A 52 years old male with no relevant medical history, presented to the Emergency Department with fever of 39°C, vomiting, diarrhea, and dark urine for 5 days after returning 15 days ago from a one-month stay in Ghana (August–September 2023). He had gone to visit his wife, who was working temporarily in that country. He reported complete local vaccination (and he had positive history of IgG for hepatitis A virus). He had not attended a travel clinic before traveling and did not take chemoprophylaxis for malaria, although he did use DEET repellent and a mosquito nets.
On arrival, he presented with poor general condition, generalized jaundice, tachycardia 150bpm, tachypnea 40rpm, blood pressure 130/85mmHg, and basal saturation 95%. Upon arrival, his Glasgow Coma Scale score was 15; however, he progressively became increasingly drowsy. Physical examination revealed right hypochondrial pain and bibasal crackles.
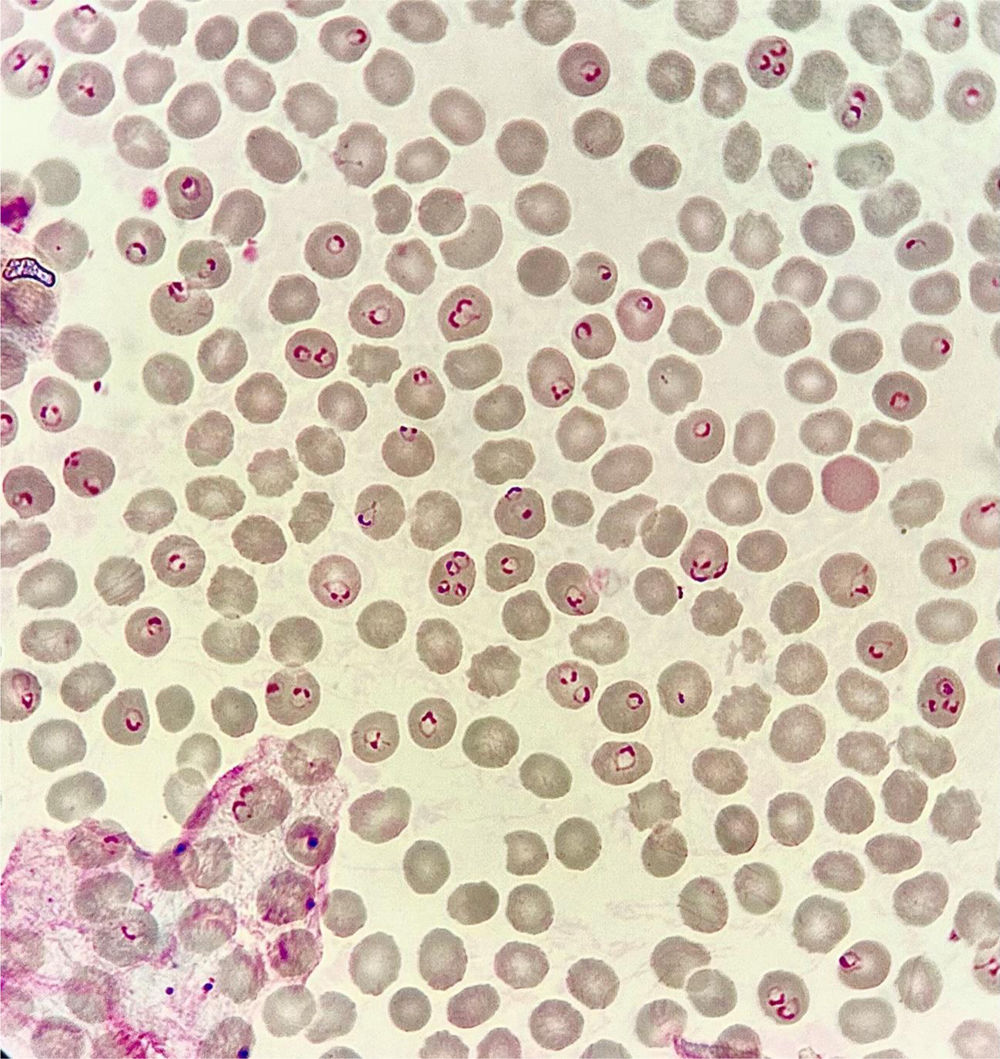
Urgent laboratory tests included normal leukocytes and hemogram, platelets 29,000/μL, total bilirubin 12mg/dL (direct bilirubin 9.9mg/dL), ALT 96UI/L, GGT 224UI/L, LDH 868UI/L, creatinine 2.63mg/dL, glucose 71mg/dL, sodium 129mmol/L, and CRP 20mg/dL. No alterations in coagulopathy. A PCR of arbovirus (dengue, zika and chikungunya) and a study of parasites in peripheral blood was requested (Fig. 1).
What do you consider to be the most likely etiological agent?Multiple parasitism is hcharacteristic of Plasmodium falciparum, showing up to four rings within a single erythrocyte. There are often observed several chromatin dots per trophozoite, corresponding to multinucleate forms. Very intense parasitemia (>10%) involving only trophozoites is suggestive of P. falciparum, even if gametocytes and schizonts are not observed, as these remain sequestered in visceral capillaries.
P. falciparum parasitises erythrocytes at all stages of development without altering their morphology, in contrast to Plasmodium vivax and Plasmodium ovale infections.
P. falciparum is frequently observed at the edge of the erythrocyte membrane; this position is known as apliquée or accolée and is distinctive for this species.
The patient was admitted to the Intensive Care Unit and started therapy with artesunate 210mg (2.4mg/kg for a 87kg patient) at hours 0, 12, and 24 on the first day, followed by daily administration with parasitemia monitoring every 12h (the parasitemia in the first 24h of treatment continued to be reported as >50%) for an additional 5 days, totaling 6 days, following confirmation of parasitemia clearance. Ceftriaxone and supportive treatment were also initiated. After parasitemia became negative, three days of oral artemisinin-combination therapy were administered. During his stay in ICU, serologies for hepatitis, HIV, and syphilis were also conducted, with negative results (he was vaccinated against hepatitis B and had known positive IgG for hepatitis A). After completing the therapy, the patient had a positive outcome with the treatment and was able to be discharged.
FundingNo funding sources were used.
Conflict of interestsAll the authors deny any conflict of interest.