To assess the effectiveness of pacifier and swaddling on premature infant's pain score, hearthrate, and oxygen saturation during an invasive procedure.
MethodThis randomized control trial involv 30 premature infants who were randomly assigned into control (n=15) and intervention (n=15) groups using parallel design. Infants in the intervention group received pacifier and swaddling when they were undergoing invasive procedures. The outcome indicators of the two-day intervention were pain score, hearth rate, and oxygen saturation. The Premature Infant Pain Profile (PIPP) was used in this study to measure infants’ pain.
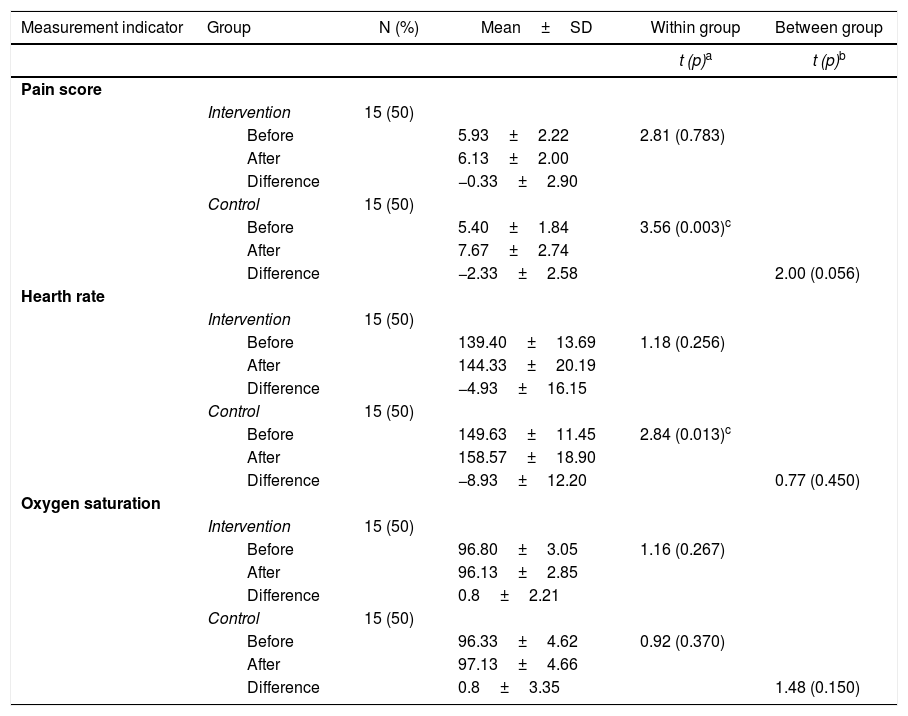
ResultsThe paired t-test results showed that the pain score and heart rate were significantly increased following the procedure in the control group (p=0.003; p=0.013 < 0.05); meanwhile, there was no significant increase in the intervention group (p=0.256; p=0.783 > 0.005). There was no significant different in oxygen saturation in the control group (p=0.270) and in the intervention (p=0.370) group before and after the procedure.
ConclusionsProviding pacifier and swaddling can impede the increase of premature infants’ pain score and hearth rate during an invasive procedures, therefore it can be implemented as an alternative to pain management in premature infants.
Premature infants receive invasive procedures for 93 times during hospitalization1,2. These invasive procedures can cause stress to the infants and lead to frequent stress response3,4. The Synactive Theory of Development proposed by Als in 1982 was relevant to this phenomenon. The theory consists of five subsystems: autonomic stability (physiological parameters), motor control (body movement); state control (sleep cycle), interaction and social responsiveness, and self-regulation5. During the invasive procedure, there will be over stimulation that influences all subsystems in infants. Those influences include instability in heart rate, oxygen saturation, and respiration rate. The changes in the motor subsystem are manifestated by hand and leg agitation activities; while the changes in state subsystem can be manifested by infant sleep disturbances6–8. Those changes can influence the process of brain nerve myelinization that can cause development disturbances in the short and long term periods9.
The non pharmacologic pain management has been developed years ago. Previous studies had been analyzed the effectiveness of swaddling in pain controlling10, physiological function11, safety12, and sleep13. Meanwhile, the use of pacifier had been proved to prevent heart variability14, and as a means of pain control15,16. A numbers of previous studies have used combination between pacifier and sucrose17–21, and facilitated tucking6,8 in dealing with premature infants’ pain who undergoing several invasive procedures such as heel-stick procedure, intramuscular injection of Hepatitis Vaccine, or intra venous insertion. However, there are limited studies in using combination between pacifier and swaddling in different pain procedures in preterm infants.
MethodThis study was a prospective randomized controlled trial with parallel design approach. Each sample received one type of invasive procedure such as hill-prick or venous access which was randomly allocated to the infants receiving pacifier and swaddling (Group A) or routine care (Group B). The blinding process was carried out by two experts to evaluate pain scores22.
The study sample was selected based on the convenience sampling from the special care unit and Neonatal Intensive Care Unit at Dr. Cipto Mangunkusumo Hospital, Jakarta. There were 30 preterm infants who met the criterias: (1) gestational age 26-36 weeks; (2) 2-30 days of post birth age, and (3) birth weight < 2500 g. The exclusion criteriaswere: (1) infants on sedative treatment, muscle relaxant, antiepileptic or analgesic drugs; (2) have congenital anomalies; (3) have neurological problems and history of neonatal seizure, and (4) experience severe physiological alteration.
Pain scores and physiological functions were measured 15 minutes before invasive procedure (baseline/T1). The intervention (pacifier and swaddling) was applied three minutes before the invasive procedure started (T2). The next measurements were carried out at the beginning of invasive procedure (T3), three minutes (T4) and 15 minutes after the procedure ending (T5). These measurements conducted in two days consequently in both groups.
Infants’ pain was measured using the Premature Infant Pain Profile (PIPP) which was developed by Steven, Jhonston, Pethrysen, and Taddion23. The PIPP is reported to have a moderate internal consistency (0.59-0.76 item total correlation), high interrater reliability (0.95-0.97) and intrarater reliability (0.89-0.91)7,24.
The Ethical clearance was obtained from the Ethical Research Committee, Faculty of Nursing Universitas Indonesia (0244/UN2.F12.D/HKP.02.04/2015) and the Ethical Research Committee, Faculty of Medicine Universitas Indonesia (0244/UN2.F12.D/HKP.02.04/2015). Written informed consent was obtained from mothers.
Pain score and physiological responses were measured five times (T1, T2, T3, T4, and T5). Data were rated by two experts. A Bland Altmant test was carried out to test the interrater reliability of two experts and the result were 0.632 and 1.99 in the range of –5 to +5. It means that there was a similar perception between experts.
Chi-square test was used to test the homogeneity of data in both control and intervention groups. The hypothesis was tested using dependent and independent t-test with the level of significance was 0.05.
ResultsThe result of the homogeneity test showed that there were no significant differences in infants’ characteristics between control and intervention groups. The characteristics were gestational age, chronological age, the length of stay, birth weight, body weight, length of the invasive procedure, gender, type of invasive procedure, and Apgar score.
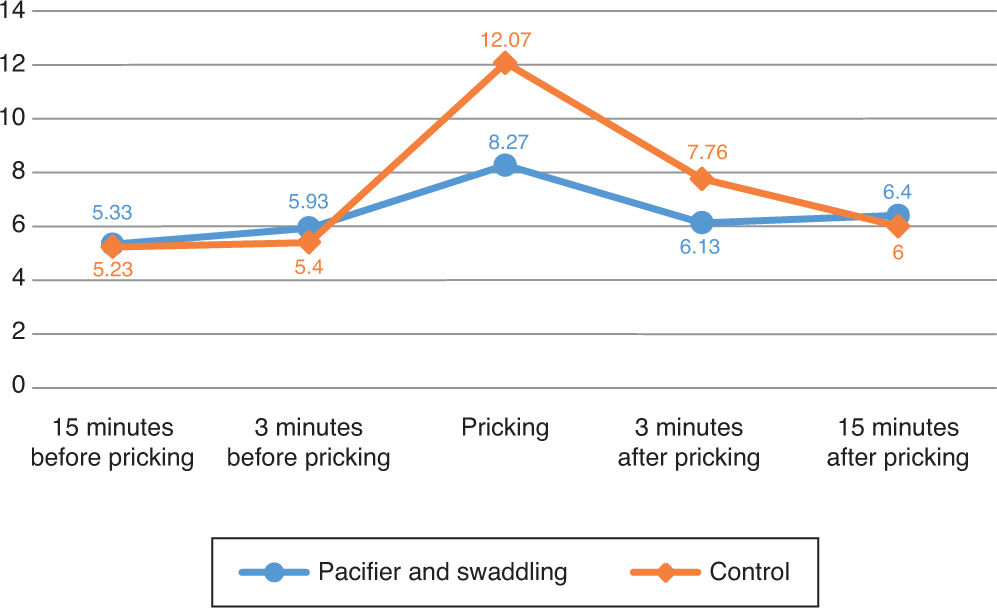
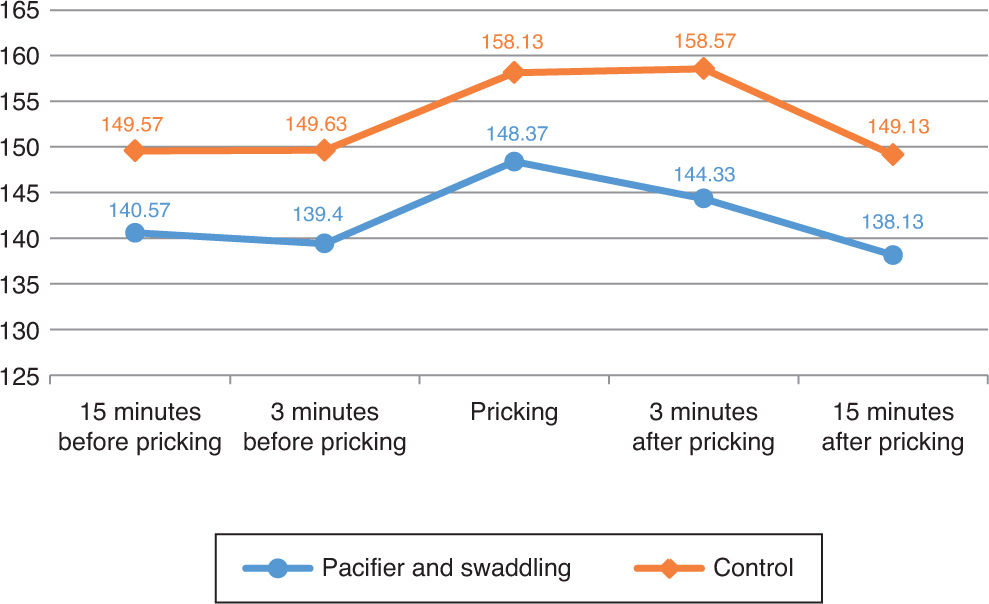
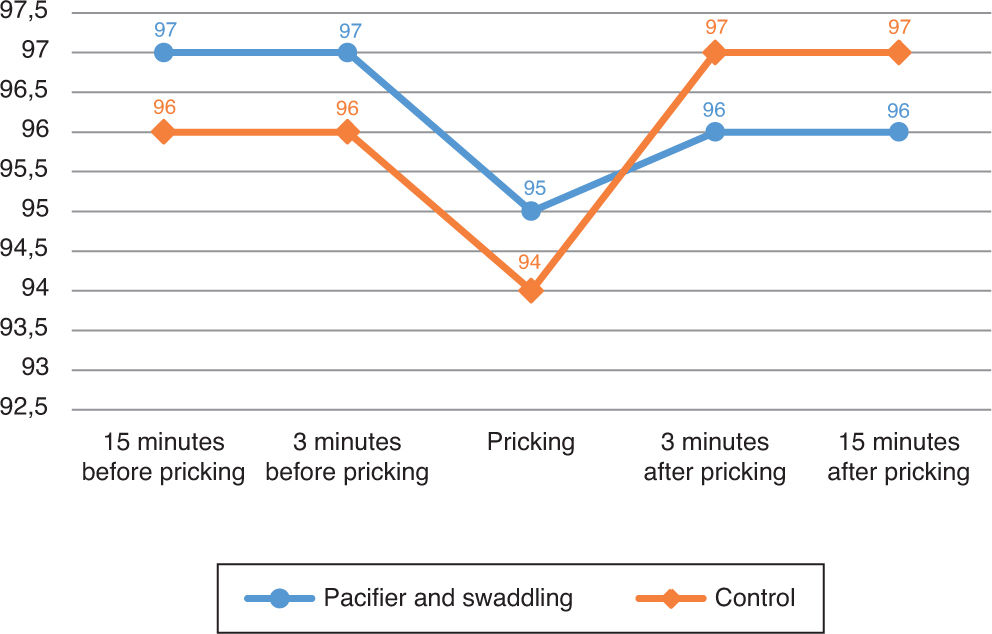
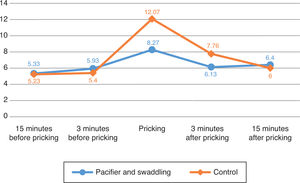
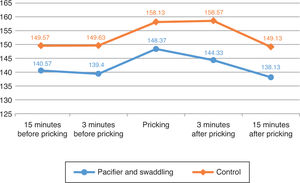
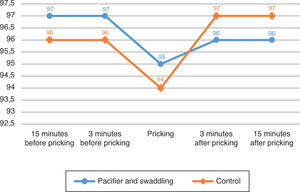
The output of this study was the comparison of pain score, saturation, heart rate differences before and after invasive procedures between intervention and control groups (Table 1). There were no significant differences in all variables. However, there were significant differences in several spots of measurements between two groups (Figure 1).
Comparison of treatment effects on pain score, hearth rate and oxygen saturation (n=30).
| Measurement indicator | Group | N (%) | Mean±SD | Within group | Between group |
|---|---|---|---|---|---|
| t (p)a | t (p)b | ||||
| Pain score | |||||
| Intervention | 15 (50) | ||||
| Before | 5.93±2.22 | 2.81 (0.783) | |||
| After | 6.13±2.00 | ||||
| Difference | −0.33±2.90 | ||||
| Control | 15 (50) | ||||
| Before | 5.40±1.84 | 3.56 (0.003)c | |||
| After | 7.67±2.74 | ||||
| Difference | −2.33±2.58 | 2.00 (0.056) | |||
| Hearth rate | |||||
| Intervention | 15 (50) | ||||
| Before | 139.40±13.69 | 1.18 (0.256) | |||
| After | 144.33±20.19 | ||||
| Difference | −4.93±16.15 | ||||
| Control | 15 (50) | ||||
| Before | 149.63±11.45 | 2.84 (0.013)c | |||
| After | 158.57±18.90 | ||||
| Difference | −8.93±12.20 | 0.77 (0.450) | |||
| Oxygen saturation | |||||
| Intervention | 15 (50) | ||||
| Before | 96.80±3.05 | 1.16 (0.267) | |||
| After | 96.13±2.85 | ||||
| Difference | 0.8±2.21 | ||||
| Control | 15 (50) | ||||
| Before | 96.33±4.62 | 0.92 (0.370) | |||
| After | 97.13±4.66 | ||||
| Difference | 0.8±3.35 | 1.48 (0.150) | |||
Difference: the result from mean after invasive procedure minus mean before invasive procedure. Between groups: the comparison of mean differences between intervention and control groups.
The peak score of pain was during the invasive procedure. The score increased 6.67 point in the control group compared to 2.34 point in the intervention group. The increase of pain score was significant in the control group (p=0.003) (Figure 2).
The heart rate increased in both groups during the procedure, and it decreased significantly in the intervention group after the procedure (p=0.013).
The oxygen saturation was decreased in both groups and relieved three minutes after the procedure. There was no significant difference in oxygen saturations before, during, and after procedures between two groups.
DiscussionThe low score of pain and stability of physiological function are the main objectives of non-pharmacologic pain management. The main objectives of this study were to measure the differences in pain score, saturation, and heart rate before, during, and after procedures between infants who received pacifier and swaddling, and the control group who received routine care. Based on those indicators, there were no significant effect of pacifier and swaddling in reducing pain score, stabilizing heart rate, and oxygen saturation. This result was relevant with previous studies that providing pacifier were not significantly reducing the pain score in preterm infants25 and preventing alteration in heart rate14. Other studies also found that using pacifier and swaddling was not effective in preventing oxygen saturation variability26. Longer stimulation is needed to give effect on the oxygen saturation changes26.
On the other hand, several studies had different finding with this study. The previous study identified that pacifier with sucrose can decrease infant's pain17. A meta-analysis of 10 articles identified that providing pacifier can decrease pain responses16 and decrease pain score in term and preterm infants8,20. Review articles also found that pacifier can decrease infants’ pain score27,28.
This study was different with previous studies in term of infant gestational age. In the previous studies, gestational age of the infants involved was more than 37 weeks17,20; meanwhile, in this study the gestational age of the infant was less than 37 weeks. Preterm infants are more sensitive to stimuli which characterized by physiological changes, ineffective regulation, and negative cues30–32.Prematurity can lead the increase of hearth rate, respiration rate, and oxygen saturation compared to term infants. Besides that, our study did not measure baseline data of infant state which was done in the previous study that may influence the difference of physiological function indicators.
The pain observation in this study was two days, meanwhile the observation in the previous studies was carried out in three and five days8,20. Furthermore, the previous studies measure the mean score of the whole observation period17,20, while this study using different score between before and after the procedure. This study is also different with other previous study in regard to the intervention used. This study used a combination between pacifier and swaddling, yet other studies used a combination of pacifier-facilitated tucking8, also pacifier and sucrose17,20.
However, our study found that pacifier and swaddling impeding the increase of pain score during acute period (during procedure-three minutes after the procedure). The frequency of heart rate also decreased faster in the pacifier and swaddling group compared to infants in the routine care group. The decrease of heart rate was faster significantly in the pacifier and swaddling group (p=0.013) (Figure 3).
Physiologically, heart rate, respiration rate, blood pressure, intracranial pressure of infants who receive pain procedure will increase. This response due to the release of adrenal stress hormones associated with pain7. The pain was impeded by the antinociceptive effect of application pacifier and swaddling that can reduce pain sensation17.
Based on Gate Control Theory, applying pacifier and swaddling can impede the transfer of pain impulse along the spinothalamic tract that can reduce the pain sensation28,33. The combination of pacifier and swaddling can increase the stimuli that sift transferring pain stimuli which can generate stronger analgesic effect29,34. Pacifier and swaddling are simple tools that are easy to find in the developing country.
Conflicts of interestThe authors declare that they have no conflicts interest.