This was a 74-year-old male with a history of dyslipidaemia, arterial hypertension, atrophic kidney, obstructive sleep apnoea syndrome, permanent atrial fibrillation and heart disease since 2009. In 2021, he developed heart failure with double mitral and aortic lesions, for which in May 2022 he underwent cardiac surgery with double mitral and aortic valve replacement with a bioprosthesis and tricuspid ring, developing acute kidney failure requiring dialysis during that admission. After discharge, the patient led a normal life, being active and independent, until December 2022, when he went to the Accident and Emergency with a two-week history of dyspnoea on minimal effort. The most significant findings in blood tests on admission were: creatinine 1.74&#¿;mg/dl, leucocytes 8270, neutrophils 78.1%, CRP 11.7&#¿;mg/l, INR 4.63, platelets 129,000 and NT-proBNP 4768&#¿;pg/ml. Venous blood gas analysis showed pH 7.389, pCO2 43.1 and bicarbonate 26.
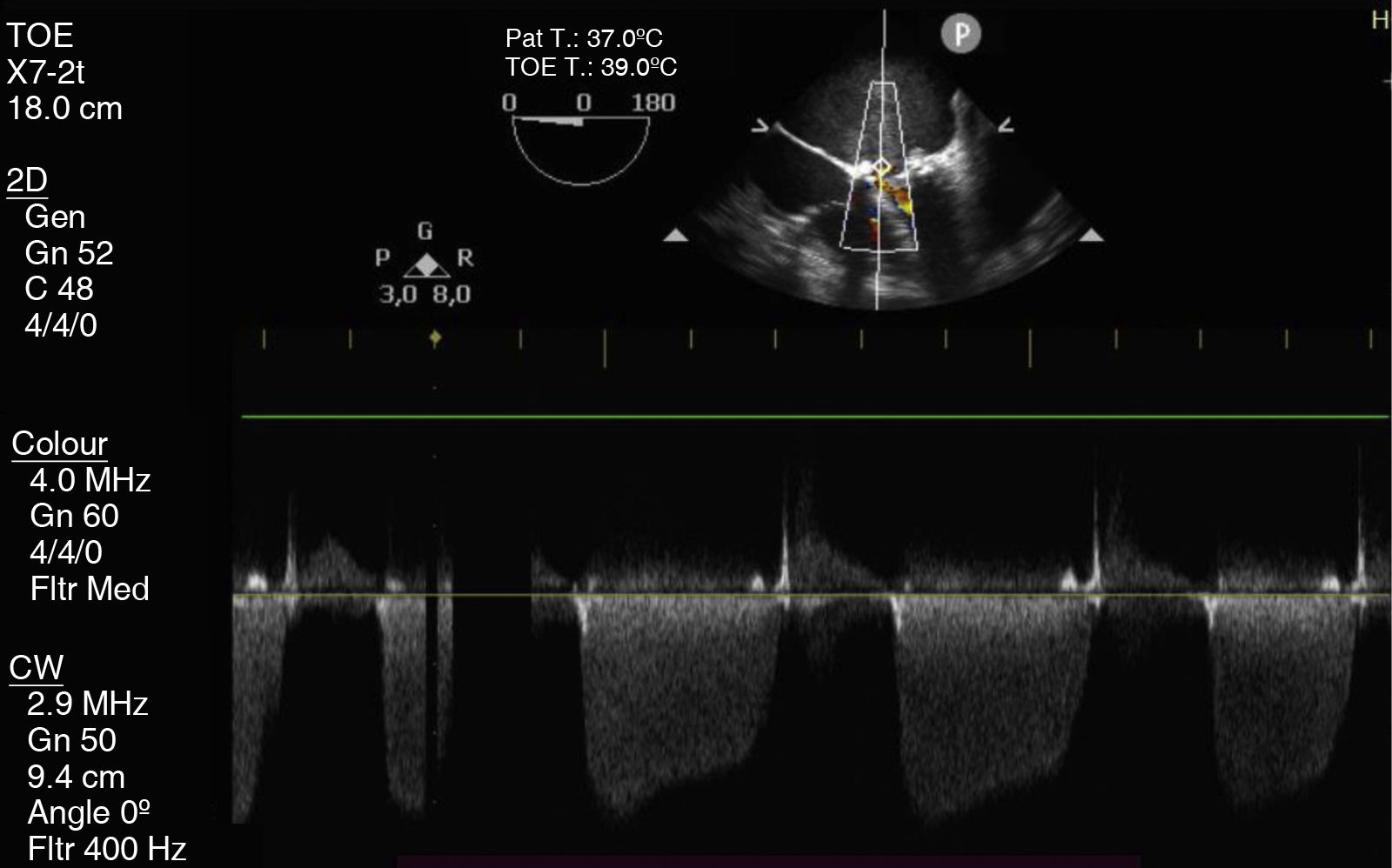
The patient was admitted with a diagnosis of decompensated heart failure with acute pulmonary oedema. On admission, the patient was haemodynamically unstable, requiring vasoactive drugs, in addition to having severe thrombocytopenia and exacerbated chronic kidney disease. Transoesophageal echocardiogram (TOE) (Fig. 1) revealed severe mitral stenosis secondary to mechanical obstruction due to possible thrombosis, as well as mild aortic valve insufficiency secondary to a mild peri-prosthesis aortic leak. Given these findings, cardiac surgery with mitral valve replacement was performed.
Clinical courseHistopathology examination of the valve revealed multiple hyphae whose thickness and lack of septation suggested Mucor spp., but with acute-angled branches, which meant that Aspergillus spp. could not be ruled out.
As two major Duke criteria were met, the patient was diagnosed with early prosthetic infective endocarditis of fungal origin and he was started on treatment with liposomal amphotericin B (3&#¿;mg/kg/day).
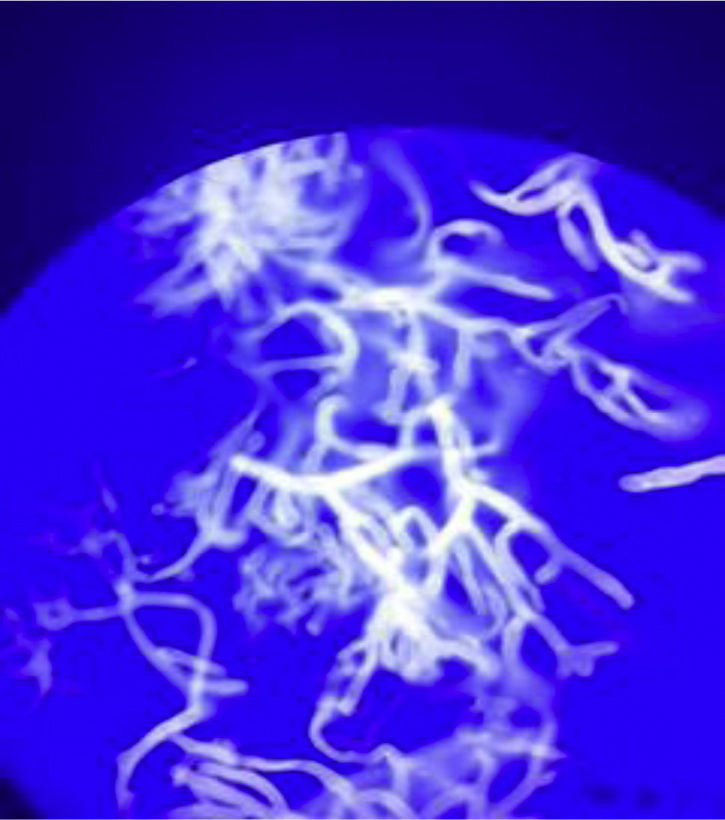
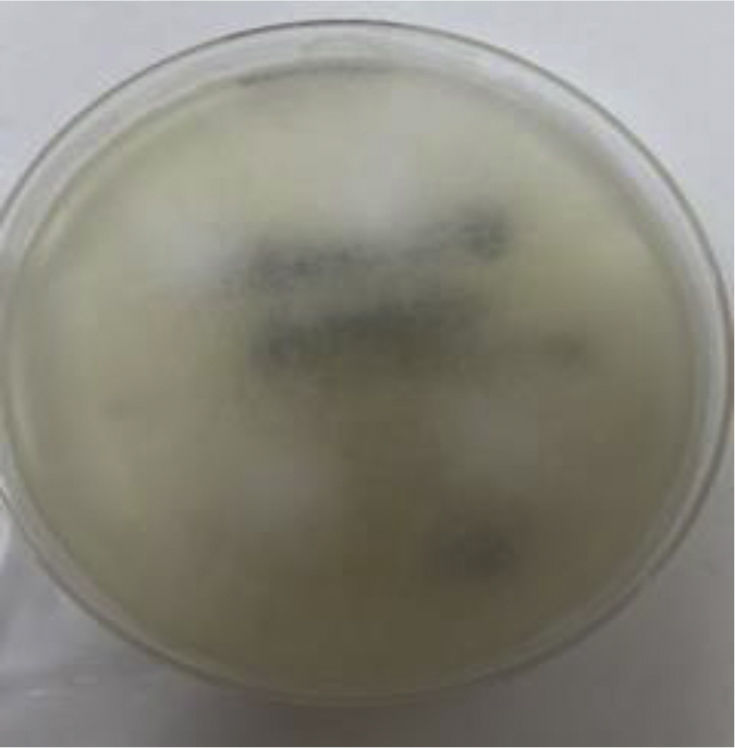
The microbiological diagnosis was made by microscopy with calcofluor white stain, where wide, non-septate hyphae were seen, consistent with the typical morphology of Mucor spp. (Fig. 2). In addition, heart valve culture was performed on Sabouraud dextrose agar at 25&#¿;°C, and abundant cottony colonies were seen after 48&#¿;h of incubation (Fig. 3). The definitive diagnosis was made by multiplex PCR for Zygomycetes in a reference centre, which identified it as Rhizopus oryzae. MALDI-TOF mass spectrometry (Bruker®) identified the same species.
During the first month postoperatively, the patient developed oligoanuric acute renal shutdown, with progressive reduced level of consciousness, desaturation and hypotension, requiring orotracheal intubation and connection to invasive mechanical ventilation. Transthoracic echocardiogram and TOE were performed, showing limited mitral valve opening with severe mitral stenosis, severe left atrial dilatation and right ventricular claudication. Based on these findings, urgent surgery was performed to replace the mitral valve. In the second operation, the mitral prosthesis was found to have large vegetations, infiltrating the wall and the papillary muscles, lacerations of both lungs, which were repaired with haemostatic patches, and significant dilatation of the left atrium. After this, the patient became severely unstable haemodynamically, requiring high doses of vasoactive drugs. He arrived at the resuscitation unit from the operating theatre in refractory cardiogenic shock and unfortunately died a few hours later. No post-mortem examination was performed.
Closing remarksMucormycosis is a potentially fatal fungal infection by fungi of the order Mucorales, which occurs primarily in immunocompromised patients.1 Cardiovascular mucormycosis is very rare and usually causes death within a short period of time.2 The main predisposing factors for mucormycosis are diabetes mellitus, haematological neoplasm, prolonged treatment with corticosteroids or deferoxamine, metabolic acidosis and AIDS.1,2
Fungal endocarditis is very rare, especially due to Mucorales, but it is considered the most serious form of infective endocarditis. Features of fungal endocarditis include large vegetations, with an increased potential for embolisation and a tendency to grow on prosthetic valves.2
Treatment is based on a combination of surgery and early antifungal therapy, with liposomal amphotericin B being the treatment of choice. However, the prognosis is very poor despite adequate treatment, with a high associated mortality rate.2,3