The epidemiology of respiratory syncytial virus (RSV) infection has changed during the COVID-19 pandemic. Our objectives were to describe the RSV epidemic in 2021 and compare it with the previous years to the pandemic.
MethodsRetrospective study performed in Madrid (Spain) in a large pediatric hospital comparing the epidemiology and clinical data of RSV admissions during 2021 and the two previous seasons.
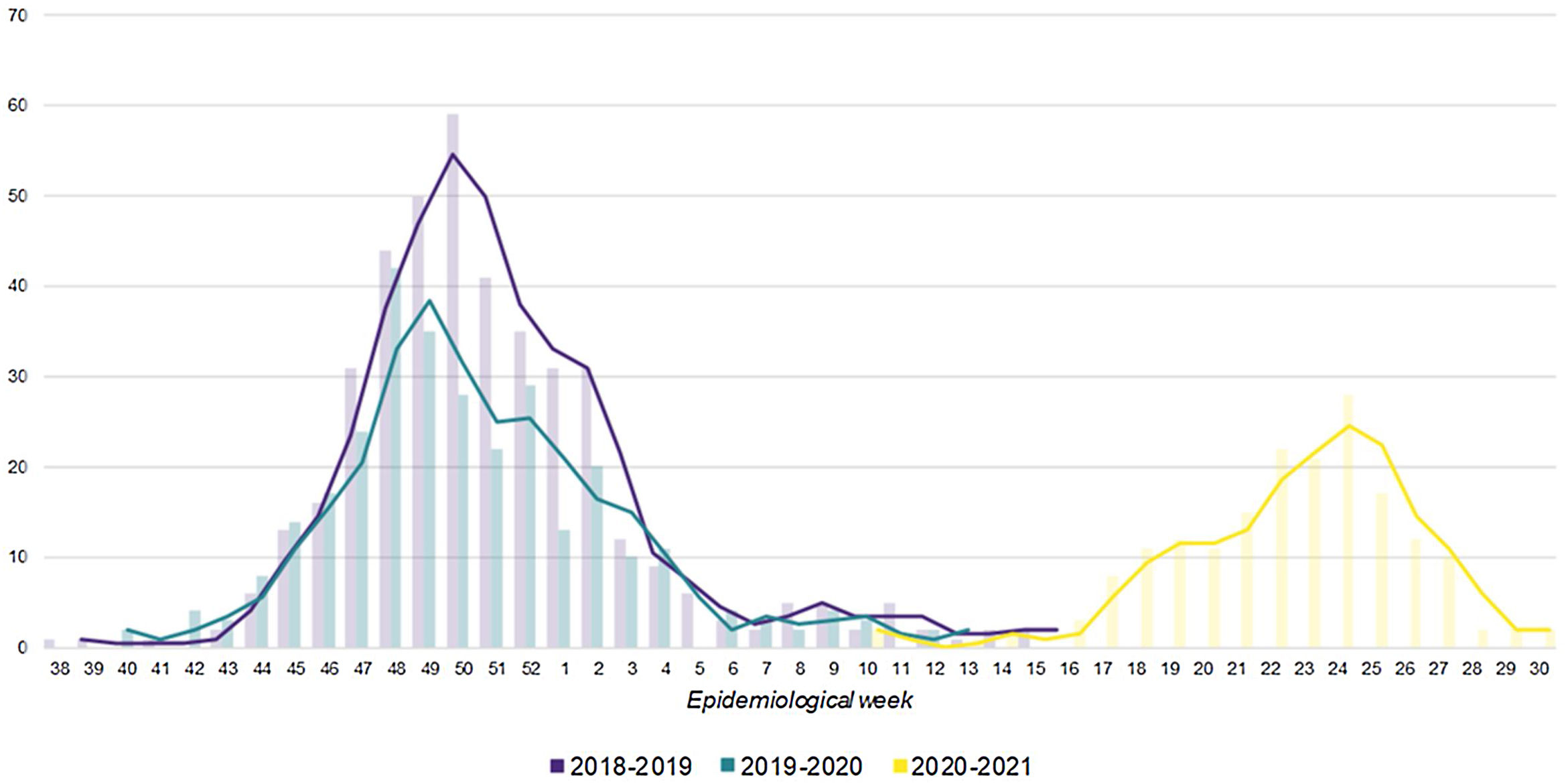
Results899 children were admitted for RSV infection during the study period. During 2021, the outbreak peaked in June and the last cases were identified in July. Previous seasons were detected in autumn-winter. The number of admissions in 2021 was significantly lower than in previous seasons. There were no differences between seasons regarding age, sex or disease severity.
ConclusionRSV hospitalizations during 2021 in Spain moved to summer with no cases in autumn and winter 2020–2021. Unlike other countries, clinical data were similar between epidemics.
La epidemiología de la infección por virus respiratorio sincitial (VRS) ha cambiado durante la pandemia de COVID-19. Nuestros objetivos fueron describir la epidemia de VRS en 2021 y compararla con las de los años previos a la pandemia.
MétodosEstudio retrospectivo realizado en Madrid (España), en un hospital pediátrico terciario, que compara los datos epidemiológicos y clínicos de los ingresos por VRS durante 2021 y las 2 temporadas anteriores.
ResultadosIngresaron 899 niños por infección por VRS en el período de estudio. Durante 2021, el brote alcanzó su punto máximo en junio y los últimos casos se identificaron en julio. En las temporadas anteriores se detectaron en otoño-invierno. El número de hospitalizaciones en 2021 fue significativamente menor que en temporadas anteriores. No hubo diferencias entre temporadas en cuanto a edad, sexo o gravedad de la enfermedad.
ConclusiónLas hospitalizaciones por VRS durante 2021 en España se trasladaron a verano, sin casos en otoño e invierno 2020-2021. A diferencia de otros países, los datos clínicos fueron similares entre epidemias.
Respiratory syncytial virus (RSV) is the most prevalent viral cause of bronchiolitis and lower respiratory tract infection and hospitalization in infants worldwide. Estimates suggest that about 34 million new cases of RSV lower respiratory infection occur globally in children younger than 5 years, with 3.4 million admissions to hospitals (10% admission rate) and about 199000 deaths per year, predominantly in the developing world.1,2
The COVID-19 pandemic has drastically changed the epidemiology of other viral respiratory infections in both children and adults. Worldwide, the autumn and winter RSV epidemics have virtually disappeared,3,4 and in some countries in the Southern hemisphere like South Africa or Australia, the RSV season has moved to spring, marking an unprecedented phenomenon.5 In Spain, as in other European countries, the winter epidemic (November–February) has disappeared and moved to spring-summer.6 Although the increased absenteeism to day care centers and the non-pharmacological measures used to combat the COVID-19 pandemic will have contributed to modify the seasonal pattern, there are other theories about what may be behind these epidemiological changes. In addition, other viruses such as rhinoviruses have remained causative agents of respiratory infections and bronchiolitis.7
RSV has not circulated for more than one year and pregnant women have not acquired natural immunity as a result of prolonged absence of contact, which could mean a change in the severity of the infection in young infants.
The objective of this study is to describe the epidemiological characteristics of the delayed 2021 RSV epidemic in Spain and compare them with those of previous winter seasons in a pediatric tertiary care hospital.
Patients and methodsThis is a retrospective study including all patients under 18 years hospitalized for RSV during two conventional pre-COVID-19 epidemic seasons – 2018–2019 and 2019–2020 – and the 2021 season at the La Paz University Hospital, a tertiary center in Madrid, Spain. We consider the 2021 epidemic to be over by July 31, as the number of incident cases in our center practically disappeared.
In our hospital, rapid test and/or PCR for RSV (Alere i or COBAS Liat, Roche®) is systematically performed in pediatric patients needing admission with compatible symptomatology during the epidemic season. During the 2020–2021 season, the same criteria were followed. When the regional surveillance systems detected the first positive cases in 2020, systematic screening was established in our center. Additionally, in the last season, multiplex PCR (Filmarray®) was performed on children diagnosed with bronchiolitis. The department of Preventive Medicine conducted data collection as a part of their regular activities. Each season they conducted a surveillance of all hospitalized RSV cases. The epidemiological data on age, sex, date of admission, discharge date, need for admission to the pediatric intensive care unit (PICU), and length of stay was obtained from electronic medical records. We considered a nosocomial infection when the diagnosis was made after the third day of hospitalization in a patient with absence of symptoms of RSV infection on admission.
All statistical analyses were performed using R Statistical Software, version 4.1.0 (R Foundation for Statistical Computing, Vienna, Austria). Continuous variables were presented as means and standard deviations (SD) or medians and interquartile ranges (IQR), as appropriate. Categorical variables are expressed in terms of frequency (percentages). Categorical variables were compared using the chi-square and Fisher's exact test, and continuous variables were analyzed with ANOVA or non-parametric tests (Kruskal–Wallis) as appropriate. A two-tailed p-value <0.05 was considered statistically significant.
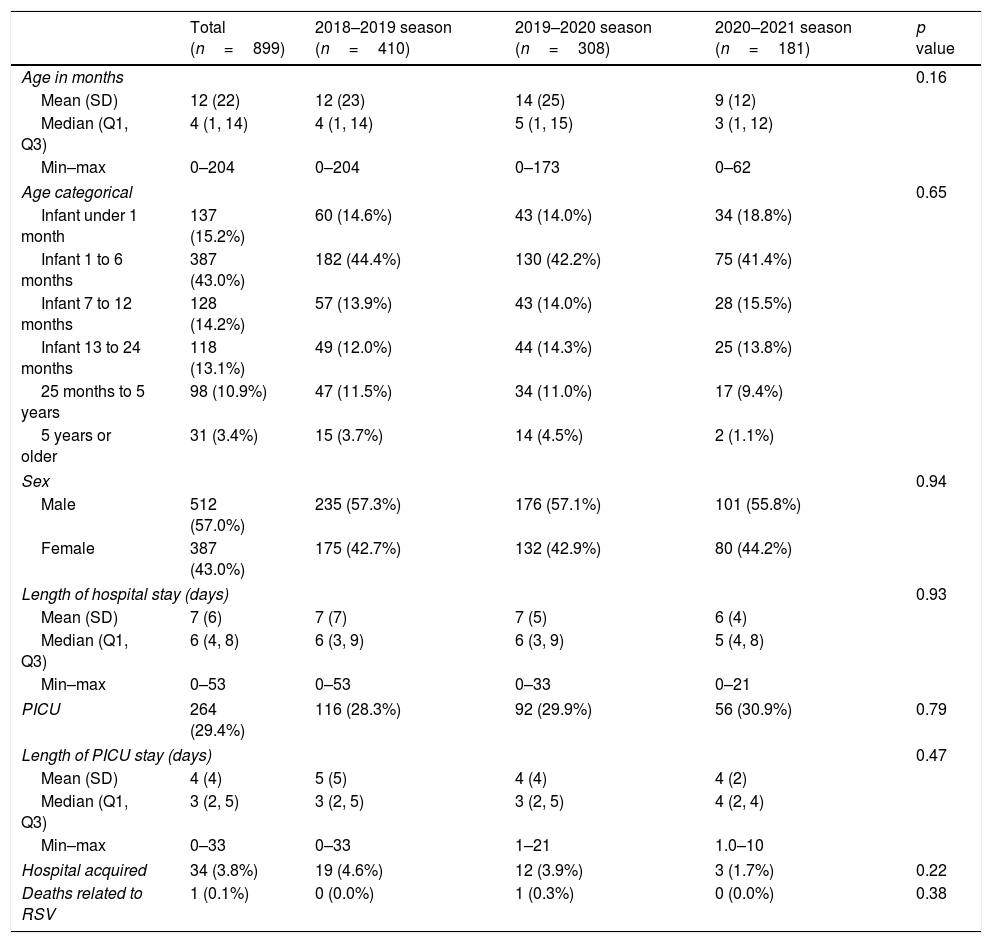
ResultsA total of 899 patients were hospitalized with RSV infection in the Paediatric Infectious Unit of La Paz University Hospital during the studied epidemic seasons. Mean age of all patients was 12.3 months (SD 22.3) and 57% were male.
During the 2021 season we registered 181 hospitalizations. 55.8% of the patients were male and mean age was 9 months (SD 12.4). Median length of hospital stay was 5 days (IQR 4–8). PICU admission rate was 30.9%, with median length of stay in PICU of 3 days (IQR 2–5). Median age of patients admitted to PICU was 1 month (IQR 0-3), while those who did not required PICU admission were older, with median age 7 months (IQR 1–16; p-value <0.001). Three cases were hospital-acquired (1.7%), which were diagnosed more than 5 days after admission and had no symptoms on admission. Patients’ characteristics had a similar distribution in the three studied seasons, no significant differences were observed between them (Table 1).
Patients’ characteristics and outcomes.
| Total (n=899) | 2018–2019 season (n=410) | 2019–2020 season (n=308) | 2020–2021 season (n=181) | p value | |
|---|---|---|---|---|---|
| Age in months | 0.16 | ||||
| Mean (SD) | 12 (22) | 12 (23) | 14 (25) | 9 (12) | |
| Median (Q1, Q3) | 4 (1, 14) | 4 (1, 14) | 5 (1, 15) | 3 (1, 12) | |
| Min–max | 0–204 | 0–204 | 0–173 | 0–62 | |
| Age categorical | 0.65 | ||||
| Infant under 1 month | 137 (15.2%) | 60 (14.6%) | 43 (14.0%) | 34 (18.8%) | |
| Infant 1 to 6 months | 387 (43.0%) | 182 (44.4%) | 130 (42.2%) | 75 (41.4%) | |
| Infant 7 to 12 months | 128 (14.2%) | 57 (13.9%) | 43 (14.0%) | 28 (15.5%) | |
| Infant 13 to 24 months | 118 (13.1%) | 49 (12.0%) | 44 (14.3%) | 25 (13.8%) | |
| 25 months to 5 years | 98 (10.9%) | 47 (11.5%) | 34 (11.0%) | 17 (9.4%) | |
| 5 years or older | 31 (3.4%) | 15 (3.7%) | 14 (4.5%) | 2 (1.1%) | |
| Sex | 0.94 | ||||
| Male | 512 (57.0%) | 235 (57.3%) | 176 (57.1%) | 101 (55.8%) | |
| Female | 387 (43.0%) | 175 (42.7%) | 132 (42.9%) | 80 (44.2%) | |
| Length of hospital stay (days) | 0.93 | ||||
| Mean (SD) | 7 (6) | 7 (7) | 7 (5) | 6 (4) | |
| Median (Q1, Q3) | 6 (4, 8) | 6 (3, 9) | 6 (3, 9) | 5 (4, 8) | |
| Min–max | 0–53 | 0–53 | 0–33 | 0–21 | |
| PICU | 264 (29.4%) | 116 (28.3%) | 92 (29.9%) | 56 (30.9%) | 0.79 |
| Length of PICU stay (days) | 0.47 | ||||
| Mean (SD) | 4 (4) | 5 (5) | 4 (4) | 4 (2) | |
| Median (Q1, Q3) | 3 (2, 5) | 3 (2, 5) | 3 (2, 5) | 4 (2, 4) | |
| Min–max | 0–33 | 0–33 | 1–21 | 1.0–10 | |
| Hospital acquired | 34 (3.8%) | 19 (4.6%) | 12 (3.9%) | 3 (1.7%) | 0.22 |
| Deaths related to RSV | 1 (0.1%) | 0 (0.0%) | 1 (0.3%) | 0 (0.0%) | 0.38 |
Fig. 1 shows the epidemic curves for the three seasons. In 2021, RSV cases started to appear in week 10, with a large increase in cases from week 17. The peak was reached in week 24 with 28 admissions and the last cases were identified in week 30. The total number of admissions in 2021 was significantly lower than in previous seasons.
In previous seasons (2018–2019 and 2019–2020), cases were detected from weeks 38–41 to weeks 12–15. The 2018–2019 season peaked in week 50 with 59 cases, while the 2019–2020 season peaked in week 48 with 42 cases. These seasons were defined by the annual RSV surveillance that is established in our center, simultaneously with the influenza surveillance from week 40 to week 20 of the following year.
During the 2020–2021 season, 19 cases of rhinovirus infection were detected in children diagnosed with bronchiolitis, one of them in coinfection with RSV and adenovirus and other in coinfection with SARS-CoV-2. Rhinovirus circulated throughout the entire period without being able to highlight a peak at any time. No other respiratory viruses were identified, except for four other cases of SARS-CoV-2 bronchiolitis.
DiscussionOur study showed changes in the epidemiology of RSV hospitalizations during 2021 in Spain, with an onset of cases in spring and no cases in autumn and winter 2020–2021. In addition, the weekly number of admissions registered during 2021 epidemic was lower than previous years, although the clinical characteristics of the patients were similar.
This temporal shift was reported in other studies, although their incidence was higher and even exceeded that of preceding years.8,9 A study from Australia also found an increase in patients’ median age9 and other work from the United States reported a more severe course of the infection.10 In contrast, we did not find differences with previous epidemic seasons regarding age, sex or disease severity.
Some authors relate the changes in RSV epidemic with COVID-19 control measures (mask wearing, handwashing and isolation) and the closing of schools.10–12 However, it might not be the only explanation, especially considering that in Madrid nurseries and schools have been opened for the whole academic year and mask wearing is not mandatory in children under 6 years.4
Viral interference can alter the pattern and dynamics of infection. As proposed in studies conducted prior to the COVID-19 pandemic, rhinovirus could compete with other respiratory viruses and change the epidemic dynamics. A study suggested that it had a role in the delaying of the 2009 Influenza A pandemic in France.13 During 2021, rhinoviruses have been circulating and causing respiratory infection in children despite the hygienic measures to control SARS-CoV-2 transmission.3 In addition, there are studies that suggest that there may be interference between RSV and rhinovirus infection in children.14 Other possible hypothesis proposed to explain this phenomenon is that when there is reduced transmission in adults and older children due to non-pharmacological measures, diseases like bronchiolitis do not become real epidemics.15
A potential bias of our study is that we only included hospitalized patients. Therefore, we lack information related to mild cases that are more likely handled in primary health care. Because of this, our results cannot be widely generalized. Nevertheless, the fact that our study was conducted in a tertiary hospital including data on all RSV infection hospitalizations during three epidemic seasons, collected as part of surveillance activities existing prior to the COVID-19 pandemic allows for a big sample size which, despite the limitations, we believe is representative of the RSV hospitalized Madrid population.
As other various infectious diseases, RSV has been impacted by the COVID-19 pandemic. Our data confirms the change in seasonality reported in other studies around the world and remarks the importance of surveillance systems in order to study disease dynamics and plan ahead the potential implications for medical services. Viral interference, COVID-19 control measures and individual behavioral changes due to the pandemic are among the factors that could have caused the delayed onset of the epidemic and the low number of cases observed.
FundingThis work is not funded.
Conflict of interestThe authors declare no conflict of interest.