Antibiotic resistance has been recognized as a worldwide problem. Our aim was to assess the perceptions of Spanish residents about antibiotic use and resistance.
MethodsAn online cross-sectional survey was conducted on all resident doctors in five teaching hospitals (September to November 2010). A link to the questionnaire was e-mailed to 844 doctors. The questionnaire collected demographical characteristics, residents’ knowledge about microorganisms of known clinical relevance, their habits in the antibiotic prescription process, and their perceptions on the activities aimed to improve antibiotic use.
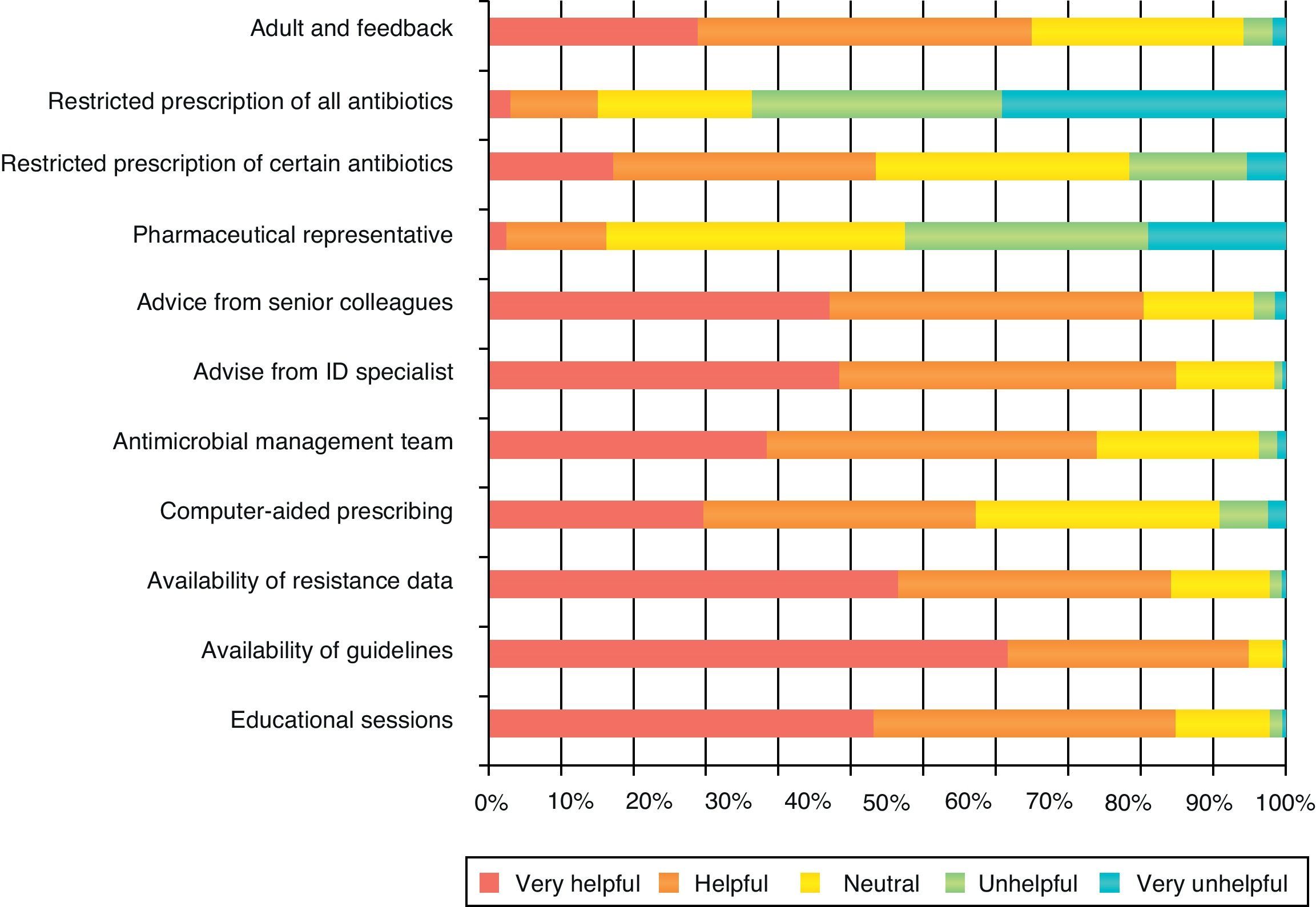
ResultsWe received 279 responses corresponding to 33.05% of all targeted residents. The response rate was higher among junior than among senior residents (39.95% vs. 26.12%; p<0.05). Residents of all hospitals, specialties and seniority mostly considered that antimicrobial resistance was a significant problem at national level (94.3%), at their institution (91.3%), and for their daily practice (83.8%). Residents considered their training regarding antibiotics insufficient, although up to 86.5% had prescribed antibiotics in the last month. They preferred the availability of local antibiotic guidelines (65%), specific teaching sessions, specific antimicrobial management teams or readily accessible advice from a group or an infectious diseases specialist, to improve antibiotic prescribing, rather than other restrictive interventions.
ConclusionsMost residents at the hospitals surveyed believed that antibiotic resistance was a serious problem. The results of this survey provided very important information to optimize adherence to Antimicrobial Stewardship Programs (ASPs). Educational strategies and non-restrictive aids are the most valuable interventions, which ASPs should capitalize on to improve antimicrobial prescription.
La resistencia a los antibióticos ha sido reconocida como un problema a nivel mundial. Nuestro objetivo fue conocer las percepciones de los médicos residentes españoles, respecto al uso de antibióticos y la resistencia a los mismos.
MétodosEstudio descriptivo transversal mediante encuesta on-line, a todos los médicos residentes de 5 hospitales terciarios, realizada entre septiembre y noviembre de 2010. Se envió un enlace a la encuesta a través de correo electrónico a 844 médicos residentes. El cuestionario evalúa las características demográficas, el conocimiento de los residentes sobre algunos microorganismos de relevancia clínica conocida, sus hábitos en el proceso de prescripción de antibióticos y sus percepciones sobre las actividades encaminadas a mejorar el uso de antimicrobianos.
ResultadosSe recibieron 279 respuestas que corresponden al 33,05% de todos los residentes encuestados. La tasa de respuesta fue mayor entre los residentes de los primeros años que entre los residentes de los últimos años (39,95% vs 26,12%, p<0,05). Los residentes de todos los hospitales, especialidades y grado de experiencia, en su mayoría consideran que la resistencia antimicrobiana es un problema importante a nivel nacional (94,3%), en su institución (91,3%) y para su práctica diaria (83,8%). Los residentes consideran su formación respecto a los antibióticos insuficiente, aunque, hasta el 86,5% había recetado antibióticos en el último mes. Preferían la disponibilidad de guías locales de uso de antibióticos (65%), sesiones de enseñanza específicas, equipos de gestión de antimicrobianos o mayor facilidad de acceso a la asesoría de un adjunto o de un especialista en enfermedades infecciosas, para mejorar la prescripción de antibióticos, en lugar de otras intervenciones restrictivas.
ConclusionesLa mayoría de los residentes de los hospitales encuestados consideran la resistencia a antibióticos como un problema grave. Los resultados de este estudio proporcionan información muy importante para optimizar la adherencia a los programas de optimización de uso de antimicrobianos (PROA). Estrategias de tipo educativo y las ayudas no restrictivas a la prescripción son las intervenciones más valoradas por los médicos residentes en España, sobre las que los programas PROA deben incidir en aras de mejorar la prescripción de antimicrobianos.
Antibiotic resistance has been recognized as a worldwide problem, in part related to inappropriate antibiotic prescribing.1 One of the proposed solutions to this problem has been the implementation of ASPs. ASPs use a systematic approach to optimize antimicrobial therapy through a variety of interventions and have been proven to be cost-effective.2 In order to improve the prescription of antimicrobials, ASPs should promote changes in prescribing habits of professionals involved in their use.3 These habits are influenced by many factors but among those are the knowledge and perceptions about antimicrobials and resistance. Resident physicians as specialists in training are a very important target for interventions aiming to improve antimicrobial prescribing. Previous surveys have been conducted to assess physicians’ knowledge, attitudes and beliefs about antimicrobial use and resistance in USA, Brazil, France and Scotland.3–9 These results are not necessarily applicable to other settings, and studies comparing the knowledge and attitudes toward antimicrobial use of residents in different years of their training programs have not been performed previously. We surveyed resident doctors from five public teaching hospitals from Spain to assess their knowledge, attitudes and perceptions concerning antibiotic use and resistance. Our goal was to gain some understanding of this process in order to detect areas for further improvement and intervention.
Participants and methodsWe conducted an online cross-sectional survey of all eligible residents in five large tertiary teaching hospitals belonging to the Spanish National Health Service, which were located in 4 different cities (Madrid, Seville, Murcia and Barakaldo). The term “resident” referred to doctors after qualification from medical school who were still in their training years for a specialty. Both junior (post-graduate year-1 [PGY-1]) and senior (PGY-4 and PGY-5) residents of the participating medical centers were targeted. The survey was Internet-based using the platform http://www.surveymonkey.com and was voluntary and anonymous. The survey remained open for 8 weeks between September 20 and November 20, 2010. No incentives for participation were given. An electronic invitation letter including a link to the survey was sent to 844 residents in various specialties (Allergy, Clinical Analysis, Pathology, Pharmacy, Clinical Biochemistry, Internal Medicine, Family and Community Medicine, Oncology, Neurology, Pneumology, Cardiology, Gastroenterology, Nephrology, Hematology, Endocrinology, Dermatology, General Surgery, Maxillofacial Surgery, Cardiovascular Surgery, Vascular Surgery, Plastic Surgery, Pediatric Surgery, Cardiac Surgery, Geriatrics, Pharmacology, Thoracic Surgery, Neurosurgery, Orthopedic Surgery, Anesthesia, Intensive Care, Preventive medicine, ENT, Ophthalmology, Obstetrics and Gynecology, Immunology, Microbiology, Neurophysiology, Pediatrics, Psychiatry, Radiology, Rheumatology, Urology, Nuclear medicine, Rehabilitation and Occupational Health), at all participants hospitals. During the period the survey remained open, residents received 3 reminders (email) to try to get the maximum number of participants.
We adapted the questionnaire designed by Pulcini et al.6 and designed a 46-item questionnaire, after searching the literature for similar studies (supplementary data online).3–7 The questionnaire collected information on training doctors’ demographic data (number of years since medical school graduation, the resident's year of postgraduate training and whether the respondent was a foreign medical graduate and medical specialty). We collected data about the frequency with which they prescribed antibiotics and past training in antibiotic prescribing. For attitudes about antibiotic prescribing we used a 5-point Likert-style scale with response options from very unhelpful/unimportant/unconfident to very helpful/important/confident. To assess residents’ knowledge of the prevalence of antibiotic resistance there were 5 multiple-choice questions to estimate the prevalence of resistance in their hospital for two specific bacterium–antibiotic combinations relevant to clinical practice: Escherichia coli resistance to quinolones and Staphylococcus aureus resistance to methicillin.8 Choices were presented as intervals. Correct intervals ranged at least ±10% of the actual prevalence of resistance at each center.
Percentages were calculated for the categorical data. Univariate analysis used the chi-square test for the categorical data or Fisher's exact test when needed. We analyzed all data using SPSS software, version 15 (SPSS Inc., Chicago, IL, USA). All reported p-values were two-tailed and p-value <0.05 was considered to be significant.
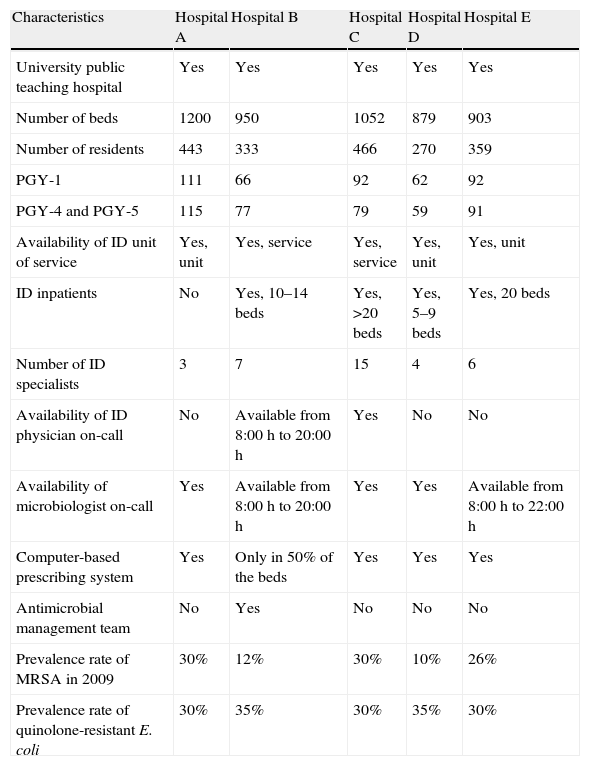
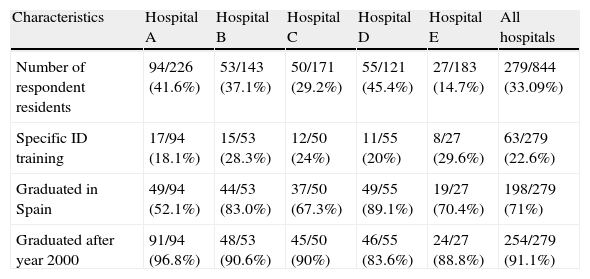
ResultsThe characteristics of the participating hospitals are described in Table 1, and characteristics of respondent residents are shown in Table 2. Of the 844 targeted residents to whom the survey was sent, 279 (33.05%) completed it. Response rate was higher among junior (39.95%) than among senior residents (26.12%) (p<0.0005). Of the 279 respondents, 157 (56.3%) belonged to medical specialties as shown in Table 2.
Hospitals characteristics and antibiotic policy.
| Characteristics | Hospital A | Hospital B | Hospital C | Hospital D | Hospital E |
| University public teaching hospital | Yes | Yes | Yes | Yes | Yes |
| Number of beds | 1200 | 950 | 1052 | 879 | 903 |
| Number of residents | 443 | 333 | 466 | 270 | 359 |
| PGY-1 | 111 | 66 | 92 | 62 | 92 |
| PGY-4 and PGY-5 | 115 | 77 | 79 | 59 | 91 |
| Availability of ID unit of service | Yes, unit | Yes, service | Yes, service | Yes, unit | Yes, unit |
| ID inpatients | No | Yes, 10–14 beds | Yes, >20 beds | Yes, 5–9 beds | Yes, 20 beds |
| Number of ID specialists | 3 | 7 | 15 | 4 | 6 |
| Availability of ID physician on-call | No | Available from 8:00h to 20:00h | Yes | No | No |
| Availability of microbiologist on-call | Yes | Available from 8:00h to 20:00h | Yes | Yes | Available from 8:00 h to 22:00 h |
| Computer-based prescribing system | Yes | Only in 50% of the beds | Yes | Yes | Yes |
| Antimicrobial management team | No | Yes | No | No | No |
| Prevalence rate of MRSA in 2009 | 30% | 12% | 30% | 10% | 26% |
| Prevalence rate of quinolone-resistant E. coli | 30% | 35% | 30% | 35% | 30% |
ID: infectious diseases; MRSA: methicillin resistant S. aureus; PGY-1: junior resident; PGY 4–5: senior residents.
Characteristics of respondent residents.
| Characteristics | Hospital A | Hospital B | Hospital C | Hospital D | Hospital E | All hospitals |
| Number of respondent residents | 94/226 (41.6%) | 53/143 (37.1%) | 50/171 (29.2%) | 55/121 (45.4%) | 27/183 (14.7%) | 279/844 (33.09%) |
| Specific ID training | 17/94 (18.1%) | 15/53 (28.3%) | 12/50 (24%) | 11/55 (20%) | 8/27 (29.6%) | 63/279 (22.6%) |
| Graduated in Spain | 49/94 (52.1%) | 44/53 (83.0%) | 37/50 (67.3%) | 49/55 (89.1%) | 19/27 (70.4%) | 198/279 (71%) |
| Graduated after year 2000 | 91/94 (96.8%) | 48/53 (90.6%) | 45/50 (90%) | 46/55 (83.6%) | 24/27 (88.8%) | 254/279 (91.1%) |
| Hospital A | Hospital B | Hospital C | Hospital D | Hospital E | All hospitals | |||||||||||||||||||
| Specialty | M | S | C | N | M | S | C | N | M | S | C | N | M | S | C | N | M | S | C | N | M | S | C | N |
| PGY-1 | 43 | 5 | 8 | 7 | 18 | 7 | 1 | 4 | 19 | 7 | 1 | 4 | 11 | 5 | 5 | 10 | 14 | 2 | 3 | 0 | 105 | 26 | 18 | 25 |
| PGY-4 and PGY-5 | 15 | 13 | 1 | 2 | 6 | 9 | 4 | 4 | 15 | 2 | 1 | 1 | 13 | 2 | 5 | 4 | 3 | 0 | 1 | 4 | 52 | 26 | 12 | 15 |
ID: infectious diseases; M: medical specialty; S: surgical specialty; C: critical care/anesthesiology; N: others specialties; PGY-1: junior resident; PGY 4–5: senior residents.
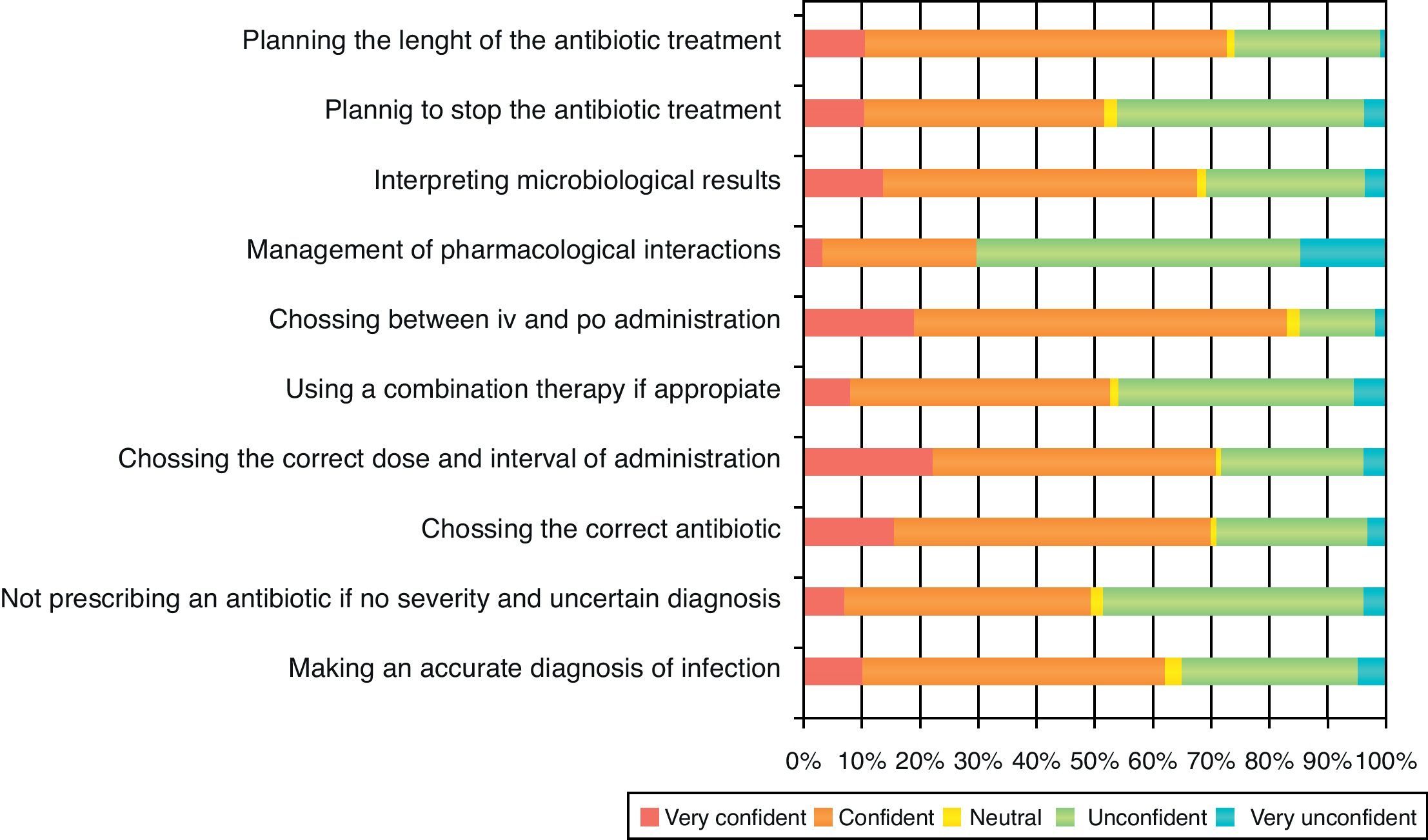
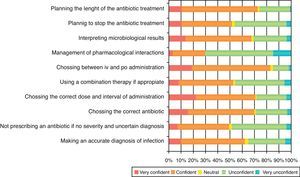
Most (71%) of respondents were graduated in Spanish medical schools, and 91.1% (254 residents) were graduated after 2000. Of the 279 respondents, 63 (22.6%) of them had received specific training (rotation) on infectious diseases during their residency. Most of the respondents 183/259 (70.3%), considered their education in infectious diseases had been insufficient or very insufficient. In contrast, 230 (82.5%) had prescribed antibiotics in the previous month and almost two-thirds (64.6%) of them had prescribed two or more antibiotics in the previous week. Decisions about antimicrobial therapy were taken in 43.2% of cases by the residents themselves and by a faculty staff member in 36.9%. Residents from surgical specialties prescribed antibiotics by themselves in 61.9% of the cases; those one belonging to medical specialties in 43.8% and critical care residents only in 34.5% of the cases. Seventeen percent (17.7%) of PGY-1 prescribed antibiotics by themselves in contrast with 87.7% of senior residents (PGY-4 and PGY-5) (p<0.05). Residents seemed to feel relatively confident prescribing antibiotics, choosing the dose, interval and route of administration (Fig. 1). Most respondents (94.3%) perceived antibiotic resistance as a national problem, and 83.8% believed that it was a problem in their clinical practice. The perception that resistance was a problem in clinical practice was not influenced by postgraduate year of experience (82.4% RY-1 vs. 82.7% RY-4 and 5) (p=0.97).
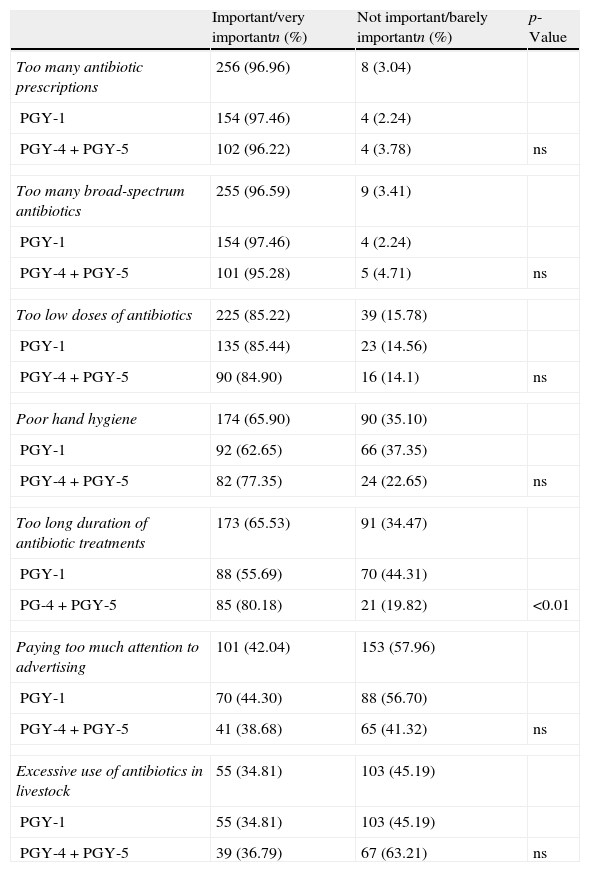
There are three factors that were perceived as the most relevant causes of antimicrobial resistance: antimicrobial overprescription, excessive use of broad spectrum antibiotics and the use of sub-therapeutic doses (Table 3). Paying too much attention to pharmaceutical advertising and excessive use of antibiotics in livestock were found to be the less relevant factors associated to antimicrobial resistance. When evaluating differences between junior and senior residents, the latter were more concerned about the length of antibiotic treatments as an important factor fueling antimicrobial resistance (Table 3).
Differences between junior and senior resident's perception of the importance of several factors linked to antibiotic resistance.
| Important/very importantn (%) | Not important/barely importantn (%) | p-Value | |
| Too many antibiotic prescriptions | 256 (96.96) | 8 (3.04) | |
| PGY-1 | 154 (97.46) | 4 (2.24) | |
| PGY-4+PGY-5 | 102 (96.22) | 4 (3.78) | ns |
| Too many broad-spectrum antibiotics | 255 (96.59) | 9 (3.41) | |
| PGY-1 | 154 (97.46) | 4 (2.24) | |
| PGY-4+PGY-5 | 101 (95.28) | 5 (4.71) | ns |
| Too low doses of antibiotics | 225 (85.22) | 39 (15.78) | |
| PGY-1 | 135 (85.44) | 23 (14.56) | |
| PGY-4+PGY-5 | 90 (84.90) | 16 (14.1) | ns |
| Poor hand hygiene | 174 (65.90) | 90 (35.10) | |
| PGY-1 | 92 (62.65) | 66 (37.35) | |
| PGY-4+PGY-5 | 82 (77.35) | 24 (22.65) | ns |
| Too long duration of antibiotic treatments | 173 (65.53) | 91 (34.47) | |
| PGY-1 | 88 (55.69) | 70 (44.31) | |
| PG-4+PGY-5 | 85 (80.18) | 21 (19.82) | <0.01 |
| Paying too much attention to advertising | 101 (42.04) | 153 (57.96) | |
| PGY-1 | 70 (44.30) | 88 (56.70) | |
| PGY-4+PGY-5 | 41 (38.68) | 65 (41.32) | ns |
| Excessive use of antibiotics in livestock | 55 (34.81) | 103 (45.19) | |
| PGY-1 | 55 (34.81) | 103 (45.19) | |
| PGY-4+PGY-5 | 39 (36.79) | 67 (63.21) | ns |
PGY-1, fist year residents; PGY-4 and PGY-5, fourth and fifth year residents.
Prevalence of quinolone-resistant E. coli (QREC) in surveyed centers was between 30% and 35%. Of the respondents, 42.38% correctly identified the rate of QREC at their institutions (25.3% did not answer). The proportion of residents that correctly identified the rate of methicillin resistant S. aureus (MRSA), which is between 10% and 40% of all S. aureus isolates, was 20.2% (49.8% did not answer). No differences in the knowledge of the actual prevalence of QREC were found when specialty or seniority was considered (40.9% among PGY-1 vs. 40.6% among PGY-4 and PGY-5; p=0.63). Nevertheless, senior residents knew better the prevalence of MRSA in their centers (15.7% among PGY-1 vs., 26.4% among PGY-4 and PGY-5; p=0.02, n=265).
The percentage of residents giving the right answer for the prevalence of antibiotic misuse in European hospitals was 20.5%, with 63.6% of them underestimating the real prevalence (this prevalence in Europe ranges between 21% and 50%12–14). There were no significant differences among the five participating hospitals, and knowledge of this prevalence rate was not related to the degree of experience of the resident (23.4% of correct answers among PGY-1 participants vs. 29.2% among PGY4-5 participants; p=0.54, n=264).
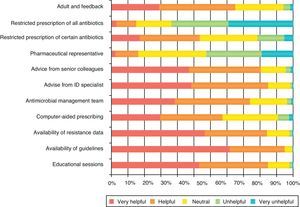
The most favored interventions to improve antibiotic prescribing according to surveyed residents were those providing information without restrictions (Fig. 2), such as availability of local guidelines, availability of resistance data, educational sessions or advice from an Infectious Diseases specialist. Pharmaceutical representatives activities and restriction of antibiotics use were perceived as unhelpful measures (Fig. 2).
DiscussionOur survey shows that residents in Spain are aware and concerned about antibiotic resistance. Ninety-five percent of them think that antibiotic resistance is a national problem, whereas 83% believed that resistance was a problem in their clinical practice. This trend was observed in all hospitals, suggesting that to some extent, residents perceive the risk to be more theoretical than concrete. These findings are consistent with those of Pulcini et al.6 and other surveys previously published.3,5,6,10
Attitudes regarding antibiotic prescribing process varied according to the scenario studied but in general resident doctors felt surprisingly confident in not so easy contexts, such as defining the length of antimicrobial therapy, which is a difficult decision even for senior Infectious Diseases specialists. Residents were more comfortable when making a diagnosis and less confident planning to stop treatments, using combinations of antibiotics or managing pharmacological interactions. This high level of confidence is not supported by evidence12 and, as demonstrated in our survey our residents do not feel comfortable not prescribing antibiotics when the diagnosis is uncertain. Residents from surgical specialties prescribed more antibiotics by themselves than those belonging to medical or critical care specialties, this probably being related to the degree of supervision of the resident in each of these specialty groups. From a different perspective, as expected, the degree of autonomy of the resident increased with experience (years of training).
The overuse and misuse of antimicrobial agents has detrimental effects on patients, the health care system, and society.11 The majority of the respondent physicians agreed that antibiotic overuse is one of the main causes for resistance. Also inappropriate antimicrobial use contributes to the rising cost of health care, the emergence of multidrug-resistant organisms, and adverse drug reactions.12–14
As noted in previous studies,4,15 our residents agreed that knowledge is important to improve the indication and use of antibiotics. They preferred more educational interventions and locally developed guidelines for antimicrobial treatment than other restrictive interventions such as antimicrobials requiring preapproval. Guidelines, in particular, have the additional advantage of offering prescribing support to those physicians who are insecure about optimal antibiotic use.16,17 Restrictions to the initial prescription of some antibiotics is a not a common measure in Spanish hospitals as it was shown in a nation-wide survey on ASP's18 although in other countries it is perceived as a valuable tool to aid the prescription of antibiotics.6 In the same way, this measure appears not to be highly valued by Spanish residents. They also considered useful the availability of infectious diseases specialist, which is consistent with Pulcini et al.6 Interestingly, the approach of the Spanish consensus document about ASP is consistent with residents perceptions, emphasizing on non-restrictive measures to improve antimicrobial use.19
It seems that Spanish residents have important gaps in knowledge regarding prevalence of important pathogens such as QREC and MRSA. Knowledge regarding appropriate use of antibiotics is also limited representing an opportunity for further improvement. The apparent lack of continuing antimicrobial education is also supported by the findings that PGY4-5 did not score significantly higher than first year residents. The implementation of formal antimicrobial education as a requirement for accreditation and one to one specialized feedback on their antimicrobial use and local patterns of resistance are some of the proposed solutions to this problem.
The similarity between residents’ answers in all hospitals included in this survey supports the external validity of our results. To our knowledge, only a few surveys have been published in English3–9 which focused on this topic and only three of them specifically surveyed residents.3–5
However, our study has limitations. As most surveys, there is the possibility that respondent doctors gave socially desirable answers. To minimize this, we ensured complete response confidentiality with a self-reported questionnaire. The response rate (33%) is significantly lower than in Pulcini study, probably because they designated a specific session to complete the survey. In addition, residents belonging to specialities other than medical, surgical or critical care represented 14.3% of the responses, which could have somewhat influenced the overall results.
This survey has demonstrated several areas where antimicrobial stewardship education and intervention activities could be targeted. Exposure to continuing medical education about antimicrobials and resistance is one of the proposed activities to improve antimicrobial prescribing. Design of local guidelines in agreement with all specialties involved in their use, with indications on empiric treatment, antibiotic combinations and optimal duration of antibiotic treatments should be other important activity of the ASP. Reassessment of antibiotic prescriptions 3–5 days after the start of therapy could improve the diagnosis, sequential therapy (parenteral to oral), and duration of the treatment.
FundingThis study was supported by the Ministerio de Ciencia e Innovación, Instituto de Salud Carlos III (Grant: EC07/90338). M. Dolores Del Toro and Jesús Rodríguez-Baño receive funding for research from the Spanish Network for Research in Infectious Diseases (REIPI), Ministerio de Ciencia e Innovación, Instituto de Salud Carlos III – co-financed by European Development Regional Fund “A way to achieve Europe” ERDF, RD06/0008.
Conflicts of interestThe authors have no conflicts of interest to declare.
We acknowledge all resident physicians who responded to the study. We also thank Dr. Jesús Morán-Barrios, Chief of Academic Medical Affairs Unit, Hospital Cruces, Barakaldo for his carefully revision of this manuscript as well as the suggestions made, Dr. Genoveva Yagüe Guirao for microbiological data provided and Dr. Jesús Díez Sebastián (Biostatistics Unit, Hospital Universitario La Paz) for his assistance with the statistical analysis.
Some results of this study were presented as a poster at The European Congress of Clinical Microbiology and Infectious Diseases (ECCMID) in Milan 2011 (Poster-1279).