Osteomyelitis and septic arthritis can cause significant morbidity in children. Most of these infections occur due to hematogenous dissemination of microorganisms. A small proportion occurs after a trauma and differs from hematogenous cases in their clinical presentation and microbial etiology, as a consequence of a direct inoculation.1Staphylococcus aureus, Enterobacter cloacae, Acinetobacter spp. and Pseudomonasaeruginosa are the most reported posttraumatic arthritis pathogens in the literature.1–3 We report a posttraumatic arthritis caused by infrequent microorganisms.
A 13-year-old male arrived at the emergency department suffering from pain and right knee swelling. He fell down over a rocky terrain in a rural area two days before, causing a wound in his right knee.
Right knee examination showed warmth around the wound and loss of the range of motion. Radiographic findings were normal. The blood count showed a normal leukocyte count (WBC) but a high C-reactive protein (CRP) of 104.8mg/l (normal range, <1.0mg/l) and an erythrocyte sedimentation rate of 68mm/h (<15.0mm/h). The suspected diagnosis was post-traumatic septic arthritis. The patient was empirically treated with cefazolin (2g/12h).
A right knee arthrocentesis was performed. The fluid analysis showed 40,500cells/mm3 with 82% neutrophils, 39.9mg protein/dl and presence of Gram variable bacilli in the specimen's Gram stain. The same day, an arthroscopic debridement and irrigation was carried out.
Part of the fluid was inoculated onto chocolate and 5% sheep blood agars (bioMérieux, France). The plates were incubated at 37°C with 5% CO2. In 24h, it grew up green, pale colonies. Additionally, in the following 48h, it grew up mucoid colonies that became shade of salmon pink 5 days later.
The matrix-assisted laser desorption ionization-Time of flight mass spectrometry (MALDI-TOF MS) (Bruker Corporation, USA) identified the isolates as Paenibacillus barcinonensis and Rhodococcus equi (both log score values: 1.9). Identification was supported by Gram stain, colony characteristics and biochemical tests (CAMP-test). Antibiotic treatment was changed to vancomycin (950mg/6h).
P. barcinonensis showed susceptibility to vancomycin, sulfamethoxazole-trimethoprim and fluoroquinolones (CLSI criteria).4R. equi showed susceptibility to vancomycin, erythromycin and fluoroquinolones (no-approved standards criteria).5 The treatment was switched to levofloxacin (500mg/12h) after a week of vancomycin.
The boy was discharged after 22 days in hospital with a full mobility recovery.
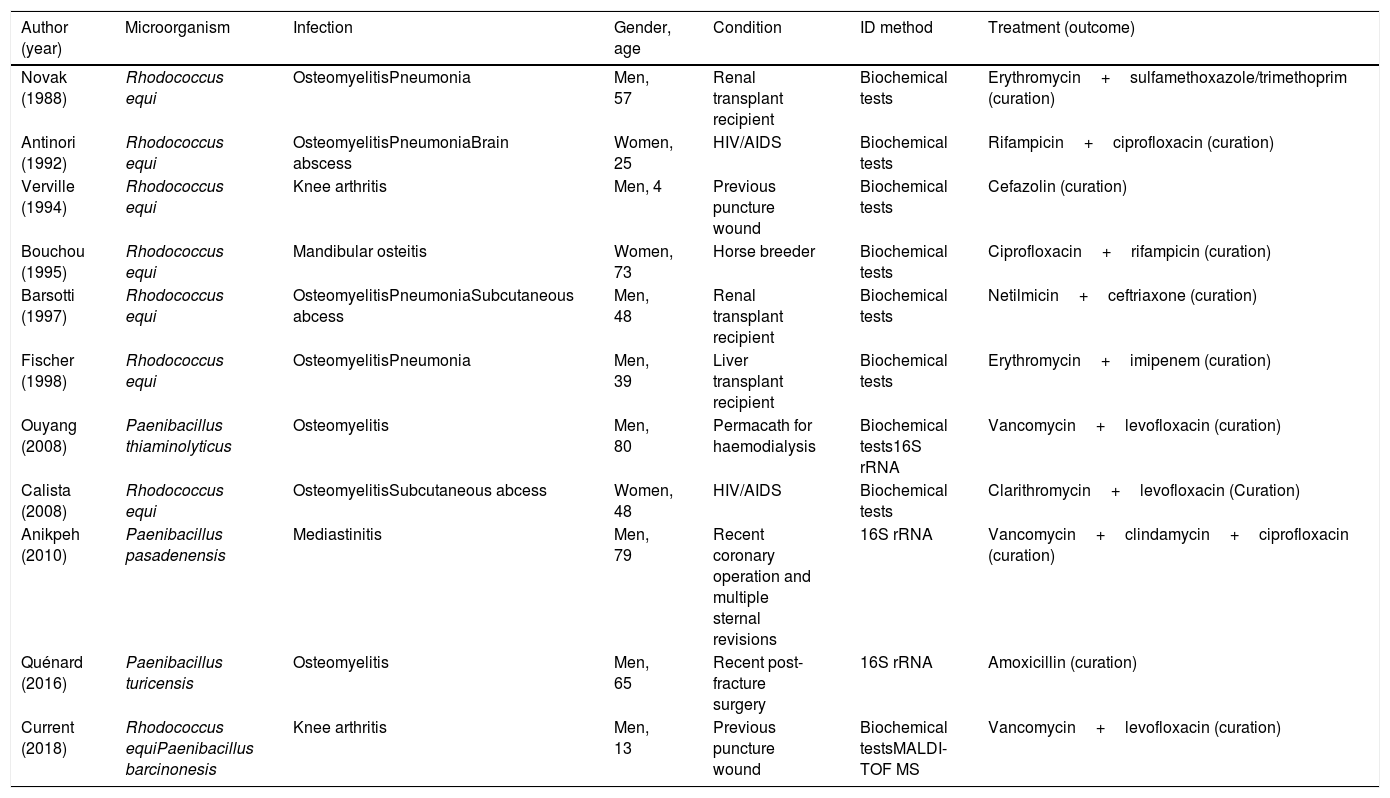
P. barcinonensis is a Gram-variable microorganism. This species takes its name from Barcelona, a city of Spain where it was first isolated.6 It is a saprophytic inhabitant of a large variety of sources (soil, water, etc.).7 In general, is considered a contaminant. Only three bone infection cases have been described by species of the genre Paenibacillus spp. (Table 1). As we can observe, skin and tissue disruption were underlying in these three bone infection cases. Telluric microorganisms, like Paenibacillus spp., are opportunistic pathogens that can cause infections when our natural barriers are broken.7Paenibacillus spp. is resistant to ampicillin and susceptible to fluoroquinolones, gentamicin and vancomycin.7,8
Reported bone infections cases by Paenibacillus spp. and Rhodococcusequi.6–8,10
| Author (year) | Microorganism | Infection | Gender, age | Condition | ID method | Treatment (outcome) |
|---|---|---|---|---|---|---|
| Novak (1988) | Rhodococcus equi | OsteomyelitisPneumonia | Men, 57 | Renal transplant recipient | Biochemical tests | Erythromycin+sulfamethoxazole/trimethoprim (curation) |
| Antinori (1992) | Rhodococcus equi | OsteomyelitisPneumoniaBrain abscess | Women, 25 | HIV/AIDS | Biochemical tests | Rifampicin+ciprofloxacin (curation) |
| Verville (1994) | Rhodococcus equi | Knee arthritis | Men, 4 | Previous puncture wound | Biochemical tests | Cefazolin (curation) |
| Bouchou (1995) | Rhodococcus equi | Mandibular osteitis | Women, 73 | Horse breeder | Biochemical tests | Ciprofloxacin+rifampicin (curation) |
| Barsotti (1997) | Rhodococcus equi | OsteomyelitisPneumoniaSubcutaneous abcess | Men, 48 | Renal transplant recipient | Biochemical tests | Netilmicin+ceftriaxone (curation) |
| Fischer (1998) | Rhodococcus equi | OsteomyelitisPneumonia | Men, 39 | Liver transplant recipient | Biochemical tests | Erythromycin+imipenem (curation) |
| Ouyang (2008) | Paenibacillus thiaminolyticus | Osteomyelitis | Men, 80 | Permacath for haemodialysis | Biochemical tests16S rRNA | Vancomycin+levofloxacin (curation) |
| Calista (2008) | Rhodococcus equi | OsteomyelitisSubcutaneous abcess | Women, 48 | HIV/AIDS | Biochemical tests | Clarithromycin+levofloxacin (Curation) |
| Anikpeh (2010) | Paenibacillus pasadenensis | Mediastinitis | Men, 79 | Recent coronary operation and multiple sternal revisions | 16S rRNA | Vancomycin+clindamycin+ciprofloxacin (curation) |
| Quénard (2016) | Paenibacillus turicensis | Osteomyelitis | Men, 65 | Recent post-fracture surgery | 16S rRNA | Amoxicillin (curation) |
| Current (2018) | Rhodococcus equiPaenibacillus barcinonesis | Knee arthritis | Men, 13 | Previous puncture wound | Biochemical testsMALDI-TOF MS | Vancomycin+levofloxacin (curation) |
The second agent was R. equi. Its name derives from a pigment that grants a salmon-pink shade. R. equi is a Gram-positive coccobacillus and a well-known pathogen in veterinary medicine. It is microorganism widespread in the environment also. Its transmission is due to inhalation and usually causes a subacute pulmonary disease.9 The infection in immunocompetent people is uncommon.10 The highest prevalence of disease coincided with the HIV epidemic. Nowadays, thanks to the introduction of HAART, the incidence has changed substantially.9 To our knowledge, only few bone infections cases by R. equi have been reported in the literature, frequently in immunocompromised patients (Table 1). R. equi is susceptible to vancomycin, macrolides, aminoglycosides, fluoroquinolones and carbapenems.5,9
In summary, both microorganisms are environmental and sometimes they are considered contaminant. However, we should know that in non-hematogenous osteoarticular infection, there is a larger variety of microorganisms than in the hematogenous one. This microbiology diversity highlights the importance of performing a detailed anamnesis, microbiologic diagnosis and adequate treatment. This case report emphasizes the importance of having a robust and rapid tool for routine identification. The correct antimicrobial treatment of the patient can be initiated early if the laboratory is provided of fast and accurate methods for microbiology identification, such as MALDI-TOF MS.
Funding informationThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations of interestNone.
We would like to thank Dr. Juan Carlos Martínez-Pastor (from the Department of Orthopedic Surgery and Traumatology, Hospital Clínic, Barcelona, Spain) and Dr. Marta Azuara-Robles (from the Department of Pediatrics, Hospital Universitari Germans Trias i Pujol, Badalona, Spain) for their reviews, suggestions and professional support.