A nurse, caregiver, and elderly partnership are essential in aged care institutions to maintain a functional status and quality of life for the elderly. However, there are insufficient aged care institutions that can provide thorough care service due to the limitations of the aged care service system teams. This study aimed to determine the effectiveness of the nurse, caregiver, and elderly partnership model (MiRaDaSia) on the functional status and quality of life of the elderly living in public aged care institutions in Jakarta, Indonesia.
MethodThis quasi-experimental design included 102 participants in an intervention group and 102 participants in a control group. Samples were taken with multistage random sampling, the World Health Organization Quality of Life-BREF, and Barthel Index were used to measure elderly patient quality of life and functional status, and McNemar's test and repeated measurements were used to analyze the results.
ResultsThe results showed improving functional status and quality of life after 12 weeks of the intervention.
ConclusionsWe can conclude that the MiRaDaSia model is significantly effective in improving the functional status and quality of life of the institutionalized elderly. The use of this model allowed the aged care service system members to take part based on their roles and competencies optimally. Finally, this model can be used as a model of care in other aged care institutions in Indonesia and as a training reference for future nurses to be assigned in that setting.
Increased life expectancies worldwide mean there is a global phenomenon of increasing numbers of the elderly. This phenomenon is also occurring in Indonesia, where there will be a sudden change of demographic profile to an aging population, with the total number of elderly to exceed 7% of the total population.1,2 This situation should be anticipated, and the challenge becomes developing various services to handle the needs of the growing elderly population, one of which is the need for institutionalization. Aged care institutions were designed to address this phenomenon. Aged care institutions are expected to maintain and improve the quality of life and psychological well-being of this elderly population by offering caring and helpful services such as physical, spiritual, social, and psychological coaching.3
The growing development of the 9% aged care institution led to changes for a better and more flexible approach and became a norm in Taiwan and China.4 However, aged care institutions face problems on increase the elderly population. In Latin America, aged care institutions became the last choice of individuals following unsatisfactory elderly services.5 Many facets of institutionalization, such as family abandonment, exclusion, and social isolation, contribute to negative perceptions. In Indonesia, common perceptions of aged care facilities, where limited space and financial support and the norms and rules the elderly residents were bound by led to a social image as a place for separating the elderly from family.6 Along with this perception, services in the aged care institutions were challenged when faced with the numerous problems of the elderly and the aging process, including irreversible chronic conditions that result in a decline of functional status if early diagnosis, treatment, and rehabilitation services are not performed well in the aged care institution. Given these various reasons, it is important to provide living environments that enhance individual functional ability by addressing the needs of the elderly.7
Data from studies conducted in Indonesia have shown a monotonous routine with activities of daily living (ADL) and a lack of attention to the elderly individual's needs. These adverse effects are partially caused by limited numbers of skilled care providers, lack of worker understanding of their roles, and the high demand for a health care workforce.8 Aged care institution services are delivered by nurses, physicians, social workers, and caregivers, which leads to both benefits and challenges. The limited number and lower quality of care providers creates a significant burden on care services and leads to unfortunate events such as elder abuse, a further decline of functional status, and a lower quality of life.9,10 This slowly decreasing quality of care is also caused by poor teamwork resulting from institutional, organizational structures as well as gaps in education and communication among the care providers.11,12 This entails clarification of the vague expectations for the performance of roles by care providers, freeing up more time to avoid the restriction on activities due to insufficient time to care for the elderly, and even incorporating skills training aimed at the daily care routines for maintaining and improving the functional status of the institutionalized elderly.13
A physical disability often manifests as the loss of the ability to live independently and complete basic ADLs without assistance, such as bathing, dressing, eating, and mobility.14 Declining functional capacity, which is worse among the elderly in institutions, contributes to limited physical activity for the elderly and may cause severe cardiometabolic health problems and worsened quality of life.15,16 Further declining functional capacity and hospitalization of the institutionalized elderly due to chronic illnesses both need to be prevented to avoid further effects leading to decreasing quality of life for the elderly that encompasses physical health, psychological status, social relationships, and environment; it also includes health problems of the care providers.17,18 Declining functioning of those in aged care institutions has caused caregivers working in those institutions to have higher rates of depression and increasing neglect of their health.19 This doubled effect needs to be addressed with a renewed integrated care system that includes nurses, social workers, and caregivers through health measures and strategies that empower the further involvement of the elderly themselves as the consumers of the aged care institution's services.20
There are few studies that measure the effects of partnership in elderly care, especially between nurses, caregivers, and the elderly themselves, including in Indonesia. To address this matter, the nurse, caregiver, and elderly partnership model (keMitraan peRawat, penDamping dan lanSia, MiRaDaSia in Bahasa) were developed by researchers to provide a solution for the problems of caregivers and nurses in aged care institutions. With this model, the shared decision-making of the elderly person's possible nursing interventions can be attained through a sympathetic practitioner providing holistic care and being authentically engaged with the elderly.21 This research was needed to provide broad information about how the performance of elderly care services can contribute to an improved quality of life for the institutionalized elderly in developed countries such as Indonesia. The present study of the current system of care providers was aimed at determining how to allow each and every member of the aged care system to optimally execute their own roles and synergize those roles for better institutionalized aged care services.
MethodsThis study used a quasi-experimental design with control groups and participants from several public aged care institutions in Jakarta, Indonesia. The target population consisted of individuals aged 60 years or older.1 The sample size was 102, and the inclusion criteria were people who were not diagnosed with mild to severe dementia as proved by their medical status on the institution's report, not hearing or visually challenged, and willing to participate in this study. Out of 204 elderly, 200 met the requirements and were included in the final sample. This research passed the ethics test for the Faculty of Nursing's Ethics Committee with number 0347/UN2.F12.D/HKP.02.04/2015. All the participants were given an explanation about the research program and signed the informed consent paperwork. There was no physical or mental harm to the participants.
Data collection included the sociodemographic variables of age, sex, educational attainment, occupation, length of stay at the aged care institution, and health problems. Furthermore, to assess functional status and quality of life, the Barthel Index of ADLs, Indonesian version was used, which has been validated in the setting of neuroscience studies and is considered easy to use, reliable, and sensitive to change. In addition, quality of life was measured with a modified questionnaire adapted from the World Health Organization (WHO) Quality of Life-BREF (WHOQOL-BREF) that had been translated into Bahasa by Mardiati in 2006,22 with a previous validity test of r=0.638–0.879 and reliability test of 0.9, which were also shown in other studies.23 The collected data were analyzed through simple frequencies or means and standard errors of each variable. McNemar's test was used on categorized and abnormally distributed functional status. After that, a repeated measurement test was calculated to identify the normal distribution and homogeneity of the quality of life in both groups, and Levene's test showed both groups were homogeneous.
The MiRaDaSia model is a service model carried out through partnerships between nurses, caregivers, and the elderly according to their roles. Implementation of this model for 12 weeks began with the training of nurses for 60hours, providing theories related to age-related changes and common health problems of the elderly in institutions, and it included a practicum. Caregivers were trained for 30hours in relation to the daily activities of the elderly and minimal assistance related to elderly nursing care. A pre-conference was held daily for nurses, caregivers, and elderly representatives to share tasks according to their respective roles and discuss the activities that would be carried out by individuals and elderly groups. The meetings were also attended by facilitators. The implementation of the study was also followed by the facilitator through daily supervision for the first month, and then supervision three times per week during the second month and once in the third month. The facilitators were nurses who had graduated with a professional degree and had been previously trained regarding the MiRaDaSia model. The researchers functioned as consultants and visited the aged care institutions three times a week to solve any problems found related to the elderly care conducted by the nurses and caregivers during the three months of intervention.
ResultsTable 1 shows the distribution of the 200 elderly participants, divided into 100 in the intervention group and 100 in the control group.
Distribution of elderly functional status, quality of life, and sociodemographic variables in a public aged care institution in Jakarta (n=200).
| Variable | Intervention (n=100) | Control (n=100) | ||
|---|---|---|---|---|
| n | % | n | % | |
| Sex | ||||
| Male | 46 | 43 | 42 | 37 |
| Female | 60 | 57 | 64 | 63 |
| Education | ||||
| Illiterate | 34 | 32 | 52 | 49 |
| Finished primary and secondary education | 72 | 68 | 54 | 51 |
| Occupation | ||||
| Formal | 14 | 13 | 13 | 12 |
| Informal | 92 | 87 | 93 | 88 |
| Health problems | ||||
| No | 5 | 5 | 3 | 3 |
| Yes | 101 | 95 | 103 | 97 |
| Variable | Intervention (n=100) | Control (n=100) | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Age | 71.46 | 8.42 | 69.59 | 8.82 |
| Length of stay (in months) | 41.21 | 33.99 | 45.15 | 38.43 |
| Functional status | 93.49 | 12.63 | 97.26 | 7.50 |
| Quality of life | 83.34 | 13.69 | 83.55 | 11.89 |
Table 1 shows that the majority of the respondents in the intervention group were women (57%) who had been schooled in primary or higher education (68%), were previously engaged in informal occupations (87%) and had health problems (95%). The sociodemographic results from the control group demonstrated a similar pattern, with the larger proportion of participants being women (63%) who were educated (51%) and had worked in informal sectors (93%). Thus, the groups generally had no differences in sociodemographic characteristics.
The study participant mean age was 71.46 years (±8.42) in the intervention group, which is higher than in the control group, with a mean age of 69.59 years (±8.82), even though it was statistically proven that there was no significant differences between the groups (p=0.116). Among the independent variables, functional status was the only variable with a significant difference between the intervention group (93.49±12.63) and the control group (97.26±7.50). This could be the result of the fact that the majority of the respondents in the control group were from the independent-care residential unit, so they had better initial functional capacity in comparison to those in the intervention group. However, participants in both groups had independent activity in their daily routines.
Table 2 displays the rise in elderly functional status between groups in the time span covered by the intervention. Cochran's Q test revealed a significant difference (Q=17.2; p=0.001) within the study group. Further elaboration might come from this type of care in the study group.
Differences in elderly functional status in both groups at the three-time measurements of baseline, 6 weeks, and 12 weeks.
| Functional status at baseline | Functional status at 6 weeks | Functional status at 12 weeks | Cochran's Q/p-value | ||
|---|---|---|---|---|---|
| Independent | Dependent | Independent | Dependent | ||
| Intervention | 17.2/0.001 | ||||
| Independent | 58 | 9 | 57 | 8 | |
| Dependent | 10 | 25 | 7 | 26 | |
| Control | |||||
| Independent | 71 | 12 | 71 | 6 | |
| Dependent | 5 | 11 | 5 | 9 | |
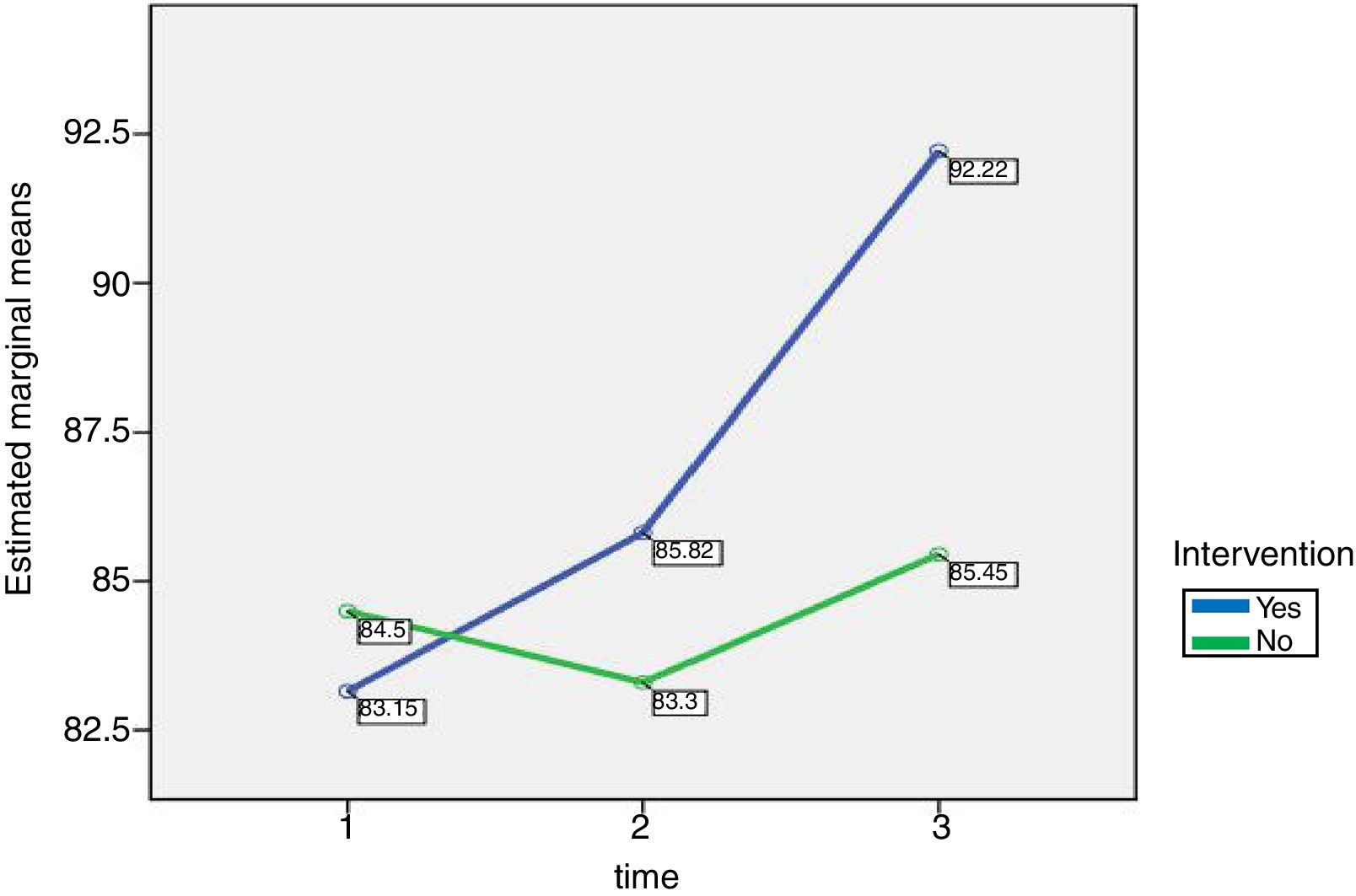
The blue line in Fig. 1 shows the increasing mean of quality of life measurements after 6 and 12-week programs in the intervention group (mean for baseline, 6 weeks, and 12 weeks were, respectively, 83.15, 85.82, and 92.22). In the control group, shown by the green line, there was an initial drop in the quality of life before a steady improvement (baseline, 84.50; 6 weeks, 83.30; and 12 weeks 85.45). This figure also reveals the sharp rise in the intervention group that suggests a strong impact from the program on improving quality of life among the institutionalized elderly.
DiscussionThe participants in this study were included in the mild aged category based on the mean of their ages. This finding confirmed that functional status altered with increasing age along with the overall aging process and health conditions.24,25 These conditions require a thorough nursing intervention, taking into account their sociodemographics, including institutionalization. The worsening conditions of the elderly and some additional factors, including specific changes related to sex, poor education, and past uneventful occupations, means the elderly are included in a vulnerable population and contributes to the declining quality of life for them.20
Improvements in the functional status and quality of life of institutionalized elderly after various patient-centered nursing interventions have been rigorously studied. However, this study emphasized how integrated nursing care involving nurses, caregivers, and the elderly will be one of the effective procedures for combating the nature of aging in the elderly. A significant improvement of functional status was found in the study group after Cochran's Q test (Q=17.2; p=0.01). This study's integrated nursing model had similar results as other studies with regard to functional ability.26 A previous study by Chao et al. mentioned the importance of integrating individual patient health management and community health management.27 However, this study only measured elderly satisfaction. This study can elaborate on previous findings that not only is patient satisfaction affected but these interventions can also promote further functional capacity increases for the elderly.
The results of this study demonstrate that the average mean of quality of life increased significantly in the intervention group after a 12-week implementation of the MiRaDaSia model. While there was no significant change in the control group, it was suggested that implementation of the MiRaDaSia model was effective for improving the elderly's overall quality of life. A possible reason for these results is that the majority of the control group sample was drawn from independent-care residential units that allow the performance of ADLs without assistance. Unlike the elderly residents who were still able to engage in daily routines by themselves, those from the dependent-care residential units in the intervention group received assistance in performing their daily routines, and thus, their improvement could be followed. Similar results were also mentioned in previous studies demonstrating that physical and social activities improved the quality of life.2,28,29 A centered and integrated health management model was also implemented in China, with improvements in health indicators.26 A study conducted by Riasmini indicated after 3 and 6-month evaluations that improved elderly quality of life can be achieved with a family, health care, and elderly partnership.22 These findings add more confirmation that in order to improve elderly quality of life, an integrated health care system should be provided.
In this study, improved functional status and quality of life can be explained by the increased interaction and attention from the institutional care provider. One of the topics covered during the implementation of the MiRaDaSia model showed how nurses and caregivers should communicate therapeutically with the elderly. This aspect confirmed a study that stated good communication with and among staff was an important element for supporting positive relationships with institutionalized elderly.30 Even though the association between these variables was not analyzed, the previous study explained how more attentive care from providers could help the elderly minimize functional limitations, which is a predictor of declining quality of life.27,31 However, cognitive impairment, declines incontinence, and hospitalizations should also be considered as they were statistically shown to be prognostic of functional limitations.15
The long-run use of the Barthel Index in aged care institutions in Indonesia should be evaluated, especially for the public aged care settings. Given that most of the residential elderly were homeless and poorly financed, their will to survive and resilience were high and thus affected their daily activities.32 These elderlies will continue to do their daily routines despite their functional limitations. With that in mind, these elderlies are also very grateful for the government aid of daily necessities, so the least they can do is independently take care of themselves regardless of their declining functioning.33 The MiRaDaSia model's focus on the partnership of nurses, caregivers, and the elderly in the institution allows for compassion for the elderly and support within the group of care providers. The positive results with this model should be considered to empower each and every care provider to take on their roles with complete competency.
Our result is a key contribution to linking elderly health indicators and nursing care performance in aged care institutions. However, because the data were collected from aged care institutions in Jakarta, a generalization of the results should be considered very carefully for future studies. As the first study that integrated a system of care, we suggest that continuous supervision and evaluation should be done to maintain the future sustainability and assurance of the trained care providers in the built integrated system of care and further prevent the high burden of care.34 Examining this possible high burden of care is another topic of interest for future studies. Given this explanation, we believe our study will be a useful and practical choice for elderly care and health policy makers for initiatives for the betterment of aged care services. In the end, this improvement of service should change negative perceptions of aged care services and make it one of the alternative solutions for the elderly living alone in the community.
The majority of the elderly participants in this study were women around 69–71 years old who had an educational level of elementary school or less, with an average length of stay in the institution of more than 6 months and who had more than one health problem. After 12 weeks of the MiRaDaSia model being implemented, there was a significant improvement of functional status and quality of life. This result was the first step for the aged care institutions to provide a better partnership of the care providers so that they can maintain or improve the functional status and delay the declining quality of life for the institutionalized elderly.
MiRaDaSia can be implemented as a practical model to enhance the services provided by professional staff for the institutionalized elderly in Indonesia, or even in other countries with similar sociodemographic characteristics, to strengthen our findings. Future studies should consider a longer implementation (6–9 months) of this model to maintain sustainability.
Conflict of interestsThe authors declare no conflict of interest.
This work is supported by Hibah PTUPT 2018 funded by The Ministry of Research, Technology, and Higher Education Republic of Indonesia No. 441/UN2.R3.1/HKP.05.00/2018.
Peer-review under responsibility of the scientific committee of the Second International Nursing Scholar Congress (INSC 2018) of Faculty of Nursing, Universitas Indonesia. Full-text and the content of it is under responsibility of authors of the article.