The aim of this study is to determine the effectiveness of sialang honey on wound bed preparation in diabetic foot ulcer.
MethodThe study design was quasy experiment with one group pre test post test design approach. The sampling technique used was consecutive sampling, where respondents were selected based on the criteria that had been planned. Instrument used in this study was wound bed score, where the measurement results will be analyzed using Wilcoxon test with 95% confidence level.
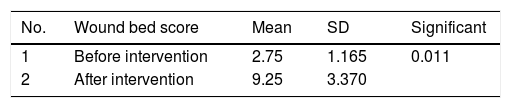
ResultResult of this study was average wound bed score before intervention was 2.75 and became 9.25 after the intervention on a scale of 0–16. Wilcoxon test in this study obtained p value 0.011 with the conclusion that sialang honey had a significant effect on wound bed preparation in diabetic foot ulcer.
ConclusionStatistically, honey can help the occurrence of wound bed preparation in diabetic foot ulcer.
Globally people with diabetes mellitus (DM) in 2014 it was estimated at 422 million.1 The pattern of increasing DM sufferers in Indonesia has a graph of the same increase that occurs on a global scale and in 2015 there were 10 million people with DM in Indonesia.2 An increase in the number of DM patients who were not handled properly would be followed by an increase in the number of DM complications from the DM. 15% of people with diabetes would experience diabetic foot ulcer and up to 70% will experience amputation.3
Treatment of diabetic foot ulcer was still a difficult problem. However, wound care for diabetic foot ulcer was considered as one of the ways that could be carried out to reduce the number of amputations and even the number of deaths. The right treatment method for diabetic foot ulcer will improve wound healing.4
One of the wound care methods that could be used to improve wound healing is to maintain moisture at the base of the wound and prevent bacterial colonization. The wound care method was often known as the moisture balance method. The moisture balance method used dressings to maintain moisture in that the environment for wound healing could be maintained optimally.5
Honey is a natural liquid produced by honey bees from the flowers of plants or other parts of plants or the excretion of insects that have a sweet taste.6 Honey is osmotic in that it contains almost 20% water. Honey properties like this can improve moisture balance in wounds and eventually can trigger autolytic debridement as one of the actions of wound bed preparation.7
The aim of the researchTo determine the effectiveness of sialang honey on wound bed preparation in clients with diabetic foot ulcer.
Design of researchThe design of research used was quasi-experimental approach one group pretest and post test design.
Population and sampleThe population in this study were all patients with diabetic foot ulcer in Padangsidimpuan City. The sampling technique used is consecutive sampling where all diabetic foot sufferers can become a research sample if they meet the existing criteria and their acquisition within the prescribed time limit.
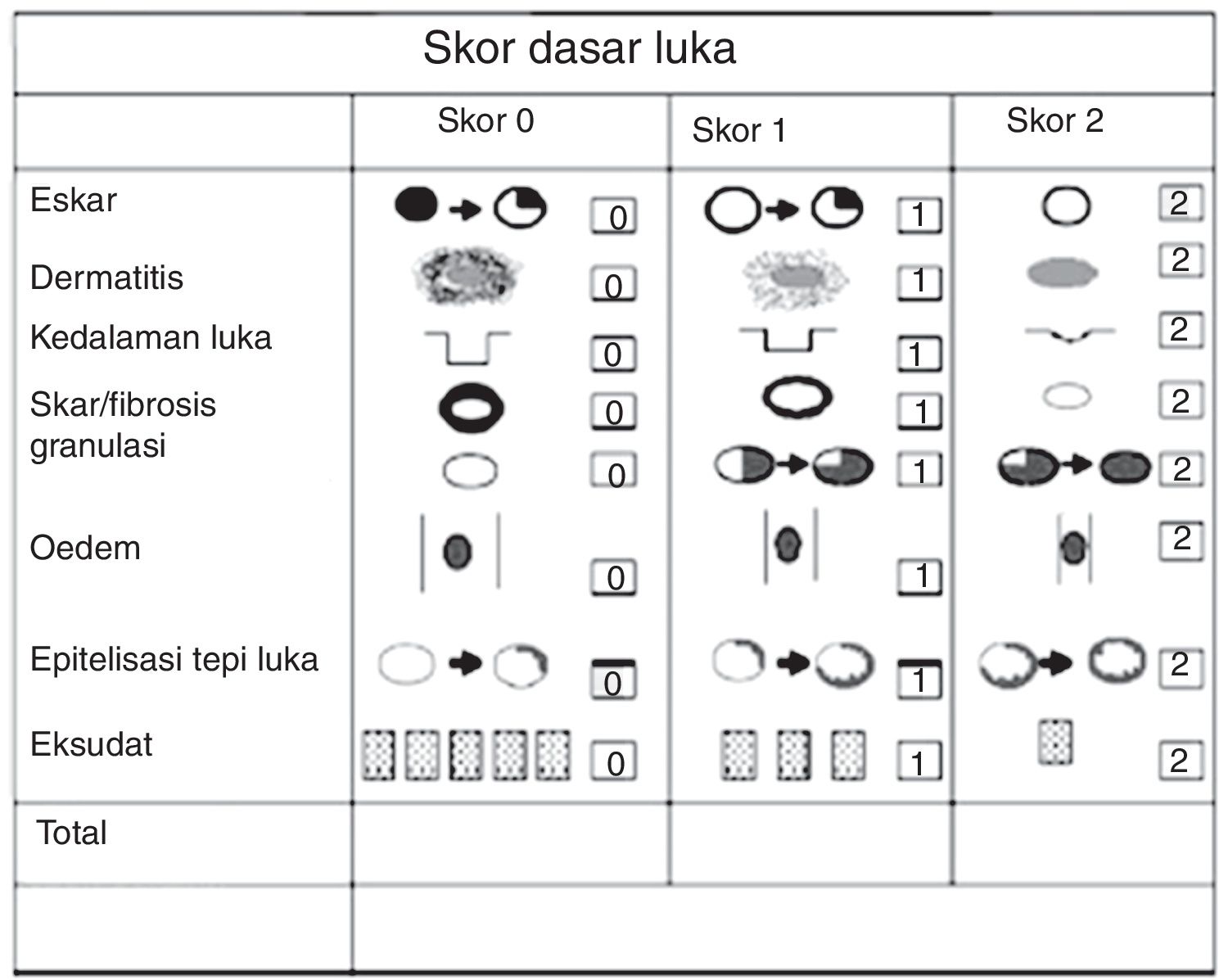
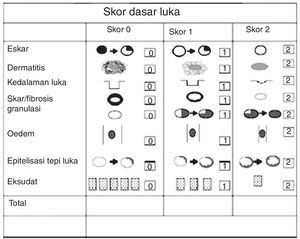
Measurement methodThis research used observation sheet wound bed score (Fig. 1).
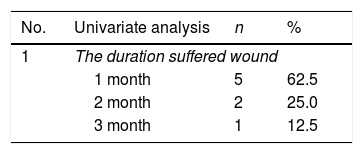
The resultUnivariate analysisThe analysis results were displayed in the form of frequency distribution tables and percentages (Tables 1 and 2).
Distribution of research subjects according to the duration of the injury and day of treatment.
| No. | Univariate analysis | n | % |
|---|---|---|---|
| 1 | The duration suffered wound | ||
| 1 month | 5 | 62.5 | |
| 2 month | 2 | 25.0 | |
| 3 month | 1 | 12.5 | |
| 2 | Day of treatment | n | % |
|---|---|---|---|
| The day 6 | 3 | 37.5 | |
| The day 8 | 1 | 12.5 | |
| The day 10 | 0 | 0.0 | |
| The day 12 | 2 | 25.0 | |
| The day 14 | 1 | 12.5 | |
| >The day-14 | 1 | 12.5 | |
| Total | 8 | 100.0 | |
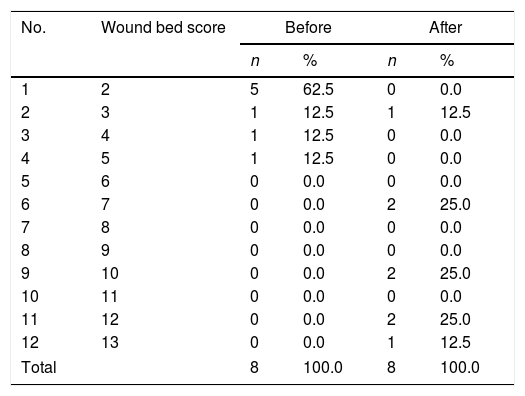
Distribution of research subjects based on wound bed scores before and after intervention.
| No. | Wound bed score | Before | After | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| 1 | 2 | 5 | 62.5 | 0 | 0.0 |
| 2 | 3 | 1 | 12.5 | 1 | 12.5 |
| 3 | 4 | 1 | 12.5 | 0 | 0.0 |
| 4 | 5 | 1 | 12.5 | 0 | 0.0 |
| 5 | 6 | 0 | 0.0 | 0 | 0.0 |
| 6 | 7 | 0 | 0.0 | 2 | 25.0 |
| 7 | 8 | 0 | 0.0 | 0 | 0.0 |
| 8 | 9 | 0 | 0.0 | 0 | 0.0 |
| 9 | 10 | 0 | 0.0 | 2 | 25.0 |
| 10 | 11 | 0 | 0.0 | 0 | 0.0 |
| 11 | 12 | 0 | 0.0 | 2 | 25.0 |
| 12 | 13 | 0 | 0.0 | 1 | 12.5 |
| Total | 8 | 100.0 | 8 | 100.0 | |
Bivariate analysis was conducted to examine the effect of sialang honey on wound bed score based wound bed preparation before and after intervention.
Based on Table 3 it could be concluded that sialang honey was effective in stimulating wound bed preparation in diabetic foot ulcer with p value of 0.011.
DiscussionsWound bed preparation would occur if the wound environment was balanced. To make the environment in the moisture wound balanced, in this study honey was used for being able to stimulate the occurrence of wound bed preparation.
Based on statistical tests it could be seen that honey could affect wound bed preparation. This was due to the content that honey has in that it could stimulate the wound bed preparation process
Honey was good for wound care is honey containing less than 20% water and less than 80% of honey content is sugar.8,9 The combination of water and sugar makes honey osmotic and can provide an environment with balanced moisture in the wound. The wound environment with the balance of moisture will stimulate the occurrence of wound bed preparation.8,9
Moisture balance triggers macrophages to produce collagenase and protease which were responsible for debridement through the separation and breakdown of proteins that keep dead tissue in the wound. When the protein was solved, the dead tissue would separate and debridement occurs. This process was also stimulated by neutrophils which would increase when the debridement process occurs.10,11
The success of honey therapy in maintaining moisture balance in the wound was affected by the use of the right dressing. This study combines honey as a topical therapy with gauze which functions as absorbance and transparent film which functions as an occlusive dressing. This method can retain moisture balance in the wound. This method was also good for preventing the seepage of honey out of the bandage in that honey was easy to melt when in contact with wounds that were warm.
This method was chosen based on a reflection of the research conducted by Evans and Mahoney. In Evans and Mahoney's research, secondary dressing used was foam which had high absorbance properties, but in that of the high absorbance properties it resulted in reduced effectiveness of honey as a debridement agent. Honey which should be able to moisturize the wound base was absorbed first by the foam to reduce the effect of honey.7
This was consistent with the statement of Sussman and Bates-Jensen that this wound bed preparation could be obtained through dressing that can retain moisture. This moist wound surface supports the rehydration of dead tissue and wound fluid consisting of white blood cells and this enzyme would break down necrotic tissue.12 Therefore with a combination of honey, gauze and transparent this film not only provides moisture but can also retain moisture.
Conclusions- 1.
The majority of respondents have suffered from diabetic foot ulcer for 1 month with a percentage of 62.5%.
- 2.
The day of treatment needed to remove dead tissue (wound bed preparation) starts from the 6th day. But there was one respondent who until the 14th day wound bed preparation has not happened well.
- 3.
After analyzing the data it could be concluded that sialang honey was effective in stimulating wound bed preparation in diabetic foot ulcer with a p value of 0.011.
The success and final outcome of this research required a lot of guidance and assistance from many people and I am extremely privileged to have got this all along the completion of our research.
I respect and thank to Ministry of Research, Technology and High Education for providing me an opportunity to do the research by through research grant programs.
I respect and thankful to all client who are willing to be respondents in this study.
I am thankful to and fortunate enough to get constant encouragement, support and guidance from all members of this research which helped us in successfully completing our research work.
Peer-review of abstracts of the articles is under the responsibility of the Scientific Committee of Riau International Nursing Conference 2018. Full-text and the content of it is under responsibility of authors of the article.