This study aimed to identify the effectiveness of using a multimodal approach to improve hand hygiene compliance among nurses. This research identifies how far the effectiveness of this method and its barriers.
MethodWe used the following databases to find full-text articles; Springer Link, Science Direct, and The Wiley Library. We used a “multimodal approach,” “hand hygiene,” “compliance,” and “infection control” as keywords. This article is a literature review.
ResultsBased on the articles reviewed, a multimodal approach is effective in improving hand hygiene compliance, but the range of compliance differ among countries. Commonly used approaches include the educational approach, which is particularly effective in improving hand hygiene compliance. Potential barriers complicate the process, including work culture, nurse beliefs, and organizational climate.
ConclusionHand hygiene compliance can be improved using a multimodal approach. Improving hand hygiene compliance is proven to decrease hospital-acquired infections. To overcome barriers that complicate this health campaign and to optimize all strategies, research and development must be continuously conducted.
There are two ways to prevent infection: standard precautions and prevention of transmission. Hand washing is one of the standard precautions for preventing infection and is effective in preventing transmission agents. Research shows that hand washing can reduce Central line-associated bloodstream infections (CLABSI) infections in the Intensive Care Unit (ICU).1 Other research has confirmed that hand hygiene or hand washing can stop cross-infection among nurses and patients,2 and hand hygiene has been reported to significantly decrease hospital-acquired infection.3 The WHO recommends a multimodal to improve nurses’ handwashing compliance. A multimodal approach combining strategies such as system changes, education and training, evaluation and reciprocity, reminders, and enhancing safety culture is effective in improving hand hygiene compliance.4,5 The WHO's recommendations have become health campaigns that have been carried out in various countries.
However, not all countries have implemented these recommendations. For instance, the implementation of a sustainable strategy still has barriers.6 Other barriers include nurse awareness, nurse perceptions about the importance of improving hand hygiene behavior,7 and a hospital organization that has not established a positive climate. Other known barriers are a program that has not reached the right target, a workplace culture that does not support the intervention, failure of managerial practice in a hospital ward, and costs of infection control. Therefore, the WHO has carried out continuous evaluations and developed interventions through research.
MethodThis study is a literature review that examined reliable sources. We used several electronic database search engines, including Springer Link, Science Direct, and Wiley Online Library. We used a “multimodal approach,” “hand hygiene,” “compliance,” and “infection control” as keywords.
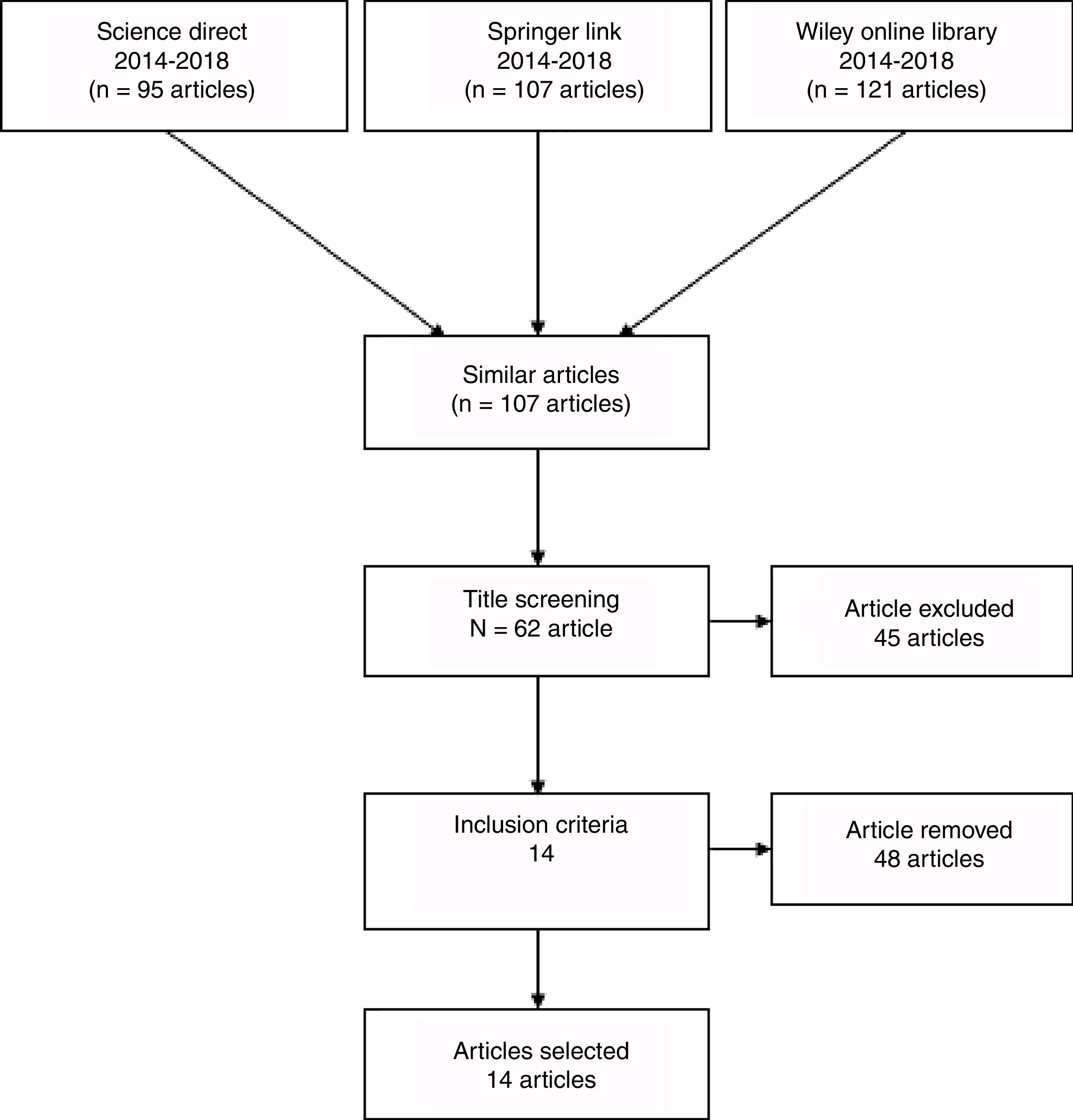
Most articles retrieved were experimental studies, RCTs, and descriptive research. The inclusion criteria were articles published in English from 2014 to 2018 that focused on hand hygiene, hand hygiene compliance, and multimodal approaches (Table 1). The exclusion criteria of this review were articles not written in English, articles published before 2013, and articles that did not focus on the topic. We found 107 articles and used PRISMA to choose relevant articles. Around 14 articles were selected and reviewed (Fig. 1).
Articles published in English from 2014 to 2018 that focused on hand hygiene.
| No. | Title | Sample | Method | Results |
|---|---|---|---|---|
| 1 | Hang, Hang, Anh, Zingg, & Pittet, 20158 | A total of 34,415 opportunities for hand hygiene during 2688 observation sessions | Direct observation | Hand hygiene compliance increased from 8% in 2010 to 52% in 2014. |
| 2 | Benedetta, Allegranzi & Pittet, 20149 | A group of samples used to be observed | Quasi-experimental research | Hand hygiene compliance increased from 51.3% to 98.6%. |
| 3 | Allegranzi et al., 20149 | There were 25,372 observations chances, with 22,501 compliance events, for an overall Hand Hygiene Compliance Rates (HHCR) is 88.7%. | Quasi-experimental research | Hand hygiene compliance improved from 72.7% (pretest) to 93.2% (posttest). |
| 4 | Midturi et al., 201510 | The study was conducted at six hospitals. The sample size was not stated clearly. | Quasi-experimental research | National compliance rates increased from 49.6% in 2005 to 69.1% in 2015 before the intervention, and from 68.6% in 2005 to 75.8% in 2013 after the intervention. |
| 5 | Fonguh, Hammami, Catry, Simon, & Hand, 201511 | A total of 2888, 2865, and 2244 opportunities for hand hygiene were observed during follow-up. | Direct observation before and six weeks after the intervention | Compliance with hand hygiene was 1.4% at baseline and increased to between 11.7% and 13.1% after follow-up. |
| 6 | Pfäfflin et al., 201712 | This research used 650 beds in a hospital. | Descriptive research | Hand hygiene compliance increased from 53.2% in 2008 to 72.6% 2014. |
| 7 | Kawagoe et al., 201513 | A total of 31,267 opportunities hand hygiene chances were observed. | Direct observation before and six weeks after the intervention | Hand hygiene compliance increased from 73% in 2010 to 88% in 2014. |
| 8 | Mustikawati, Syitharini, Widyaningtyastuti, & Gunawan, 201514 | A sample of 553 healthcare workers with a total of 5044 observations in 23 wards | Quasi-experimental research | Correct hand hygiene compliance increased from 66.27% and 47.75% at baseline to 80.53% and 88.35% after the intervention. |
| 9 | Scmitz et al., 20146 | Study location: a 278-bed university-affiliated teaching hospital in Addis Ababa | Quasi-experimental research | Hand hygiene compliance increased from 2.1% at baseline to 12.7%. |
| 10 | Hongsuwan, Srisamang, Day, Limmathurotsakul, & Cooper, 201515 | During the first phase of the research, a total of 15,797 opportunities for hand hygiene were observed. | Quasi-experimental research | Hand hygiene compliance was 46% before the intervention and increased to 69% after the intervention. |
| 11 | Shen et al., 201716 | A total of 5044 were hand hygiene opportunities observed. | Quasi-experimental research | Overall hand hygiene compliance improved from 66.27% to 80.53% among doctors (84.04%), nurses (81.07%), and other healthcare workers (69.42%). The rate at which the correct technique was used improved from 47.75% to 88.35%. |
| 12 | Watson, 201617 | A group of intervention groups was used. | Quasi-experimental research | Hand hygiene compliance improved from 51.3% to 98.6% among healthcare workers. |
| 13 | Ghezeljeh et al., 201518 | Hand hygiene chances Samples observed at 1408 beds. | Quasi-experimental research | Hand hygiene compliance improved from 62.3% during the first 4 months before the intervention to 73.3% in the 12 months following the intervention.Hand hygiene compliance improved from 69.1% to 81.2% among nurses, from 35.5% to 51.7% among physicians, and from 22.3% to 37.9% among nursing assistants. |
| 14 | Škodová 201519 | A group of intervention groups was used. | Quasi-experimental research | Hand hygiene compliance improved from 52% to 73% by indication. |
We reviewed 14 articles about the impact of using a multimodal approach to improve hand hygiene compliance among nurses. Most of the articles confirmed that multimodal approaches are effective in improving hand hygiene compliance. The rate of improvement ranged from at least 1.95% to 11% per year.
DiscussionThe hand hygiene compliance strategy was implemented in 2010 in all departments. The strategy included systemic changes by implementing a policy review and an infrastructure survey. Additional strategies included training and education, evaluation and feedback, monthly audits, and external audits. Reminders were also displayed in the workplace, such as posters in public areas, and/or were disseminated to staff by electronic media.20
The WHO has recommended a standard of hand hygiene compliance. Compliance should be practiced in two ways, at five moments, using six steps. Clinical nurses have to follow this recommendation to prevent infection.9,20 Cross infection will not be prevented optimally if an organization's hand hygiene process is sub-standard. Hand hygiene procedures must be practiced by all clinical nurses; hand hygiene self-reports are an evaluation tool for further improvement.21 Most hospitals, especially in developed countries, use systemic changes to improve hand hygiene compliance.9 A high-end technology monitoring system is a common systemic change. Moreover, several hospitals use Ultra Violet (UV) to strengthen hand hygiene results.22 Other strategies are improving the tools available in the ward, such as hand sanitizer, rubbing alcohol, and other necessary tools.
Education is the most commonly used method to improve hand hygiene compliance. Hospitals in various countries have a hand hygiene education program campaign in place.23 Various methods have been developed, such as seminary programs, workshops, and media development. This approach is effective in increasing nurses’ knowledge of, attitudes toward, and practices of hand hygiene. The educational tools and media that are available should be easily accessible by nurses. Positive results can be achieved using educational methods to improve hand hygiene.24
However, hand hygiene compliance is not always improved by having good facilities and a good system at a hospital ward; nurses’ hand hygiene beliefs and habits in hospital ward affect the work culture,25 which is a common barrier to hand hygiene.26 Ongoing education and the campaign may be the best choice to maintain positive nurse beliefs and culture. The first-line manager should create a positive workplace culture to improve nurses’ hand hygiene compliance.
Based on the articles reviewed, a multimodal approach is an effective methodology to improve nurses’ hand hygiene compliance. However, there is a problem with the continuity of nurse compliance. Therefore, evaluation and health campaign must be carried out continually. The goal of continuous socialization is to maintain the knowledge, beliefs, and adherence of nurses in carrying out hand washing.
A multimodal approach is suitable for hospital-acquired infection control. By improving the existing approach and system, a manager can decrease the prevalence of hospital-acquired infections (HAIs). A new approach cannot be implemented well if the managers at a hospital do not perform their roles effectively, starting from the first-line manager to the middle manager and the director. Managers play an important role in supporting this program, allowing the system of HAI prevention to run well.
Conflict of interestsThe authors declare no conflict of interest.
This work is supported by Hibah PITTA 2018 funded by DRPM Universitas Indonesia No. 1843/UN2.R3.1/HKP.05.00/2018.
Peer-review under responsibility of the scientific committee of the Second International Nursing Scholar Congress (INSC 2018) of Faculty of Nursing, Universitas Indonesia. Full-text and the content of it is under responsibility of authors of the article.