To determine DBI and its relationship with polypharmacy and pharmacotherapeutic complexity (PC) in a cohort of PLWH over 50 years of age at follow-up of pharmacotherapy in a tertiary hospital.
MethodsObservational and retrospective study that included PLWH in active antiretroviral treatment over 50 years of age who have been followed up in outpatient pharmacy services. Pharmacotherapeutic complexity was estimated through Medication Regimen Complexity Index (MRCI). Collected variables included comorbidities, current prescriptions and its classification according to anticholinergic and sedative activity and associated risk of falls.
ResultsStudied population included 251 patients (85.7% men; median age: 58 years, interquartile range: 54–61). There was a high prevalence of high DBI scores (49.2%). High DBI was significantly correlated with a high PC, polypharmacy, psychiatric comorbidity and substances abuse (p<0.05). Among sedative drugs, the most prescribed were anxiolytic drugs (N05B) (n=85), antidepressant drugs (N06A) (n=41) and antiepileptic drugs (N03A) (n=29). For anticholinergic drugs, alpha-adrenergic antagonist drugs (G04C) were the most prescribed (n=18). Most frequent drugs associated with risk of falls were anxiolytics (N05B) (n=85), angiotensin-converting enzyme inhibitors (C09A) (n=61) and antidepressants (N06A) (n=41).
ConclusionThe DBI score in older PLWH is high and it is related to PC, polypharmacy, mental diseases and substance abuse as is the prevalence of fall-related drugs. Control of these parameters as well as the reduction of the sedative and anticholinergic load should be included in the lines of work in the pharmaceutical care of people living with HIV+.
Determinar la relación del Drug Burden Index (DBI) con la polifarmacia y complejidad farmacoterapéutica en pacientes con virus de la inmunodeficiencia humanamayores de 50 años en un hospital de tercer nivel.
MétodosEstudio observacional, retrospectivo en el que se incluyó a pacientes mayores de 50 años en tratamiento antirretroviral (TAR) activo que acudieron a la consulta de farmacia del hospital. El índice de complejidad farmacoterapéutica se calculó a través de la herramienta Medication Regimen Complexity Index (MRCI). Se recogieron variables que incluyeron las comorbilidades, prescripción actual de fármacos y su clasificación en función de la actividad anticolinérgica, sedante o su relación con el riesgo de caídas.
ResultadosSe incluyó a 251 pacientes, el 85,7% hombres, con una mediana de edad de 58 años (RIQ: 54-61). El 49,2% de los pacientes presentó una puntuación DBI elevada. Valores altos de DBI se correlacionaron de forma significativa con alto IC, presencia de comorbilidad mental, patrón de multimorbilidad, consumo de tóxicos y presencia de polifarmacia. Entre los fármacos sedantes, los fármacos más prescritos fueron ansiolíticos (N05B) (n=85), antidepresivos (N06A) (n=41) y antiepilépticos (N03A) (n=29). Entre los fármacos anticolinérgicos, destacan los antagonistas alfa-adrenérgicos (G04C (n=18). Los fármacos asociados a recaídas más prescritos fueron los ansiolíticos (N05B) (n=85), seguidos de los inhibidores de la enzima conversora de la angiotensina (C09A) (n=61) y antidepresivos (N06A) (n=41).
ConclusiónEl DBI elevado se relaciona con la presencia de alta complejidad farmacoterapéutica, enfermedad mental, consumo de tóxicos y la presencia de polifarmacia. Monitorizar estos aspectos, así como reducir la carga sedante y anticolinérgica, debería ser incluido en las líneas de trabajo de atención farmacéutica a las personas que viven con virus de la inmunodeficiencia humana.
Polypharmacy is an increasingly important aspect to evaluate in people living with HIV+ (PLWH). Possible interactions of concomitant medications with antiretroviral therapy (ART)1 as well as the presence of potentially inappropriate drugs are factors that makes it a challenge.2,3 Within these, both sedative and anticholinergic drugs could cause cognitive impairment as side effects with an increase in risk of falls as a consequence.
The risk factors that increase the likelihood of falls may be related to the individual (normal aging process or chronic diseases) and/or the environment increasing the number of falls as a result of their interaction.4 Although some of the factors cannot be changed, others are modifiable. Among them, the use of certain medications is a modifiable risk factor which is recognized as relevant in increasing the risk of falls, especially in elderly people.5
Multifactorial interventions are recommended for fall prevention, consisting of a fall risk assessment accompanied by one or more risk reduction strategies within a coordinated program. These interventions focus on three components: physical exercise, medication review, and home risk intervention.6
The Drug Burden Index (DBI) is a score that measures the exposure of patients to sedative and anticholinergic drugs.7 These effects can be considered as Class A adverse effect,8 which are those related to the mechanism of action of the drug and are, therefore, predictable. They can be defined as the result of an increased response to the administered dose due to pharmaceutical, pharmacokinetic or pharmacodynamic alterations.
The aging of PLWH is associated with an increase in comorbidities and, consequently an increase also in the number of drugs included in their treatment. The prevalence of potentially inappropriate drugs in this population is high with the consequent development of adverse events and even psycho-geriatric comorbidities. The evaluation of DBI allows us to obtain a picture of how these drugs influence the patient and the possibility of developing strategies to minimize their negative consequences. This score gives us a measure of overall exposure to medications with anticholinergic and sedative properties that implements the principle of dose response to determine the effect of medication exposure.
Another concept used to evaluate patient treatment is the pharmacotherapeutic complexity (PC).9 In a recently published article, a complex patient is defined as a patient with a Medication Regimen Complexity Index (MRCI) value equal to or greater than 11.25.10
The importance of these groups of drugs in both the general population and PLWH lies in their prevalence of prescription. It is estimated that 50% of patients over 50 years of age have at least one drug included in these groups. A recently published study refers to the use of this index to identify elderly patients at risk of falls associated with their pharmacotherapy.11 Various studies using DBI have been performed in the general population, but it has not yet been used in the HIV+ population. By utilizing this resource as a new indicator to optimize therapy, strategies such as deprescription could be developed.
The purpose of this study is to determine DBI and its relationship with polypharmacy and PC in a cohort of PLWH over 50 years of age at follow-up of pharmacotherapy in a tertiary hospital.
Material and methodsDesign and populationObservational and retrospective study that included PLWH in active antiretroviral treatment over 50 years of age who have been followed up in outpatient pharmacy services from January to May 2021. PLWH under 50 years of age, included in clinical trials or expanded drug access programs were excluded.
The dependent variable was considered to be the DBI value, which was calculated following the procedure described by O’Connell et al.8 The numerical value was calculated and classified into high (DBI score>1), medium (0.5–1) and low (<0.5) risk as described in the literature.11
Independent variables were demographic (age, sex), ART, type of ART used, use of a single tablet regimen (STR), comorbidities, number of active comedications, polypharmacy, MRCI, presence of sedative drugs, presence of anticholinergic drugs, presence of drug associated with falls and use of health resources.
Patients were classified according to the received ART, either two nucleoside/nucleotide reverse transcriptase inhibitors (NRTI) and one non-nucleoside reverse transcriptase inhibitor (NNRTI), or two NRTIs and one protein inhibitor (PI) or two NRTIs and one integrase inhibitor (INI) and other ART schemes, according to the Spanish GESIDA/PNS consensus document on recommendations for the beginning of ART.12 STRs were also identified, consisting of an ART that is administered as a single tablet only once a day.
Comorbidities were classified according to the multimorbidity pattern of Prados-Torres et al.13
The medications considered were those prescribed for at least 6 months prior to the start of the study. Polypharmacy was defined as the use of six concomitant drugs (including ART). We also considered major polypharmacy, defined as the use of 11 or more concomitant drugs, and extreme polypharmacy, as the use of 21 or more concomitant drugs.
The index used to calculate PC was the MRCI. This index allows the calculation of medication complexity considering the following three sections: dosage form, posology, and additional administration instructions.9 Classification into high or low PC was performed based on the study by Morillo et al. (2019), in which the polypharmacy detection threshold is defined with a score of MRCI of 11.25 points.10 The total complexity of the prescribed medication was estimated at the time of data collection. The complexity of the different sections of the MRCI was also analyzed from a quantitative and qualitative perspective.
Drugs with an anticholinergic effect were selected using the Osakidetza classification of anticholinergic drugs from their INFAC 2019 bulletin.14 Drugs with local anticholinergic properties, such as inhalers or ophthalmic formulations, were not taken into account, as no systemic anticholinergic effect has been demonstrated.
Drugs associated with falls were selected according to possible effects related to their use: sedation, somnolence, hypoglycemia, confusion, vestibular damage (deafness and tinnitus), orthostatic hypotension, postural instability, hypothermia, dehydration, vision problems, parkinsonism, decreased blood pressure or reduced heart rate.15
To be able to establish the categories of the different drugs, they were classified according to their ATC group using only the first three levels of classification (1st level: anatomical; 2nd level: therapeutic subgroup; 3rd level: pharmacological subgroup).
To assess the use of health resources, visits to the emergency room, hospital admissions and falls/fractures in the last year were taken into account.
Data were collected from patient medical records and by accessing institutional applications of the Andalusian Public Health System: electronic prescription, digital health record, as well as specific databases and outpatient management programs of the Pharmacy service.
Statistical analysisQuantitative variables were summarized with means and standard deviations, or with medians and percentiles 25th (P25) and 75th (P75), in the case of asymmetric distributions, and qualitative variables with frequencies and percentages. To study the relationships between qualitative variables, contingency tables and the Chi-square test were performed, or the non-asymptotic methods of the Monte Carlo test and the exact test. Significance was interpreted in the contingency tables using Haberman residuals. Normality was checked with the Kolmogorov–Smirnov test, to determine the use of parametric or nonparametric tests. For all contrasts, an alpha level of 0.05 was considered significant.
To facilitate statistical analysis, the main variable was classified into high or low DBI according to whether they had a DBI score ≥1 (high) or <1 (low). To analyze the relationship between quantitative and qualitative variables, Student's t test was used for independent samples and Mann–Whitney U test for nonparametric samples.
Data analysis was performed with the IBM SPSS 20.0 statistical package for Windows.
ResultsA total of 251 patients (85.7% men) with a median age of 58 [interquartile range (IQR): 54–61] years met the inclusion criteria. 10.8% of the study population were 65 years or older.
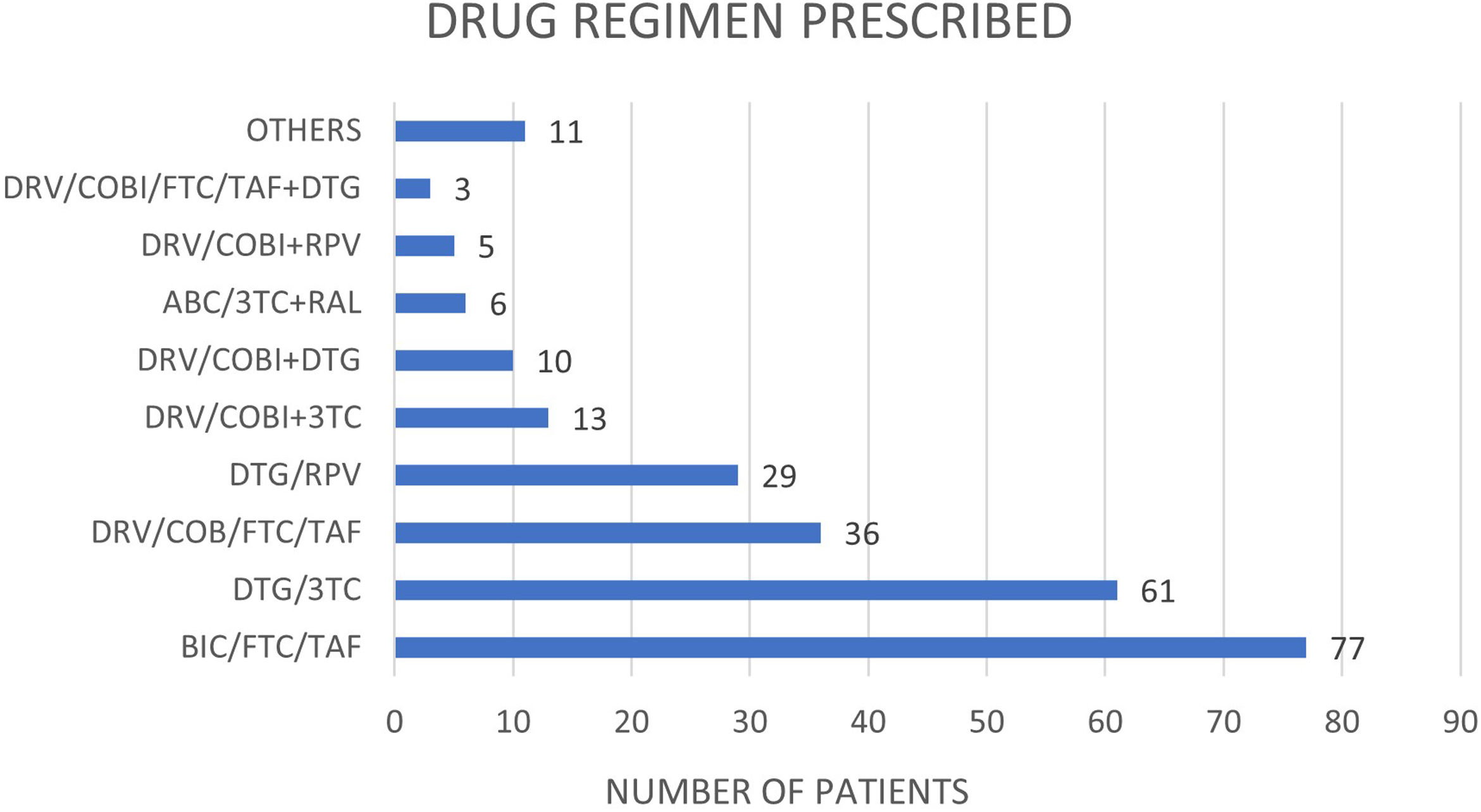
Regarding the ART prescribed, regimens based on an InIn (60.0%) and IP/P (20.7%) were the most predominant whereas 1 patient presented a regimen based on ITINN. The rest of patients presented a non-standard ART (19.9%). As for the type of therapy, triple therapies and bitherapies were the most frequent in equal parts (49.4% and 49.4% respectively), followed by a minor presence of monotherapy (0.4%) or another kind of therapy (1.2%). BIC/FTC/TAF combination (30.7%), followed by DTG/3TC (24.3%) and DRV/COB/FTC/TAF (14,3%) combinations were the most observed ART (Fig. 1). The four most used combinations are available as a STR regimen (80.8%).
Regarding comorbidities, 78.6% (n=195) of the patients had a cardiovascular comorbidity, 70.2% (n=174) had liver disease, 19.0% has a psychiatric comorbidity (n=47), 14.3% (n=36) had renal impairment, 13.3% (n=33) had a lung condition, 12.7% (n=32) had a sexually transmitted disease and 8.0% had cancer. Harmful consumption of toxic substances, including tobacco and alcohol, was observed in 37.0% of the patients. Of the patients in whom the multimorbidity pattern could be estimated (73.6%), 85.6% of the patient had a cardio-metabolic pattern, 10.5% had a psycho-geriatric, 3.3% had a mixed and 0.5% had a mechanical-thyroid pattern.
The patients had a median of 6 (IQR: 4–9) of concomitant drugs prescribed, 4 (IQR: 2–7) if considered as pill number. Polypharmacy was observed in 50.6% (n=127) of the patients. The 11.6% (n=29) met the criteria for major polypharmacy whereas two patients presented extreme polypharmacy.
The PC of total treatment (T-PC) was 9 (IQR: 5–15) whereas the PC associated with TAR (TAR-PC) and the concomitant medication-associated PC (CM-PC) were 2 (2–3) and 6 (2–12) respectively. The median specific complexity index of the T-PC factors was 2 (IQR: 2–4) for the pharmaceutical form, 4 (IQR:4–9) for posology, and 1 (IQR: 1–2) for the requirements of specific instructions. 36.3% (n=91) of the patients had T-PC values greater than 11.25.
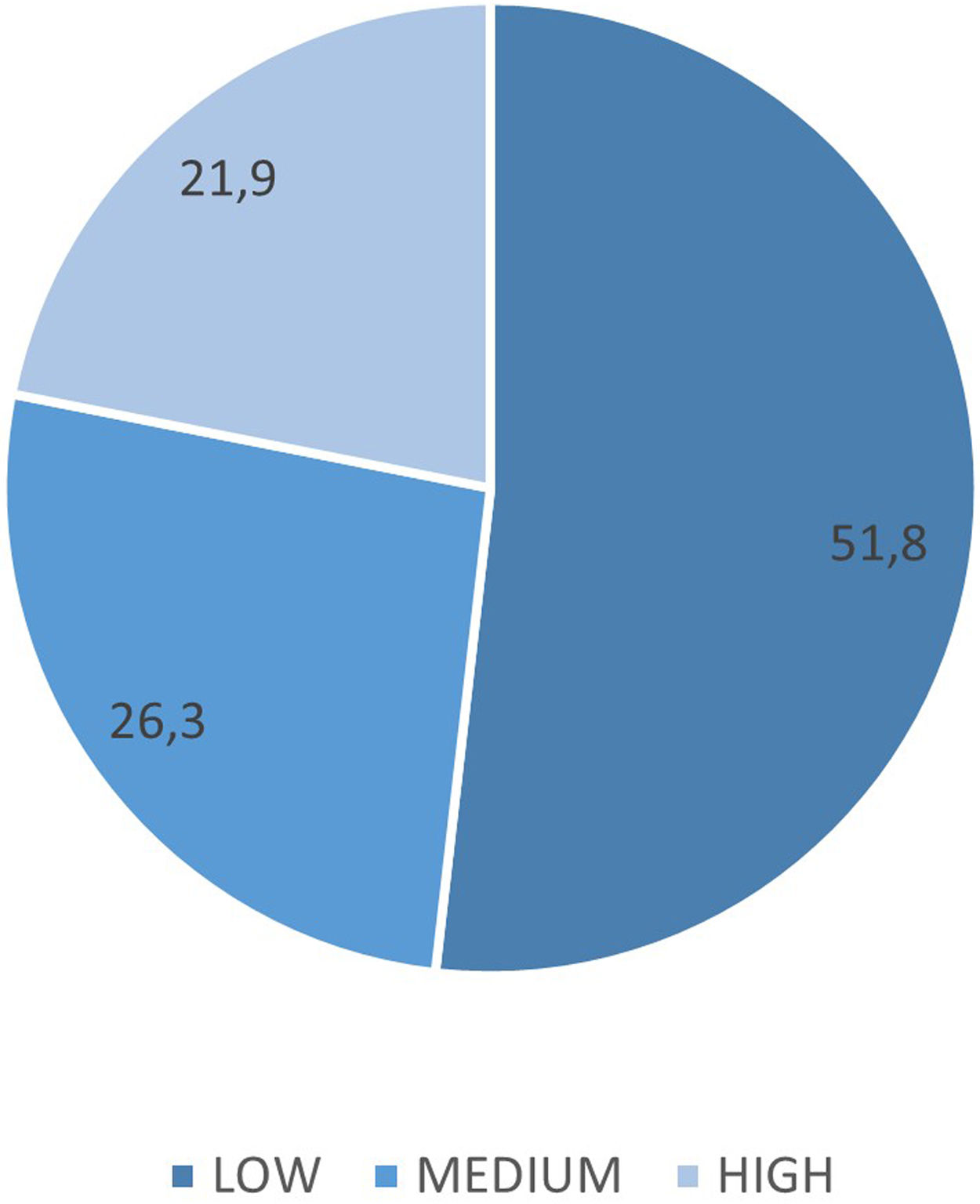
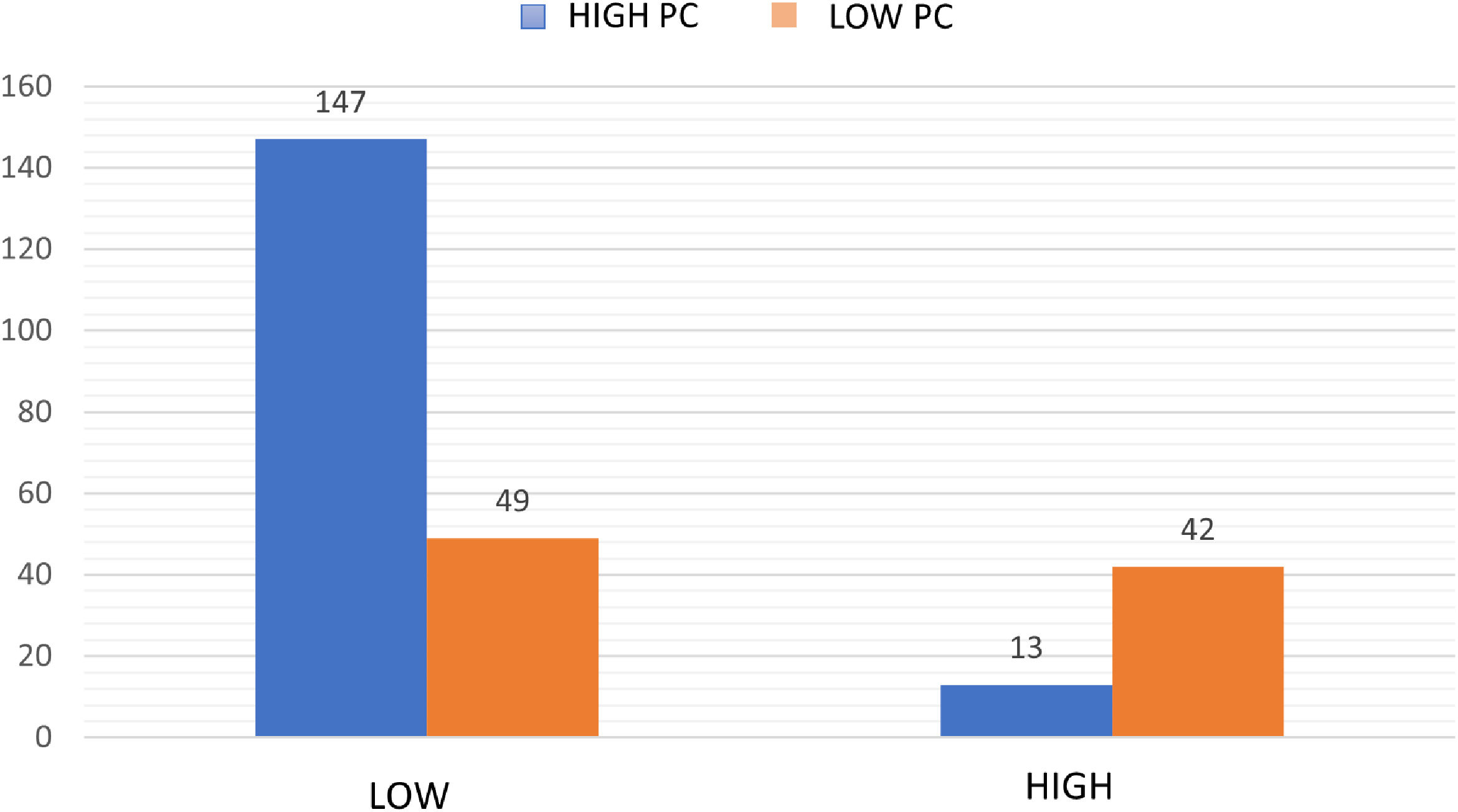
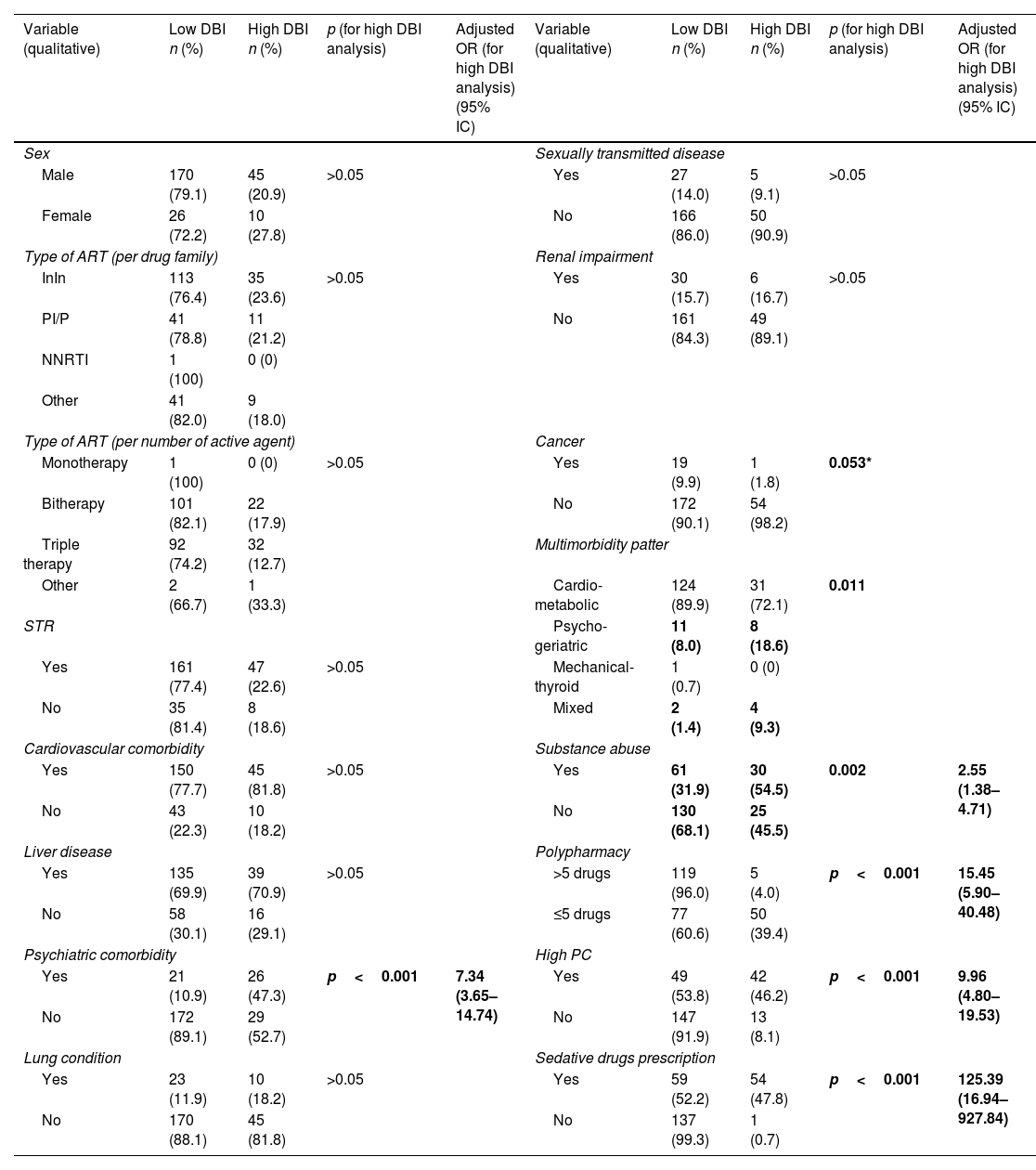
The median DBI median score was 0.90 (IQR: 0.67–1.60). More than half of the patients had a low level of DBI (51.8%) followed by a medium (26.3%) and high level of DBI (21.9%) (Fig. 2). The DBI score and PC were significantly correlated (r=0.64; p<0.001) so that the higher the pharmacotherapeutic complexity, the higher the DBI score will be expected (Fig. 3, Table 1). 45.0% of the patients were prescribed a sedative drug with a median of 1 per patient (IQR: 1–2) whereas 24.3% were prescribed an anticholinergic drug with a median of 1 per patient (IQR: 1–1). Drugs associated with an increased risk of falls were detected in 64.9% of the patients with a median of 2 per patient (IQR: 1–3).
Qualitative and quantitative analysis of DBI.
| Variable (qualitative) | Low DBI n (%) | High DBI n (%) | p (for high DBI analysis) | Adjusted OR (for high DBI analysis) (95% IC) | Variable (qualitative) | Low DBI n (%) | High DBI n (%) | p (for high DBI analysis) | Adjusted OR (for high DBI analysis) (95% IC) |
|---|---|---|---|---|---|---|---|---|---|
| Sex | Sexually transmitted disease | ||||||||
| Male | 170 (79.1) | 45 (20.9) | >0.05 | Yes | 27 (14.0) | 5 (9.1) | >0.05 | ||
| Female | 26 (72.2) | 10 (27.8) | No | 166 (86.0) | 50 (90.9) | ||||
| Type of ART (per drug family) | Renal impairment | ||||||||
| InIn | 113 (76.4) | 35 (23.6) | >0.05 | Yes | 30 (15.7) | 6 (16.7) | >0.05 | ||
| PI/P | 41 (78.8) | 11 (21.2) | No | 161 (84.3) | 49 (89.1) | ||||
| NNRTI | 1 (100) | 0 (0) | |||||||
| Other | 41 (82.0) | 9 (18.0) | |||||||
| Type of ART (per number of active agent) | Cancer | ||||||||
| Monotherapy | 1 (100) | 0 (0) | >0.05 | Yes | 19 (9.9) | 1 (1.8) | 0.053* | ||
| Bitherapy | 101 (82.1) | 22 (17.9) | No | 172 (90.1) | 54 (98.2) | ||||
| Triple therapy | 92 (74.2) | 32 (12.7) | Multimorbidity patter | ||||||
| Other | 2 (66.7) | 1 (33.3) | Cardio-metabolic | 124 (89.9) | 31 (72.1) | 0.011 | |||
| STR | Psycho-geriatric | 11 (8.0) | 8 (18.6) | ||||||
| Yes | 161 (77.4) | 47 (22.6) | >0.05 | Mechanical-thyroid | 1 (0.7) | 0 (0) | |||
| No | 35 (81.4) | 8 (18.6) | Mixed | 2 (1.4) | 4 (9.3) | ||||
| Cardiovascular comorbidity | Substance abuse | ||||||||
| Yes | 150 (77.7) | 45 (81.8) | >0.05 | Yes | 61 (31.9) | 30 (54.5) | 0.002 | 2.55 (1.38–4.71) | |
| No | 43 (22.3) | 10 (18.2) | No | 130 (68.1) | 25 (45.5) | ||||
| Liver disease | Polypharmacy | ||||||||
| Yes | 135 (69.9) | 39 (70.9) | >0.05 | >5 drugs | 119 (96.0) | 5 (4.0) | p<0.001 | 15.45 (5.90–40.48) | |
| No | 58 (30.1) | 16 (29.1) | ≤5 drugs | 77 (60.6) | 50 (39.4) | ||||
| Psychiatric comorbidity | High PC | ||||||||
| Yes | 21 (10.9) | 26 (47.3) | p<0.001 | 7.34 (3.65–14.74) | Yes | 49 (53.8) | 42 (46.2) | p<0.001 | 9.96 (4.80–19.53) |
| No | 172 (89.1) | 29 (52.7) | No | 147 (91.9) | 13 (8.1) | ||||
| Lung condition | Sedative drugs prescription | ||||||||
| Yes | 23 (11.9) | 10 (18.2) | >0.05 | Yes | 59 (52.2) | 54 (47.8) | p<0.001 | 125.39 (16.94–927.84) | |
| No | 170 (88.1) | 45 (81.8) | No | 137 (99.3) | 1 (0.7) | ||||
| Anticholinergic drugs prescription | Variable (quantitative) | n | Mean | Standard deviation | p | ||||
|---|---|---|---|---|---|---|---|---|---|
| Yes | 30 (49.2) | 31 (50.8) | p<0.001 | 7.14 (3.69–13.82) | Age | ||||
| No | 166 (87.4) | 24 (12.6) | Low DBI | 196 | 58.73 | 7.01 | >0.05 | ||
| Drugs associated with falls | High DBI | 55 | 57.51 | 5.68 | |||||
| Yes | 108 (66.3) | 55 (33.7) | p<0.001 | 1.51 (1.35–1.68) | Total number of drugs | ||||
| No | 88 (100) | 0 (0) | Low DBI | 196 | 5.85 | 3.17 | p<0.001 | ||
| Emergency room visit | High DBI | 55 | 8.22 | 3.96 | |||||
| Yes | 102 (53.7) | 35 (66.0) | >0.05 | T-PC (Total pharmacotherapeutic complexity index score) | |||||
| No | 88 (46.3) | 18 (34.0) | Low DBI | 196 | 8.70 | 6.31 | p<0.001 | ||
| Hospital admission | High DBI | 55 | 18.47 | 10.04 | |||||
| Yes | 27 (85.8) | 8 (84.9) | >0.05 | Number of sedative drugs | |||||
| No | 163 (14.2) | 45 (15.1) | Low DBI | 60 | 1.08 | 0.38 | p<0.001 | ||
| Falls/fracture | High DBI | 54 | 2.76 | 1.30 | |||||
| Yes | 9 (4.7) | 1 (1.9) | >0.05 | Number of drugs with high anticholinergic activity | |||||
| No | 181 (95.3) | 52 (98.1) | Low DBI | 16 | 1.00 | 0.00 | >0.05 | ||
| Chi-square test and t-student independent variables (p<0.05)High DBI score corresponds to a value of ≥1Low DBI score corresponds to a<1 DBI punctuation | High DBI | 10 | 1.10 | 0.32 | |||||
| Number of drugs with low anticholinergic activity | |||||||||
| Low DBI | 22 | 1.00 | 0.00 | p<0.001 | |||||
| High DBI | 26 | 1.46 | 0.64 | ||||||
| Number of drugs associated with falls | |||||||||
| Low DBI | 107 | 1.87 | 1.07 | p<0.001 | |||||
| High DBI | 54 | 3.20 | 1.52 | ||||||
Bold values are those that reach statistical significance (p<0.05).
Among sedative drugs, the most observed were anxiolytic drugs (N05B) (n=85), antidepressant drugs (N06A) (n=41) and antiepileptic drugs (N03A) (n=29). The main prescriptions were two short-acting benzodiazepines (alprazolam and lorazepam) and a long-acting benzodiazepines (diazepam).
For anticholinergic drugs, alpha-adrenergic antagonist drugs used for benign prostatic hyperplasia (G04C), such as tamsulosin and silodosin, were the most prescribed (n=18) among those with high anticholinergic activity. Among drugs with low anticholinergic activity, anxiolytics (N05B) (mainly diazepam (n=21)) and opioid analgesics (N02A) (mainly tramadol (n=11)) were the most prescribed.
The drugs associated with the risk of falls in the study cohort were anxiolytics (N05B) with 85 prescriptions, followed by angiotensin-converting enzyme (ACE) inhibitors (C09A) with 61 prescriptions, and antidepressants (N06A) with 41.
Finally, with regard to healthcare utilization, 56.4% of the patients (n=137) visited the emergency department at least once during the previous year, 14.4% (n=35) were hospitalized, and 4.1% (n=10) experienced a fall/fracture documented in health records. A statistically significant relationship was found between DBI and the following variables: polypharmacy, high PC, psychiatric comorbidity, multimorbidity patter, substance abuse and prescription of sedative, anticholinergic and falls-associated drugs (Table 1).
DiscussionThe results of this study show a high prevalence of high DBI scores (DBI≥1) (49.2%) among HIV patients over 50 years of age, with a median DBI score of 0.9 points. Among the factors related to high DBI scores, polypharmacy, high T-PC, mental disorder and substance abuse have been identified.
In a large number of patients, the prescription of sedative drugs, especially anxiolytics and antidepressants, as well as several drugs with a moderate anticholinergic load, are often prescribed. These drugs can have an additive effect when used together. Among the drugs associated with falls that are not related to the central nervous system, prescription of ACE inhibitors, beta-blockers and thiazide diuretics, which produce bradycardia, orthostatic hypotension, and possible emergency incontinence, were the most common.
Currently, there are no studies that assess the DBI scale in HIV patients, although it has been studied in other elderly populations. These studies have established a relationship between DBI score and their risk of hospitalization, as well as physical and cognitive deterioration.16 There are studies with other scales, such as the ACB (Anticholinergic Cognitive Burden) or the ARS (Anticholinergic Risk Scale) that exclusively assess anticholinergic drugs. The study by Mazzitelli et al. uses the ACB and ARS tools with 14.5% of patients prescribed anticholinergic drugs and 26.9% of them with high anticholinergic risk.17 Casajus-Navasal et al. used the same tools and observed 43.3% and 36.4% of patients with high anticholinergic burden according to the ACB and ARS scales, respectively, as well as 26.2% and 17.2% of patients taking at least one anticholinergic drug according to the same scales.18 These data on anticholinergic use are consistent with the prescriptions in this study, in which 24.3% of the patients were prescribed at least one high- and low-potency anticholinergic drug.
The DBI score assesses both sedative and anticholinergic medications, making it a more complete tool for assessing these patients. HIV patients have been found to experience neuropsychiatric symptoms such as anxiety, depression, and sleep disorders at a higher rate than the general population.19 As a result, the use of drugs from the central nervous system, particularly sedative and anxiolytic drugs, is especially important in these patients, and measuring their use is of great utility. The use of these drugs is more frequent in PLWH compared to the general population and has been associated with a worse neuropsychological state and a decrease in brain integrity, especially in HIV patients.20
Regarding the use of sedative drugs, the study by Casajus-Navasal et al. highlights 30.5% of patients with benzodiazepine prescription versus 43.1% observed in the present work.18 Similar data on benzodiazepine consumption is described in the study by Contreras et al.21
Several studies associate an increased risk of falls to the presence of polypharmacy22 or to certain drugs such as antidiabetics or antidepressants,23 but the evidence is still scarce.
The prevalence of polypharmacy is high, in line with the aging of the patient cohort, affecting more than half of the target population (50.6%). This is at the upper limit of what have been reported in other analogous studies in the HIV population both internationally24–26 and in studies published in national cohorts,27–29 which approach percentages of 30% of patients with polypharmacy. It should be noted that not all published studies were conducted in the elderly population (over 50 years of age).
Likewise, the prevalence of high overall PC is 36.3% of patients, primarily due to the complexity associated with concomitant medications rather than ART. With STR combinations, this prevalence has drastically decreased. This has already been described in other studies, such as Metz et al., who also identified concomitant medication as the main contributor to T-PC.30
This study presents a population with high PC, especially due to the complexity of concomitant medication since ART complexity has decreased in recent years due to the commercialization of new drug families.31 The arrival of new drug formulations based on InIn in STR regimen, both in bitherapy and triple therapy, has contributed to a decrease in treatment complexity. These new formulations offer ease of administration, as they can be taken once daily and are not influenced by food.
Increasingly, the complexity index is being studied in different populations, especially in PLWH. Several works have been published in this regard,32 although not all use the MRCI tool for its calculation. Zhou et al. (2014) were among the first authors to assess the dosing burden in PLWH.33 They observed a median number of prescribed drugs and pharmaceutical forms slightly higher than those described in the present work.
Contreras et al. (2021), in an HIV population without age restrictions, observed a slightly lower mean MRCI than the one detected in this study (6.9±5.5) with 20.6% of patients presenting a high complexity index.34 This difference may be due to the study being developed in HIV patients older than 18 years. Younger patients usually have a lower PC due to the absence of comorbidities.
Although the cross-sectional study design is the most appropriate for determining DBI and the prevalence of the population with high DBI, it has limitations in establishing causal relationships due to its timeless nature. However, this does not detract from the validity of the results obtained here, which serve as a working hypothesis for future lines of research based on the results obtained. Another possible limitation lies in the fact that we could underestimate the prescriptions of sedative and anticholinergic drugs and, therefore, the DBI value, since we have not included medications not considered chronic or over-the-counter (OTC) or sporadic use or recommended in the community pharmacy for minor ailments or minor symptoms. We believe that this element may be important and should be included in future studies, since many OTC or sporadic prescription drugs may have anticholinergic activity. Finally, another limitation is that the relationship between DBI and quality of life scales or patient reported outcomes has not been studied.
ConclusionThis study has shown the relevance of DBI value in HIV patients. The DBI score in the studied population is high, as is the prevalence of fall-related drugs. Therefore, the control of polypharmacy and the PC, as well as the reduction of the sedative and anticholinergic load, should be included in the lines of work in the pharmaceutical care of HIV patients, with a multidimensional approach within strategies of deprescription and review of potentially inappropriate drugs, in order to improve the health outcomes of patients.
AuthorshipR-MV and MA-RC – conception and design of the manuscript. MA-RC – data collection, analysis and interpretation of data. FA-LD – writing of the manuscript. R-MV, MA-RC and FA-LD – review and approval of the final document.
Ethics approvalThis study was approved by the Research Ethics Committee of the hospital where the research was conducted (1230-N-21).
FundingWe have received funding to carry out this study.
Conflict of interestNothing to declare.
To Celia Parrado Castaño, of the University of Seville.