Nursing students are prone to needle stick injuries (NSIs) during their practice in the hospitals. This study aimed to identify the effective NSI prevention strategies for nursing students in the clinical settings.
MethodLiterature review was performed using the databases of ScienceDirect, ProQuest, MEDLINE, PsycINFO, Scopus, CINAHL, SpringerLink, JSTOR, and PubMed. The search terms of “nursing students”, “NSI incidents”, “prevention”, and “clinical settings” were entered, generating 103 articles published between 1991 and 2015.
ResultsOur study demonstrated the high rates of NSIs in low- and middle (India, 91.85%). and high-income countries (Taiwan, 56.00%). Most injuries especially occurred when students opening the ampules (53.15%) and performing intravenous cannulation (44.50%). Our review identified four main strategies to prevent NSIs; education, trainings, safe needle use, and effective communication. Our study suggested the development of education and trainings curriculum and self- report system and culture, the provision of financial, material and manpower resources to support the prevention of NSIs.
Conclusionsfour main strategies to prevent NSIs were education, trainings, safe needle use and effective communication.
Implications for practicecollaboration of hospitals and educational institutions is essential to develop effective NSI prevention programs.
Nursing students are at high risks of needle stick injuries (NSIs) during their practice in the clinical settings. They are exposed to sharp hazards while handling medical equipments, such as when they are administering medications or taking blood samples. Therefore, it is crucial for students to possess adequate competences regarding the procedures that require them to handle sharp devices.
To date, many studies had reported the high rates of needle stick injuries among nursing students. A study in Namibia demonstrated that 17% of total students had NSIs (Small, Pretorius, Walters, & Ackerman, 2011). Moreover, another study in China showed that among those who were injured were not vaccinated (Shiao, Mclaws, Huang, & Guo, 2002). Consequently, they are at higher risks of various bloodborne infections, such as human immunodeficiency virus (HIV), hepatitis B virus (HBV), and hepatitis C virus (HCV).
Despite the rate of injuries are relatively high, students had low awareness on the importance of reporting the injuries to head nurse and/or Clinical instructors. A study in India showed that 98.4% of students were injured during procedures with sharp devices. The study, furthermore, showed that only 18.4% of them reported the incidents (Mitra, Malik, Das, & Roy, 2010). Similarly, a study in Namibia showed that, of 55 percent of students who had NSIs, only 17 percent reported their incidents (Small et al., 2011). Underreported incidents occurred because students did not know how and where to report, were too busy, or were certain that the injuries had no negative consequences (Jan, Akhund, Akhtar, & Shaikh, 2014).
There are various strategies to prevent NSIs. Nevertheless, some countries, particularly low- and middle- income countries, face obstacles in achieving their mission in lowering NSIs. One of the most common obstacles includes financial constraints that frequently stand in the way of creating safer environment and preventing injuries for students, resulting in inadequate supply of resources (Hambridge, 2011).
MethodLiterature review was employed in this study, aiming to explore the effective needle stick injury prevention strategies for nursing students in the clinical settings.
We performed electronic searches in ScienceDirect, ProQuest, MEDLINE, PsycINFO, Scopus, CINAHL, SpringerLink, JSTOR, and PubMed to identify full- text review articles and studies published in 1991-2015, in Bahasa Indonesia or English that we consider represent the strategies of needle stick injury prevention. The search terms of “nursing students”, “NSI incidents”, “prevention”, and “clinical settings” were entered into the databases, generating a total of 303 articles. The articles discussed about the NCI prevention strategies across 29 countries.
This study comprised two main stages. At the first stage, 200 articles were deleted due to duplication and irrelevancy with the research topic. At the later stage, 103 selected articles were analyzed, in which 5 articles of them were specifically reviewed and analyzed. The study was performed in over 9 months, from October 2014 to July 2015.
ResultsOur review discussed about the incidence of needle stick injury among nursing students, factors associated with needle stick injury, consequences of needle stick injury, and needle stick injury prevention strategies.
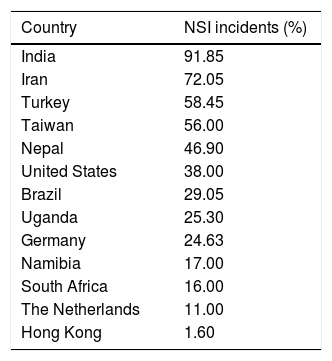
Needle stick injury among nursing studentsSome articles presented the incidents of needle stick injury among nursing students in 13 countries. The incidents were dominantly high in low and middle income countries. The incidents were highest in India, accounting for over nine tenth of the total respondents (91.85%). Surprisingly, the incidents in The high income countries, such as Taiwan and Unites States were also relatively high, accounting for over half (56.00%) and over one third (38.00%) respectively. The incidents were lowest in Hong Kong with the proportion of less than 2 percent (1.60%) (Table 1).
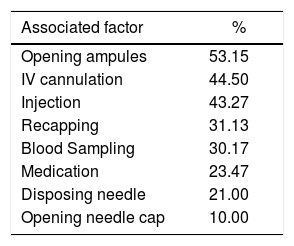
Factors associated with needle stick injurySome articles identified factors associated with needle stick injury. The results revealed that over half of the injury occurred when students opened the ampules (53.15%). Nearly half of the respondents were injured due to intravenous cannulation (44.50%) and injection (43.27%). The injury proportion was lowest when students opened the needle cap (10.00%) (Table 2).
Consequences of needle stick injurySome reviews highlighted the effects of needle stick injuries among students. Most of the articles stated that those who were injured were at higher risks of bloodborne diseases, such as HIV, HBV, and HCV. A study in Germany demonstrated the incidents had led to positive results of HCV (5.3%) and HIV (2.00%) infections (Hoffmann, Buchholz, & Schnitzler, 2013).
Needle stick injury prevention strategiesThe hierarchy of infection controlSome articles presented the hierarchy of infection control developed by the American Nurses Association (2002). The hierarchy underlined five preventive measures of bloodborne infections.
These measures were classified from the least to the most effective one. The first measure and the least effective one was the use of Personal Protective Equipment (PPE). The equipments might include barriers and filters, such as eye goggles, gloves, masks and gowns. The second measure was adherence to the standards of safe working practices. Nurses need to implement nursing procedures correctly as guided by the standards in the working unit. These practices might include proper practices of preventing needle recapping, placing sharp containers at eye's level and at arm's reach, and emptying sharps containers before they are full.
The third measure was administrative controls, such as policy and standards. When the regulation is in place, nurses will be able to differ which procedures that can prevent them from harms and injury. These controls might include the development of committee for needle stick injury prevention, hazard exposure control plans, and trainings regarding the prevention of needle stick injury.
The fourth measure was engineering controls. Activities within this measure included safe needle removal after use. Last measure and the most effective one was the elimination of hazards. All sharp hazards that have potential to harm nurses must be eliminated and removed properly. Besides, nurses need to limit unnecessary invasive procedures if possible.
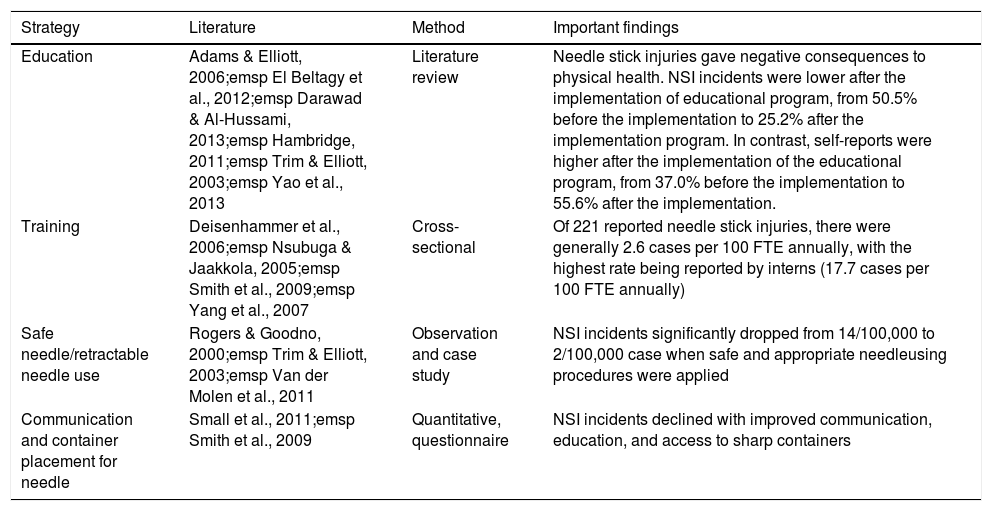
EducationFifteen articles emphasized the importance of education, safe needle handling, trainings and effective communication as strategies to prevent needle stick injury (Table 3).
Effective strategies for needle stick injury prevention.
| Strategy | Literature | Method | Important findings |
|---|---|---|---|
| Education | Adams & Elliott, 2006;emsp El Beltagy et al., 2012;emsp Darawad & Al-Hussami, 2013;emsp Hambridge, 2011;emsp Trim & Elliott, 2003;emsp Yao et al., 2013 | Literature review | Needle stick injuries gave negative consequences to physical health. NSI incidents were lower after the implementation of educational program, from 50.5% before the implementation to 25.2% after the implementation program. In contrast, self-reports were higher after the implementation of the educational program, from 37.0% before the implementation to 55.6% after the implementation. |
| Training | Deisenhammer et al., 2006;emsp Nsubuga & Jaakkola, 2005;emsp Smith et al., 2009;emsp Yang et al., 2007 | Cross-sectional | Of 221 reported needle stick injuries, there were generally 2.6 cases per 100 FTE annually, with the highest rate being reported by interns (17.7 cases per 100 FTE annually) |
| Safe needle/retractable needle use | Rogers & Goodno, 2000;emsp Trim & Elliott, 2003;emsp Van der Molen et al., 2011 | Observation and case study | NSI incidents significantly dropped from 14/100,000 to 2/100,000 case when safe and appropriate needleusing procedures were applied |
| Communication and container placement for needle | Small et al., 2011;emsp Smith et al., 2009 | Quantitative, questionnaire | NSI incidents declined with improved communication, education, and access to sharp containers |
FTE, full-time equivalent.
Nearly three quarter of the articles (11; 73.33%) mentioned the role of education as a strategy to prevent needle stick injury among students in the clinical settings. It was evident that educational programs could significantly reduce NSI incidents and increase students’ participation in self- reporting program (Yao, Wu, Yang, Zhang, Huang, Quian, & Yao, 2013). Likewise, a similar study in China indicated self-reports on NSI incidents were significantly higher after the implementation of educational program (Yang, Liou, Chen, Yang, Wang, Chen, & Wu, 2007). Apparently, education could raise students’ awareness regarding the risks of NSIs.
Saudi Arabia has long recognized the importance of education to prevent and reduce the risks of infections. Accordingly, the topic was among the top priorities in their nursing curriculum (El Beltagy, El-saed, Sallah, & Balkhy, 2012). Similarly, Jordan implemented educational program, causing the increase of students’ knowledge and the decrease of infection rates by 49.68% (Darawad & Al-Hussami, 2013).
TrainingsOver one- quarter of total articles (26.67%) indicated trainings as one of the effective strategies to prevent NSIs, along with education. Both trainings and education are interrelated, aiming to improve the knowledge of the students concerning NSIs. A study in German showed that trainings had lowered NSI during most risky procedures, like blood sampling (Deisenhammer, Radon, Nowak, & Reichert, 2006). Another study in Sub-Saharan Africa revealed that NSI incidents were nearly six times higher among staffs who had no training than those who had trainings (OR 5.72; 95%CI, 3.41-9.62) (Nsubuga & Jaakkola, 2005).
Some articles mentioned that universal and standards precautions were among the most important topics for trainings. The appropriate precautions procedures would help students to reduce NSIs (Borges, Ribeiro, & Oliveira, 2014). A study conducted in low- and middle income countries highlighted the low number of nurses participated in trainings of universal precautions, with the proportion of less than one fifth of the total respondents (16%) (Nsubuga & Jaakkola, 2005). The study suggested resources allocation for trainings to improve the knowledge, abilities, and practice of nurses in universal precautions (Tarigan, Kriebel, Quin, & Cifuentes, 2014).
Safe needle useAround 27% of the literature showed that the use of safe needles can reduce NSIs in nursing students. The articles presented the use of technology resulted in the development of protective needle shields to reduce NSIs. The reviews suggested the use of protective needle shield in high risk units along with the provision of trainings for healthcare workers and nursing students (Trim & Elliott, 2003).
Protective needle shields could prevent students from NSI incidents. A study conducted in 2000 showed that NSI incidents dropped from 27 cases to 3 cases (Salelkar, Motghare, Kulkarni, & Vaz, 2010). In the Netherlands, the use of protective needle shields was proven effective in lowering NSI incidents by 60 percent per year (Van der Molen, Zwinderman, Sluiter, & Frings-Dresen, 2011, 2011). Likewise, the use of protective needle shields had reduced the NSI incidents in the US by 76 percent (Salelkar et al., 2010).
Nevertheless, due to budget constraints, the availability of protective needle shields was limited in low resource countries. Accordingly, there was a need to improve supply of financial resources and to develop alternative protective needle shields that are affordable for low resource countries.
CommunicationOur reviews presented the vital role of communication in reducing NSI incidents. Little to no communication among healthcare workers regarding NSI incidents could lead to repetitive injuries. A study in Namibia showed that nearly one quarter (22.45%) of NSI among nursing students were underreported (Small et al., 2011). Furthermore, over half of total nursing students (55%) who experienced NSIs were not supervised by clinical instructors nor senior nurses (Small et al., 2011).
Effective communication among nursing students and clinical instructors and or senior nurses would help students feeling safe and confident. In Japan, effective communication had significantly prevented nurses from conflicts (OR 1.7; 95%CI, 0.98-3.00) (Smith, Mihashi, Adachi, Shouyama, Mouri, Ishibashi, & Ishitake, 2009).
DiscussionOur review uncovered the high incidents of NSIs among nursing students particularly in low and middle income countries despite the rates were also relatively high in some high- income countries. These findings reflected the need of actions to prevent the occurrence of NSIs since it might lead to various bloodborne diseases.
Our study demonstrated the high rates of NSIs occurred when students opening the ampules and performing IV cannulation. Therefore, we believed clinical instructors had substantial role in preventing injuries during procedures by providing adequate supervision to their students.
Our review identified four main strategies to prevent NSIs. They are education, trainings, safe needle use and effective communication. Both education and trainings could raise students’ awareness and knowledge regarding safe procedures, NSI prevention and management. Safe needle use, along with the use of technology for sharp devices would help students, too, to prevent NSI incidents. Last, effective communication along with adequate supervision from clinical instructors would prevent underreported incidents as well as help students to feel safer and confident to perform procedures, which later can also prevent them from injuries.
We believed many more preventive measures had been studied. However, articles in our review found these four strategies that had significantly be used. Our study suggested both educational institutions and hospitals could hand-in-hand in taking actions to develop programs to prevent NSI incidents among nursing students, including by developing educational and training programs and activities, establishing self- report system and culture for students, generating role model clinical instructors, developing regulations that promote zero NSIs, performing budget analysis and estimating rational budget allocation for NSI prevention programs, providing necessary facilities to support safe procedures.
We found budget constraints and insufficient resources prevented low and middle income countries from taking actions. Therefore, more efforts need to be taken in order to provide better supply and mobilize resources.
Results of our study could be the reference for future studies with respect NSI prevention and control.
ConclusionsThe rate of NSIs among nursing students was relatively high, especially when opening ampoules and performing IV cannulation. Strategies to prevent NSIs are, therefore, of importance. We identified the following as main strategies to prevent NSIs: education, trainings, safe needle use and effective communication. Our review suggested the collaboration of hospitals and educational institutions in developing programs to prevent NSI incidents among nurses.