The main objective of the study was to determine the frequency of patients receiving inappropriate empiric antibiotic therapy and to assess the impact in terms of increase length of hospital stay, 30-day re-admissions, and 30-day mortality.
MethodsAn observational retrospective cohort study was conducted over a one-month period that included all patients hospitalised from an Emergency Department (ED) due to infection. Demographic variables, comorbidity, multi-resistance risk factors, site of infection, microbiological findings, and antibiotic prescribed in ED were collected. Outcomes were length of hospital stay, 30-day re-admissions, and 30-day mortality.
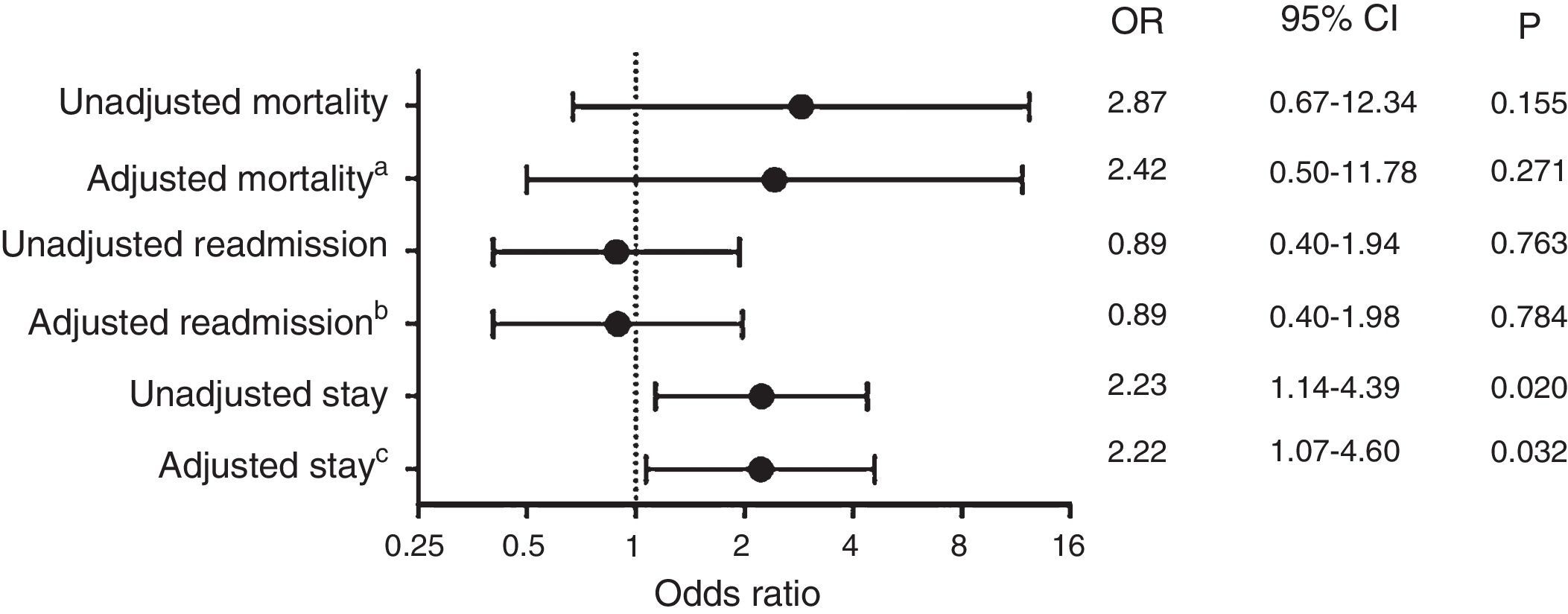
ResultsA total of 376 patients were included, with a mean age of 71.1 (SD 21) years. The most frequent causes were respiratory (45.7%) and urine (23.9%) infections. The number of patients with length of stay over the median (≥9 days) was 165 (46.1%), with re-admissions 74 (19.7%), and mortality at 30 days 44 (11.7%). There was inappropriate antibiotic treatment in 42 (11.2%) cases. After adjusting for demographic data, comorbidity, risk factors for multidrug resistant organism, presence of sepsis criteria in ED, and site of infection, inappropriate treatment was associated with an extended length of hospital stay (OR 2.22; 95% CI; 1.07–4.60; p=0.032), but did not to an increase in mortality (p=0.271) or re-admission (p=0.784) at 30 days.
ConclusionThe inappropriate empirical antibiotic therapy in patients admitted from the ED leads to an extended hospital stay, but did not increase mortality or readmission.
El objetivo principal fue determinar la frecuencia de pacientes que reciben terapia antibiótica inapropiada y evaluar los resultados en términos de estancia media, reingreso y mortalidad a 30 días.
MétodosEstudio observacional de cohortes retrospectivo que incluyó a todos los pacientes ingresados por infección desde un Servicio de Urgencias (SU) durante un mes. Se recogieron variables demográficas, comorbilidad, factores de riesgo de multirresistencia, foco de infección, resultados microbiológicos y antibiótico prescrito en el SU. Las variables de resultado fueron el tiempo de estancia, y la mortalidad y el reingreso a 30 días.
ResultadosSe incluyeron 376 pacientes con una edad media de 71,1 (DE 21) años. Las infecciones más frecuentes fueron respiratoria (45,7%) y urinaria (23,9%). El número de pacientes con una estancia superior a la mediana (≥9 días), reingreso y mortalidad a los 30 días fue de 165 (46,1%), 74 (19,7%) y 44 (11,7%) pacientes, respectivamente. La prescripción inapropiada del tratamiento antibiótico en el SU se produjo en 42 (11,2%) casos. Tras ajustar por los datos demográficos, la comorbilidad, los factores de riesgo para patógenos resistentes, la presencia de sepsis en el SU y el foco de infección, la prescripción inapropiada se asoció a una estancia prolongada (OR 2,22; IC95% 1,07-4,60; p=0,032), pero no a un aumento de la mortalidad (p=0,271) o de los reingresos (p=0,784) a los 30 días.
ConclusiónLa prescripción inapropiada del tratamiento antibiótico empírico en los pacientes ingresados por un proceso infeccioso desde el SU provoca una estancia prolongada, pero no un incremento de la mortalidad o del reingreso.
The term “appropriate treatment” is used widely in the medical literature to refer to therapy that is active against an infection-causing pathogen. If the dose, duration and route of administration are also appropriate, and if it follows current external or local treatment guidelines, it is considered a suitable treatment.1 Numerous studies have shown empirical antibiotic treatment to be inappropriate in a high proportion of cases, estimated at around 50%.2–5 In an emergency setting, the studies suggest that prescribing errors occur most frequently in elderly patients and patients with urinary infections.6–8
A recent epidemiological study found an increased prevalence of infections diagnosed in emergency departments (ED) over the last decade, mostly affecting elderly patients, patients with more comorbidities and more risk factors for multidrug-resistant strains, and patients with more serious conditions.9 However, despite the changing profile of patients being treated and the increased resistance reported in recent years of pathogens that tend to cause community infections, a proportional increase in the use of antibiotics against less common or resistant pathogens has not been seen.9
The inappropriate prescribing of antibiotics could have numerous consequences. Firstly, it could result in increased healthcare costs owing to treatment failure, increased length of hospital stay, increased number of complementary tests performed or the need for admittance to the intensive care unit.10,11 Secondly, one of the main causes of multiple drug resistance is the inappropriate use of antimicrobials, which leads to increased resistance to the antimicrobials prescribed. Resistance can spread from one bacterium to another and from one host to another, who has often not been previously exposed to those antimicrobials. Finally, it may affect the patient's long-term prognosis as it may lead to diminished survival rates in patients with severe sepsis or septic shock.12
In light of the above and of the importance of the issue, a study has been conducted to determine the rate of inappropriate antibiotic prescribing and to assess its consequences in terms of increased mean length of hospital stay, readmittance and short-term mortality of patients, against the need to modify antibiotic treatment or not once admitted.
MethodologyPatient enrolmentObservational, retrospective cohort study. All patients ≥18 years of age admitted due to infection to the ED of a tertiary university hospital between 1 and 31 October 2014 were included. The patients were identified through a hospital administrative database. All patients with any diagnosis of infection at discharge who had been admitted to the ED during the study period were enrolled. Only the first episode to occur during the study period was considered. The study was approved by the Independent Ethics Committee of Hospital Universitario Clínico San Carlos.
Study siteThe Hospital Clínico San Carlos is an urban tertiary university hospital with a catchment area of approximately 500,000 patients in the Autonomous Community of Madrid. The ED treats 350 patients per day on average, 15% of which are treated due to signs of infection.
VariablesThe following variables were collected from the patients’ medical records and recorded on a standardised electronic form: demographic variables (age, gender), the degree of comorbidity according to the Charlson index,13 risk factors for multidrug resistance (immunosuppressive treatment, chronic corticosteroid therapy, surgery in the last month, if the patient had a urinary or central venous catheter, previous hospital admissions in the last 3 months, use of antibiotics for more than 7 days in the last month and referral from a long-term care institution or nursing home), the type of diagnosed infection (respiratory, urinary, intra-abdominal, skin, soft tissue and other), whether the patient met the clinical criteria of sepsis, severe sepsis or septic shock, the antibiotic prescribed in the ED, if this antibiotic was modified during the patient's hospital stay and, if so, the day it was modified and the reason (poor progression, antimicrobial susceptibility) and the results of the microbiological studies conducted. The variable ‘change of antibiotic for any reason’ was also defined, which included those patients whose antibiotic was changed both due to poor progression as well as due to the antimicrobial susceptibility of the isolate. The variable ‘multi-resistant microorganism’ was defined when the anti-microbial susceptibility test demonstrated resistance to 3 or more families or groups of antimicrobials commonly used to treat the corresponding pathogen. The antibiotic treatment was deemed to be inappropriate when it was changed as a result of a lack of sensitivity of the isolated microorganism to the antimicrobial prescribed in the ED. Antibiotics that were descaled or changed as part of sequential treatment were not deemed to be inappropriate. The following were considered to be broad-spectrum antibiotics: ceftazidime, cefepime, carbapenems, piperacillin/ tazobactam, vancomycin, teicoplanin, daptomycin, linezolid and tigecycline. Rifampicin, isoniazid, pyrimethamine and ethambutol were considered to be tuberculostatic treatment. Antibiotics for community pathogens included fluoroquinolones, amoxicillin, ampicillin, amoxicillin/clavulanic acid, ceftriaxone, cefotaxime, macrolides, doxycycline, metronidazole, clindamycin, fosfomycin and co-trimoxazole. Only those antibiotics detailed above were prescribed.
The outcome variables were extended length of hospital stay, mortality and readmission within 30 days of the index event. Extended length of hospital stay was defined as longer than the median length of hospital stay in days for the total study sample. Patients who died during hospitalisation were not considered in the length of stay calculation. The various criteria and parameters were defined in advance by the group based on clinical guidelines and previously published consensuses. The computer systems of the autonomous community were used to determine readmissions and patient mortality within 30 days of the index event.
Statistical analysisAbsolute and relative frequency were used to describe the qualitative variables, while the mean with standard deviation, or the median and the interquartile range were used to describe the quantitative variables, depending on whether the variable met the criteria of normality or not. The effect measures were expressed as odds ratio (OR) with a 95% confidence interval (95% CI). The chi-square test or Fisher's exact test was used for the qualitative variables if more than 25% of the expected frequencies were under 5, and the Student's t test was used to analyse the quantitative variables. A multivariate logistic regression analysis to control the effects of confounding factors was used to identify the independent variables associated with prolonged hospital stay, readmissions and 30-day mortality. Differences were deemed to be statistically significant when the p-value was below 0.05 or when the 95% CI of the OR excluded the value 1. Data processing and analysis was performed using the SPSS® 19.0 statistical package.
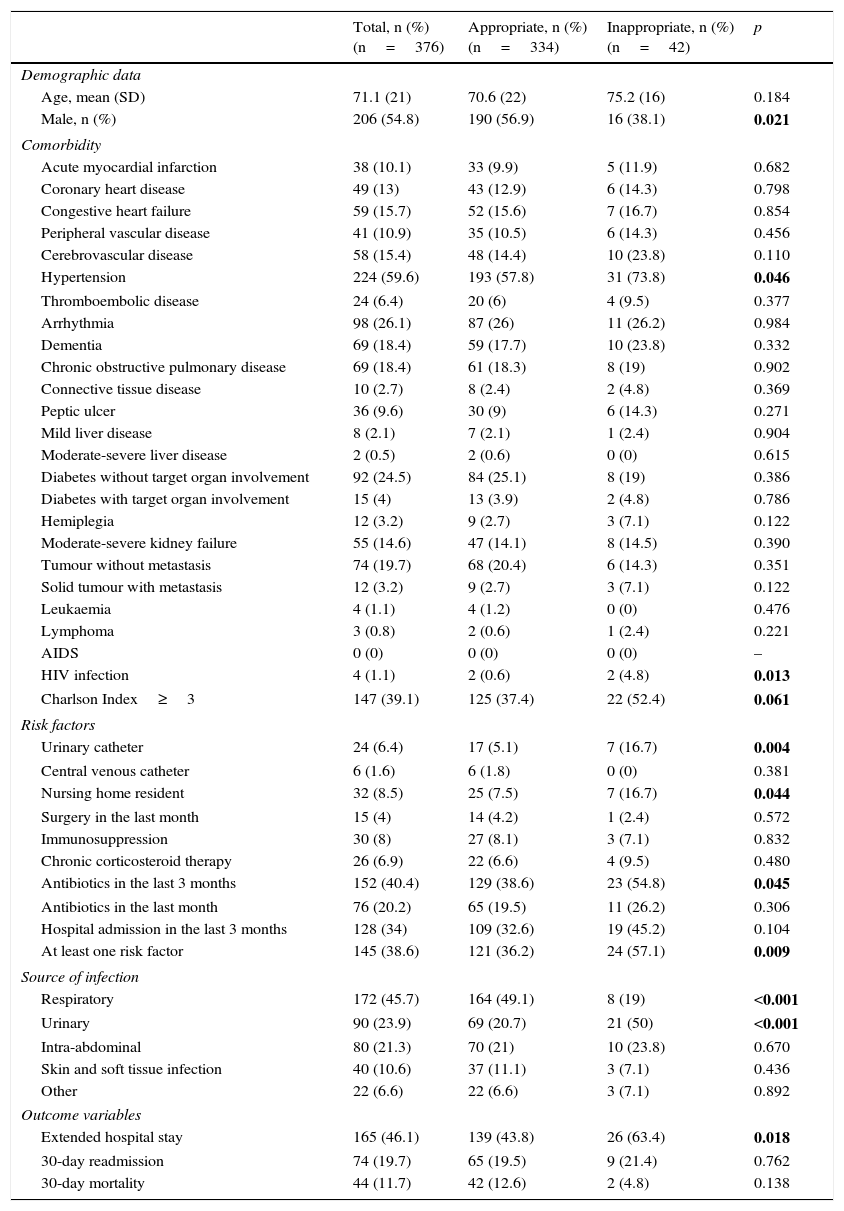
Results376 patients diagnosed with an infection and who were admitted to hospital were enrolled. The mean age was 71.1 (SD 21) years and the majority (54.8%) were male. Respiratory infections were the most common (45.7%), followed by urinary (23.9%). Patient characteristics in relation to the appropriateness of antibiotic prescribing in the ED are described in Table 1. The univariate analysis showed that patients with severe comorbidity and HIV infection were more likely to be prescribed antibiotics inappropriately. They also tended to be nursing home residents, have urinary catheters and have taken antibiotics in the last 3 months. In terms of infection type, in our sample treatment was more likely to be appropriate in respiratory infections and inappropriate in urinary infections.
Patient characteristics grouped in terms of appropriate or inappropriate antibiotic prescribing.
| Total, n (%) (n=376) | Appropriate, n (%) (n=334) | Inappropriate, n (%) (n=42) | p | |
|---|---|---|---|---|
| Demographic data | ||||
| Age, mean (SD) | 71.1 (21) | 70.6 (22) | 75.2 (16) | 0.184 |
| Male, n (%) | 206 (54.8) | 190 (56.9) | 16 (38.1) | 0.021 |
| Comorbidity | ||||
| Acute myocardial infarction | 38 (10.1) | 33 (9.9) | 5 (11.9) | 0.682 |
| Coronary heart disease | 49 (13) | 43 (12.9) | 6 (14.3) | 0.798 |
| Congestive heart failure | 59 (15.7) | 52 (15.6) | 7 (16.7) | 0.854 |
| Peripheral vascular disease | 41 (10.9) | 35 (10.5) | 6 (14.3) | 0.456 |
| Cerebrovascular disease | 58 (15.4) | 48 (14.4) | 10 (23.8) | 0.110 |
| Hypertension | 224 (59.6) | 193 (57.8) | 31 (73.8) | 0.046 |
| Thromboembolic disease | 24 (6.4) | 20 (6) | 4 (9.5) | 0.377 |
| Arrhythmia | 98 (26.1) | 87 (26) | 11 (26.2) | 0.984 |
| Dementia | 69 (18.4) | 59 (17.7) | 10 (23.8) | 0.332 |
| Chronic obstructive pulmonary disease | 69 (18.4) | 61 (18.3) | 8 (19) | 0.902 |
| Connective tissue disease | 10 (2.7) | 8 (2.4) | 2 (4.8) | 0.369 |
| Peptic ulcer | 36 (9.6) | 30 (9) | 6 (14.3) | 0.271 |
| Mild liver disease | 8 (2.1) | 7 (2.1) | 1 (2.4) | 0.904 |
| Moderate-severe liver disease | 2 (0.5) | 2 (0.6) | 0 (0) | 0.615 |
| Diabetes without target organ involvement | 92 (24.5) | 84 (25.1) | 8 (19) | 0.386 |
| Diabetes with target organ involvement | 15 (4) | 13 (3.9) | 2 (4.8) | 0.786 |
| Hemiplegia | 12 (3.2) | 9 (2.7) | 3 (7.1) | 0.122 |
| Moderate-severe kidney failure | 55 (14.6) | 47 (14.1) | 8 (14.5) | 0.390 |
| Tumour without metastasis | 74 (19.7) | 68 (20.4) | 6 (14.3) | 0.351 |
| Solid tumour with metastasis | 12 (3.2) | 9 (2.7) | 3 (7.1) | 0.122 |
| Leukaemia | 4 (1.1) | 4 (1.2) | 0 (0) | 0.476 |
| Lymphoma | 3 (0.8) | 2 (0.6) | 1 (2.4) | 0.221 |
| AIDS | 0 (0) | 0 (0) | 0 (0) | – |
| HIV infection | 4 (1.1) | 2 (0.6) | 2 (4.8) | 0.013 |
| Charlson Index≥3 | 147 (39.1) | 125 (37.4) | 22 (52.4) | 0.061 |
| Risk factors | ||||
| Urinary catheter | 24 (6.4) | 17 (5.1) | 7 (16.7) | 0.004 |
| Central venous catheter | 6 (1.6) | 6 (1.8) | 0 (0) | 0.381 |
| Nursing home resident | 32 (8.5) | 25 (7.5) | 7 (16.7) | 0.044 |
| Surgery in the last month | 15 (4) | 14 (4.2) | 1 (2.4) | 0.572 |
| Immunosuppression | 30 (8) | 27 (8.1) | 3 (7.1) | 0.832 |
| Chronic corticosteroid therapy | 26 (6.9) | 22 (6.6) | 4 (9.5) | 0.480 |
| Antibiotics in the last 3 months | 152 (40.4) | 129 (38.6) | 23 (54.8) | 0.045 |
| Antibiotics in the last month | 76 (20.2) | 65 (19.5) | 11 (26.2) | 0.306 |
| Hospital admission in the last 3 months | 128 (34) | 109 (32.6) | 19 (45.2) | 0.104 |
| At least one risk factor | 145 (38.6) | 121 (36.2) | 24 (57.1) | 0.009 |
| Source of infection | ||||
| Respiratory | 172 (45.7) | 164 (49.1) | 8 (19) | <0.001 |
| Urinary | 90 (23.9) | 69 (20.7) | 21 (50) | <0.001 |
| Intra-abdominal | 80 (21.3) | 70 (21) | 10 (23.8) | 0.670 |
| Skin and soft tissue infection | 40 (10.6) | 37 (11.1) | 3 (7.1) | 0.436 |
| Other | 22 (6.6) | 22 (6.6) | 3 (7.1) | 0.892 |
| Outcome variables | ||||
| Extended hospital stay | 165 (46.1) | 139 (43.8) | 26 (63.4) | 0.018 |
| 30-day readmission | 74 (19.7) | 65 (19.5) | 9 (21.4) | 0.762 |
| 30-day mortality | 44 (11.7) | 42 (12.6) | 2 (4.8) | 0.138 |
Results with p<0.05 are displayed in bold.
In terms of the severity of the patient's condition upon arrival at the ED, 117 (31.1%) met sepsis criteria, 50 (13.3%) severe sepsis criteria and 4 (1.1%) septic shock criteria. Median length of hospital stay of the patients studied was 9 days (interquartile range 5–15 days). 165 patients (46.1%) had an extended hospital stay longer than 9 days. There were 74 readmissions (19.7%) and 44 patients (11.7%) died.
Microorganisms were isolated from the valid microbiological samples of 159 patients (42.3%), 64 (17%) of which were found to be multidrug-resistant. In terms of type of antibiotic, antimicrobials for community pathogens were prescribed to 226 patients (60.1%), broad-spectrum antibiotics to 147 (39.1%) and tuberculostatic drugs to 3 patients (0.8%).
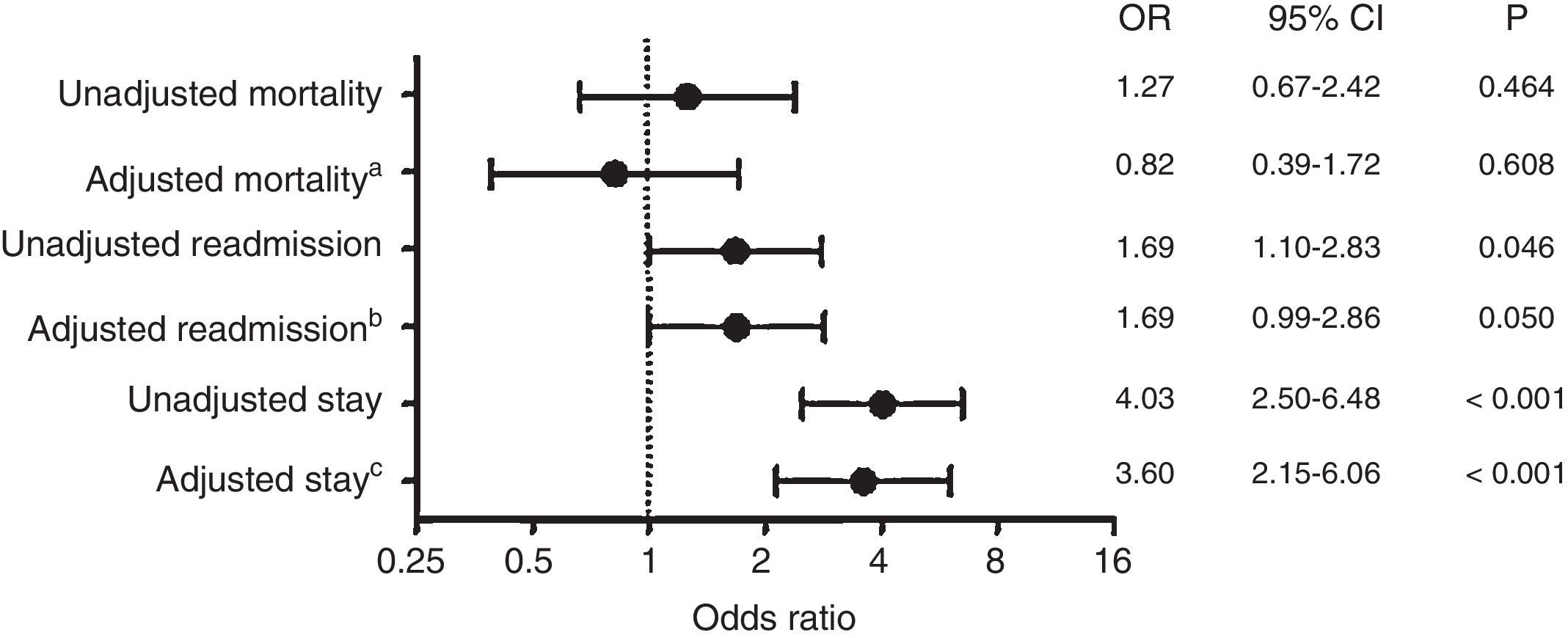
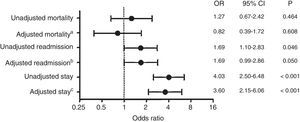
Once admitted to the ward, the antibiotic was changed in 134 patients (35.6%), 42 (11.3%) due to inappropriate treatment and 92 (24.6%) due to poor clinical progression. Treatment was changed in the first 48h of admission in 52.9% of cases. Fig. 1 shows the non-adjusted and adjusted risks of inappropriate prescribing for each outcome variable, revealing that inappropriate prescribing is an independent factor associated with extended length of hospital stay, but not with 30-day mortality or readmission. Based on the same multivariate analysis, Fig. 2 shows that if we only consider change of treatment during hospitalisation, regardless of the reason for the change, this is associated with an extended length of hospital stay and a trend towards 30-day readmission, but not with increased short-term mortality.
Effects of inappropriate treatment on hospital stay, mortality and readmissions, both unadjusted and adjusted for demographic data, comorbidity, risk factors for resistant pathogens, sepsis in the ED and source of infection. aAdjusted for admission<3 months, Charlson≥3, chronic obstructive pulmonary disease, dementia, respiratory infection, sepsis in the ED, moderate-severe kidney failure, any risk factor for resistant microorganisms, nursing home resident, immunosuppression, peripheral vascular disease and antibiotic use for more than 7 days in the last month. bAdjusted for diabetes, intra-abdominal infection and prior admission. cAdjusted for admission<3 months, Charlson≥3, chronic obstructive pulmonary disease, dementia, respiratory infection, sepsis in the ED, any risk factor for resistant microorganisms, tumour.
Effects of change of antibiotic for any reason on hospital stay, mortality and readmissions, both unadjusted and adjusted for demographic data, comorbidity, risk factors for resistant pathogens, sepsis in the ED and source of infection. aAdjusted for admission<3 months, Charlson≥3, chronic obstructive pulmonary disease, dementia, respiratory infection, sepsis in the ED, moderate-severe kidney failure, any risk factor for resistant microorganisms, nursing home resident, immunosuppression, peripheral vascular disease and antibiotic use for more than 7 days in the last month. bAdjusted for diabetes, intra-abdominal infection and prior admission. cAdjusted for admission<3 months, Charlson≥3, chronic obstructive pulmonary disease, dementia, respiratory infection, sepsis in the ED, any risk factor for resistant microorganisms, tumour.
In our sample, antibiotics were only prescribed inappropriately to one in 10 patients. The limited number of patients affected may explain why no significant differences were found in terms of mortality and readmissions, but an increase in the length of hospital stay was observed in many patients. The delayed administration of an appropriate antibiotic may not only lead to delayed control of the infection and of the bacterial inoculum, but may also hinder and delay the identification of patient comorbidities, which are often acute conditions, especially in elderly patients and patients susceptible to comorbidities that are typically treated in emergency departments. This would explain the extended length of hospital stay seen in patients prescribed inappropriate treatment. Other studies have shown that inappropriate prescribing leads to increased mortality,14,15 although it should be noted that these studies were conducted on patients with severe sepsis and septic shock, where, due to the severity of the condition, decisions taken could have a major impact on the patient's health. Nevertheless, we should not overlook the significance of extended hospital stay in terms of the increased costs incurred by the health system. Numerous studies have suggested that extended hospital stay represents the biggest expenditure in terms of the cost of treating infection.16–18
Other studies have found inappropriate treatment rates to vary widely, but all were higher than in our sample.2,3 The widespread use in our ED of empirical antibiotic treatment protocols for the most prevalent infectious diseases, as well as the regular reporting by our Microbiology Department of the antimicrobial sensitivity test results of the main microorganisms, may explain why the risk of inappropriate prescribing is lower. Some publications have shown the effectiveness of following clinical guidelines to improve appropriate prescribing.19,20 What is more, an aetiological diagnosis was only established in 2 out of every 5 patients, which means that the rate of incorrect prescribing may have been underestimated as patients without an aetiological diagnosis were not considered.
Conclusions can probably also be drawn from the change of antibiotic treatment results, regardless of the reason for the change. The initial antibiotic was changed in 2 out of every 5 patients. These patients experienced an increased length of hospital stay and a higher risk of 30-day readmission, but no increased mortality. As well as the increased cost it represents, hospital readmission is also a measure of the quality of healthcare received and may be indicative of inadequate healthcare provision.
The study shows a high rate of multidrug-resistant microorganisms in the population treated in the ED (17%). The following considerations may justify this finding. Firstly, by taking into account current data concerning the sensitivity of some of the major community pathogens. Published sensitivity studies show enterobacteriaceae resistance to quinolones, and Staphylococcus aureus resistance to beta-lactam antibiotics to be above 30% in Spain. They also reveal the emergence of resistance to extended-spectrum beta-lactamases and carbapenems,21 as well as the increasingly common manifestation of multidrug-resistant pathogens such as Pseudomonas spp. in patients coming from the community, owing to increased survival rates of patients with chronic obstructive pulmonary disease or the rise in the number of immunosuppressed patients. Secondly, it should be noted that the profile of patients enrolled in the study – elderly and with multiple comorbidities and risk factors for multidrug-resistant microorganisms – may also justify these findings. Two out of every 5 patients presented a Charlson index≥3 and 2 out of every 5 had at least one resistance risk factor. The same percentage of patients had completed a full cycle of antibiotics in the previous month. Finally, the study enrolled patients with relatively complex conditions requiring hospital admission.
This study has certain limitations. Firstly, it was conducted on patients who were admitted due to infection from a single ED. Secondly, when prescribing an antibiotic, it is not only important to consider the drug's sensitivity, but also an appropriate dosing regimen (dose, dosing interval, treatment duration, route and conditions of administration), adequate diffusion to the source of the infection, interaction with other drugs taken by the patient, its use in combination when indicated and its prompt administration. In other words, antimicrobial susceptibility is not the only criterion for assessing the appropriateness of antibiotic treatment. Finally, a stratified analysis of the source of infection or the influence of the molecule used was not conducted.
Despite the above limitations, this study offers interesting data on the implications of inappropriate antibiotic prescribing and change of antibiotic treatment for any reason in the emergency department of a highly-specialised university hospital. In conclusion, our findings suggest that the inappropriate prescribing of empirical antibiotics in patients referred from the ED due to infection, results in an extended hospital stay but not to increased mortality or readmissions.
FundingUnfunded study.
Conflicts of interestNone.
Please cite this article as: González-del Castillo J, Domínguez-Bernal C, Gutiérrez-Martín MC, Núñez-Orantos MJ, Candel FJ, Martín-Sánchez FJ. Efecto de la inadecuación de la antibioterapia en Urgencias sobre la eficiencia en la hospitalización. Enferm Infecc Microbiol Clin. 2017;35:208–213.