respondents | Frequency | Percentage (%) |
|---|---|---|---|
| 1. | Sex | ||
| Female | 61 | 71.8 | |
| Male | 24 | 28.2 | |
| 2. | Level of education | ||
| D3 Nursing | 79 | 92.9 | |
| S1 Nurse | 6 | 7.1 | |
| 3. | Participation in spiritual nursing care training | ||
| Ever | 21 | 24.7 | |
| Never | 64 | 75.3 | |
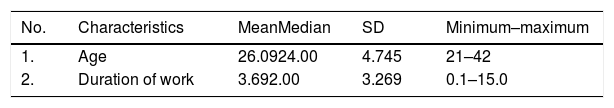
Based on Table 2, the average age of respondents is 26.09 years, the youngest is 21 years and the oldest age is 42 years. While the average duration of work of respondents is 3.69 years, the lowest tenure of 0.1 years and the longest 15 years.
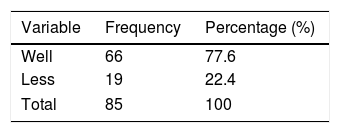
Univariate analysisKnowledge of respondents in providing spiritual nursing careBased on Table 3, respondents who have good knowledge in providing spiritual nursing care at the Citra Sari Husada Hospital in Karawang are 66 people (77.6%), and respondents who have less knowledge in providing spiritual nursing care at Citra Sari Husada Hospital in Karawang as many as 19 people (22.4%).
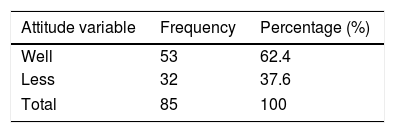
Respondents’ attitudes in providing spiritual nursing careBased on Table 4, there were 53 people who had good attitudes in providing spiritual nursing care (62.4%), and 32 employees (37.6%) lacked attitude in providing spiritual nursing care.
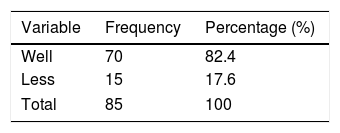
Behavior of respondents in providing spiritual nursing careBased on Table 5, 70 people (82.4%) had good behavior in providing spiritual nursing care at the Citra Sari Husada Hospital in Karawang, and respondents who had less suitable behavior in providing spiritual nursing care at Citra Sari Husada Karawang Hospital were 15 (17.6%).
Bivariate analysisThe results of the bivariate analysis in this study can be seen in Table 6.
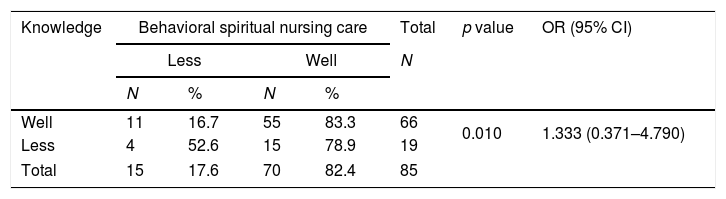
Analysis of relationship between knowledge and nurse behavior in providing spiritual nursing care at Citra Sari Husada Hospital, Karawang.
| Knowledge | Behavioral spiritual nursing care | Total | p value | OR (95% CI) | |||
|---|---|---|---|---|---|---|---|
| Less | Well | N | |||||
| N | % | N | % | ||||
| Well | 11 | 16.7 | 55 | 83.3 | 66 | 0.010 | 1.333 (0.371–4.790) |
| Less | 4 | 52.6 | 15 | 78.9 | 19 | ||
| Total | 15 | 17.6 | 70 | 82.4 | 85 | ||
Based on Table 6, respondents who have good knowledge and good behavior in providing spiritual nursing care at the Citra Sari Husada Hospital in Karawang are 55 (83.3%). About 15 respondents (78.9%) had less knowledge but had good behavior in providing spiritual nursing care. Respondents who had less knowledge and less behavior in providing spiritual nursing care were 4 people (52.6%). Respondents who have less knowledge but have good behavior as many as 11 people (16.7%).
Statistical test results obtained p value=0.010, it can be concluded that there is a relationship between knowledge and behavior of nurses in providing spiritual nursing care at Citra Sari Husada Hospital. From the analysis results obtained OR value=1.333 means nurses with less knowledge have a 1.33 times chance to perform better than nurses with good knowledge.
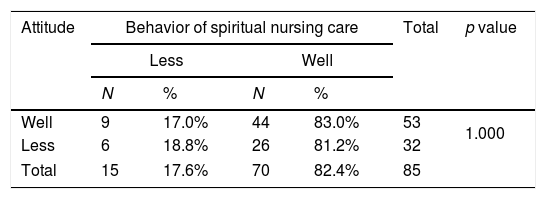
Relationship between attitude and nurse behavior in providing spiritual nursing careBased on Table 7, respondents who have good attitudes and good behavior in providing spiritual nursing care at Citra Sari Husada Hospital in Karawang are 44 people (83%). Respondents who had good attitude but lacked behavior in providing spiritual nursing care were 9 people (17%). There were 6 respondents (18.8%) lacking in attitudes and behavior in providing spiritual nursing care. Respondents who have less attitude, but good behavior are 26 people (81.2%). The statistical test results obtained p value=1.000 then it can be concluded there is no relationship between attitudes with the behavior of nurses in the provision of spiritual nursing care at Citra Sari Husada Hospital.
DiscussionBased on the results of the analysis in this study obtained from 85 respondents there were 66 respondents with knowledge of spiritual nursing care both performing spiritual nursing care, while as many as 19 respondents with less knowledge of spiritual nursing care did conduct spiritual nursing care efficiently. This shows that respondents with good knowledge of spiritual nursing care carry out spiritual nursing care behavior better than respondents who have poor spiritual nursing care knowledge. Knowledge is something that humans use to understand everything, which can be enhanced based on information obtained. Knowledge or cognitive skill is a very important domain in shaping one's actions. Knowledge is also influenced by formal education factors although it is not necessary to increase knowledge. Knowledge is a very important design in shaping one's actions.26
The length of service is also a factor. Nurses who are working for a long time will have more qualified skills. As a result, knowledge will also increase regarding the implementation of spiritual nursing care. Nurses who have good knowledge about spiritual care are expected to have good attitudes and perceptions about spiritual care so that spiritual care can be applied as a method of healing patients. The higher the nurse's knowledge about spiritual nursing care, the better the implementation of spiritual nursing care.27
Nurses’ knowledge influences spiritual nursing care supported by nurses who admit they cannot provide spiritual nursing care competently because during their education they did not receive guidance regarding the provision of spiritual nursing care to patients. Nurses are very instrumental in helping to meet the spiritual needs of patients by bringing religious leaders for the patients, providing opportunities to pray and interact with others.28 Nurses can also provide emotional support, teach prayer, motivate and give them time for worship, teach relaxation by Dhikr, and stand near the patient which is the nurse's way of providing the patient's spiritual support.29,30
Nurses who maintain their spirituality can find internal resources to care for patients by increasing comfort within themselves, also by being more sensitive to the spiritual needs of patients and bringing effective coping technique to face stress while providing nursing care.31
In order for nursing education to prepare nurses for holistic patient care, it is critical that educators become more aware of the religious and spiritual dimensions in patient care and be able to provide adequate knowledge and skills for nurses to offer spiritually based care in an ethical manner.32 Furthermore, spiritual care is an essential component in the nursing context, as nurses have to care for patients who may often turn to the spiritual dimension to cope and heal. These aspects are important issues to be considered in planning what should be taught as part of spiritual care.33
The attributes of spiritual care are healing presence, therapeutic use of self, intuitive sense, exploration of the spiritual perspective, patient-centeredness, meaning-centered therapeutic intervention and creation of a spiritually nurturing environment. Spiritual care is a subjective and dynamic concept, a unique aspect of care that integrates all the other aspects. It emerges in the context of nurses’ awareness of the transcendent dimension of life and reflects a patient's reality. The provision of spiritual care leads to positive consequences such as healing for patients and promotion of spiritual awareness for nurses.34
Research on health, well-being and spirituality has grown in the Western context, with studies showing that spirituality is an important part of a patient's life when confronted with illness. Empirical work has documented that shows that spirituality becomes particularly salient when patients must deal with HIV and AIDS, cancer and heart disease.35 Despite the growing body of literature abroad,36–38 research and literature on spirituality and spiritual care is sparse in South Africa. It has been argued that a failure to incorporate spirituality into nursing care by not addressing the spiritual needs of patients is unethical as spirituality is a part of being human.39 Miner-Williams contradicts holistic patient care. The lack of formal educational preparedness on spirituality and spiritual care appears to be the primary factor that has rendered nurses unprepared to deliver spiritual care.40 Thus the implications of this present study is essential for developing best practice in spiritual care education. So, this must be considered by nurse and midwifery educators for future incorporation in the nursing courses.
Conflict of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the 3rd International Conference on Healthcare and Allied Sciences (2019). Full-text and the content of it is under responsibility of authors of the article.