The improvement in the prognosis of HIV infection, coupled with the increase in international travel and migration, has led to a rising number of HIV infected travelers. The objective of this study was to describe the epidemiological and clinical features of returning travelers, according to their HIV status.
MethodsAn observational prospective study was conducted including travelers and immigrants who traveled to visit friends and relatives (VFRs) registered in the +REDIVI collaborative network (January-2009; October-2014). +REDIVI is a national network that registers information regarding infections imported by travelers and immigrants at 21 different centers using a standardized protocol.
ResultsA total of 3464 travellers were identified: 72 were HIV+ (2.1%) and 3.392 HIV− (98%). HIV+ vs. HIV− travelers were often older (40.5y vs. 34.2y P=.001), VFRs (79.1% vs. 44.4%; P<.001), and consulted less for pre-travel advice (27% vs. 37%; P=.078). The main destinations for both groups were sub-Saharan Africa and Latin America. The most frequent reasons for consultation after travel were fever, request for a health examination, gastrointestinal complaints, and abnormal laboratory tests (mainly eosinophilia and anemia), which differed between groups. The most frequent diagnoses in HIV+ travelers were malaria (38.8%), newly diagnosed HIV infection (25%), and intestinal parasites (19.4%), while for HIV− travelers the main diagnoses were “healthy” (17.9%), malaria (14%), and intestinal parasites (17.3%).
ConclusionsThe typical profile of an HIV+ traveler in +REDIVI was that of a VFR traveler who did not seek pre-travel advice and made high-risk trips. This may increase the chance of acquiring travel-related infections which may pose a special risk for HIV-infected travelers. The post-travel visit was a good opportunity for HIV infection screening.
La mejoría en el pronóstico de la infección por el VIH, sumada al incremento de los viajes y la inmigración, han aumentado la frecuencia del binomio viajero-VIH+. El objetivo de este trabajo es describir la epidemiología y hallazgos clínicos de los viajeros VIH+ en comparación con los VIH-.
MétodosEstudio observacional y prospectivo, de los viajeros e inmigrantes viajeros que se desplazan para visitar familiares y amigos (VFR) incluidos en la red +REDIVI (enero-2009; octubre-2014). +REDIVI es una red nacional que recopila información sobre infecciones importadas por viajeros e inmigrantes en 21 centros mediante un protocolo estandarizado de recogida de datos.
ResultadosSe identificaron 3.464 viajeros: 72 VIH+ (2,1%) y 3.392 VIH− (98%). Los VIH+ en contraste con los VIH−, eran mayores (40 vs. 34 años; p=0,001), predominantemente VFR (79,7% vs 44,4%. p<0,001), y solicitan menos consejo pre-viaje (27% vs 37%. p=0,078). Los destinos predominantes para ambos grupos fueron África Subsahariana y Latinoamérica. Los motivos de consulta más frecuentes al retorno del viaje fueron la fiebre, solicitar un examen de salud, molestias gastrointestinales, y anomalías en los resultados de laboratorio (principalmente eosinofilia y anemia) los cuales variaron según el grupo. Los diagnósticos más frecuentes en los VIH+ fueron la malaria (38,8%), nuevo diagnóstico de VIH (25%) y parasitosis intestinales (19,4%), mientras que en los sujetos VIH− los principales diagnósticos fueron “sano” (17,9%), parásitos intestinales (17,3%) y malaria (14%).
ConclusionesEl perfil más común del viajero VIH+ atendido en +Redivi es el de un inmigrante VFR que no solicita consejo pre-viaje y hace viajes de alto riesgo. Esto puede suponer un mayor riesgo de adquisición de infecciones relacionadas con el viaje, las cuales en un viajero VIH+ pueden tener un efecto deletéreo adicional. La consulta tras el viaje es una buena oportunidad para el cribado de la infección por VIH.
International travel has been growing at a sustained pace over the last two decades. A total of 1087 million people traveled overseas in 2013,1 while 232 million in the same year were living outside their country of birth, a number that continues to increase.2
Travelers from high income countries to tropical destinations face a potential health gradient between their country of origin and the country of destination.3 Health professionals should be particularly concerned about travelers with immunosuppressive conditions such as HIV infection, as these might alter an infectious disease's natural course. Accurate information on the profile of immunocompromised travelers is scarce and usually obtained from travel clinics before the trip or at HIV outpatient departments after travel.4–7 Some data indicate these patients often do not seek pre-travel advice.6–8 Few studies describe the health problems of HIV-infected patients seeking medical advice after travel. According to recent studies, up to 29.2% consulted due to an infection on return,8 and traveller's diarrhea, respiratory tract infections and skin disorders were the most common syndromes.6,7 However, information is limited about reasons for travel, specific diagnoses, countries of acquisition, and patient type (migrant or tourist).
The introduction of combined antiretroviral therapy (cART) has changed the prognosis of HIV infection9: considered a fatal disease at the beginning of the pandemic it has become a chronic condition from the mid nineties onwards.10 Patients receiving cART nowadays have a similar life expectancy to those who are not HIV infected,10 along with improved physical fitness and a growing interest for travel.7 HIV infection does not prevent patients from choosing tropical destinations7 and the proportion of HIV infected people among travelers has increased in some series.5
Migration to Spain has also increased in the last decades and migrants represent 11.7% of the current population.11 Data on HIV prevalence among non-selected migrant populations in Spain vary according to countries of origin and ranges from 0.3 to 1.7%, being higher in Sub-Saharan Africans.12
Migrants who travel to visit friends and relatives (VFRs), may be at an increased risk of acquiring a travel-related disease, whether they are infected with HIV or not. VFRs are known to travel for more time, often to rural and remote areas, may have closer contact with the local population and appear to take less precautions with food and beverages than conventional tourists.13 The prevalence of HIV infection in this population could be increased depending on country of origin.13 Nevertheless, data concerning HIV infection and travel-related diseases among VFRs are lacking.
The aim of this study was to describe the epidemiological characteristics, travel destinations and risks, along with the reasons for consultation and final diagnoses in HIV-infected travelers compared to HIV-negative travelers.
MethodsThis was an observational study based on a prospective cohort selected from the Spanish network on Infectious Diseases Imported by Travelers and Immigrants (+REDIVI). This network comprises 21 medical centers (1 primary care center and 20 hospitals, both specialized and non-specialized in travel medicine) in different regions in Spain. The network shares a common database for on-line data registry on imported infections, where demographic, clinical and travel-related data are collected according to a standardized protocol,14 which includes HIV serology (HIV testing is voluntary). Data cannot be linked back to an individual patient as these are codified when registered in the database. The population included in +REDIVI comprises immigrants from any country and returned travelers, defined as any person who crossed an international border before seeking medical advice for a presumed travel-related disease or for screening for asymptomatic infections. The network also includes well-established migrants, or their descendants, who come to consultation after traveling to visit friends and relatives in their countries of origin (VFRs).
Data were obtained from travelers included in the +REDIVI network during the period January 2009 to October 2014. Immigrants and patients with other causes of immunosuppression were excluded. Two main populations were compared: HIV-infected travelers (HIV+) vs. non-HIV infected travelers (HIV−). Additionally for HIV+ travelers, the characteristics of those traveling to visit friends and relatives (HIV+VFR) vs. conventional tourists (HIV+CT) were compared.
A descriptive analysis was performed and possible associations between epidemiological and clinical data according to HIV status were tested. Age, sex, country of origin, type of case (conventional-tourist or VFR), country of destination, travel-associated risk (travelers with non-planned journeys, missionaries, backpackers, aid workers, and travelers taking adventure trips or staying in rural areas were considered high risk travelers), duration of travel, time elapsed from arrival to consultation, reason for seeking medical care and final diagnosis were analyzed. Qualitative variables were expressed as relative and absolute frequencies, and quantitative data were expressed as median and interquartile range (IQR). Association between qualitative data were analyzed with the χ2 and Fisher exact test as appropriate; while unpaired Student's t test, or Mann–Whitney's U were used for quantitative data.
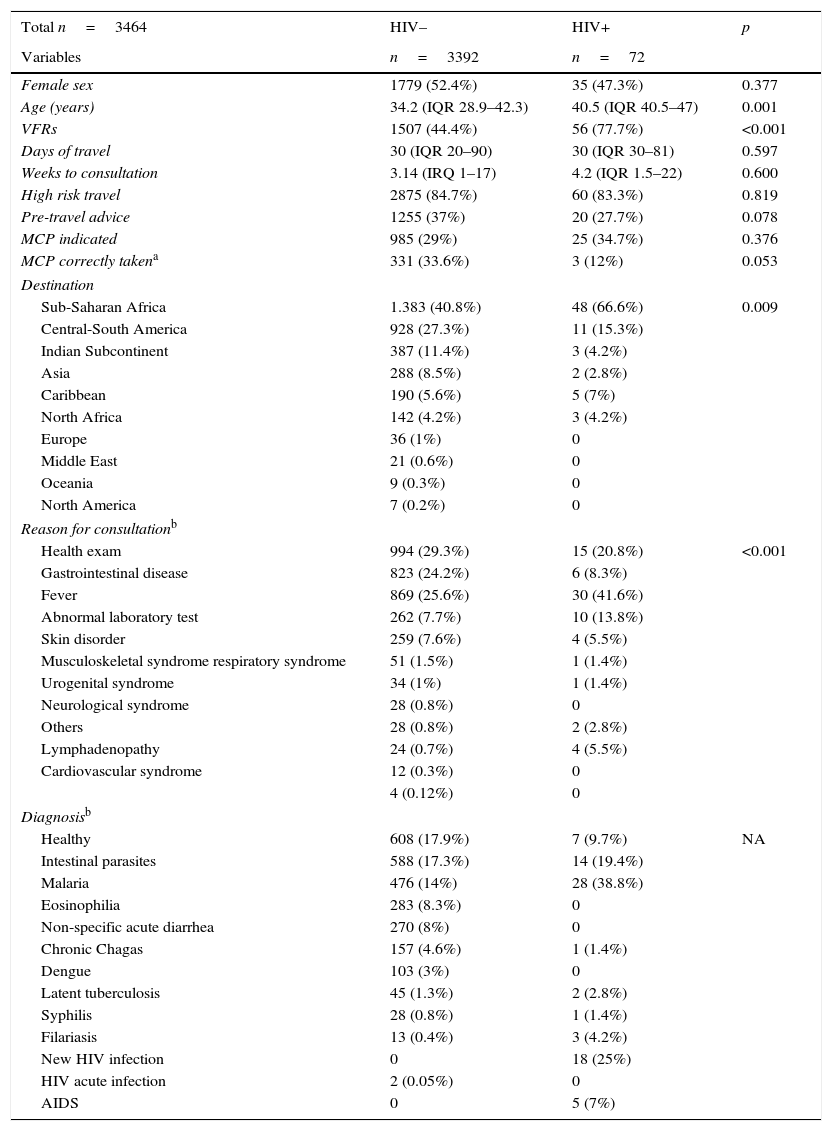
ResultsCharacteristic of travelers according to HIV statusBy October 2014 the +REDIVI network had registered 9120 cases of people seeking medical care. Out of these, 3464 were travelers (1899 national-travelers and 1565 VFRs). In total, 72 cases of HIV infection were identified (Table 1), of which 18 (25%) were newly diagnosed HIV infections and 2 were acute infections. Ten patients (13.5%) had at least one AIDS defining condition according to CDC criteria.15 Five patients were diagnosed with such a condition at the time of consultation (2 had disseminated tuberculosis, 1 cerebral toxoplasmosis, 1 Kaposi's sarcoma and 1 had Pneumocystis jiroveci pneumonia), and for two of these patients this condition was diagnosed at the same time as the HIV infection. The other five had been diagnosed with AIDS previously (registered conditions were 3 Kaposi's sarcomas, 2 disseminated tuberculosis, 1 cerebral toxoplasmosis, and 1 unregistered AIDS-defining condition as some of these patients had more than one condition).
Characteristics of travelers according to HIV status.
| Total n=3464 | HIV– | HIV+ | p |
|---|---|---|---|
| Variables | n=3392 | n=72 | |
| Female sex | 1779 (52.4%) | 35 (47.3%) | 0.377 |
| Age (years) | 34.2 (IQR 28.9–42.3) | 40.5 (IQR 40.5–47) | 0.001 |
| VFRs | 1507 (44.4%) | 56 (77.7%) | <0.001 |
| Days of travel | 30 (IQR 20–90) | 30 (IQR 30–81) | 0.597 |
| Weeks to consultation | 3.14 (IRQ 1–17) | 4.2 (IQR 1.5–22) | 0.600 |
| High risk travel | 2875 (84.7%) | 60 (83.3%) | 0.819 |
| Pre-travel advice | 1255 (37%) | 20 (27.7%) | 0.078 |
| MCP indicated | 985 (29%) | 25 (34.7%) | 0.376 |
| MCP correctly takena | 331 (33.6%) | 3 (12%) | 0.053 |
| Destination | |||
| Sub-Saharan Africa | 1.383 (40.8%) | 48 (66.6%) | 0.009 |
| Central-South America | 928 (27.3%) | 11 (15.3%) | |
| Indian Subcontinent | 387 (11.4%) | 3 (4.2%) | |
| Asia | 288 (8.5%) | 2 (2.8%) | |
| Caribbean | 190 (5.6%) | 5 (7%) | |
| North Africa | 142 (4.2%) | 3 (4.2%) | |
| Europe | 36 (1%) | 0 | |
| Middle East | 21 (0.6%) | 0 | |
| Oceania | 9 (0.3%) | 0 | |
| North America | 7 (0.2%) | 0 | |
| Reason for consultationb | |||
| Health exam | 994 (29.3%) | 15 (20.8%) | <0.001 |
| Gastrointestinal disease | 823 (24.2%) | 6 (8.3%) | |
| Fever | 869 (25.6%) | 30 (41.6%) | |
| Abnormal laboratory test | 262 (7.7%) | 10 (13.8%) | |
| Skin disorder | 259 (7.6%) | 4 (5.5%) | |
| Musculoskeletal syndrome respiratory syndrome | 51 (1.5%) | 1 (1.4%) | |
| Urogenital syndrome | 34 (1%) | 1 (1.4%) | |
| Neurological syndrome | 28 (0.8%) | 0 | |
| Others | 28 (0.8%) | 2 (2.8%) | |
| Lymphadenopathy | 24 (0.7%) | 4 (5.5%) | |
| Cardiovascular syndrome | 12 (0.3%) | 0 | |
| 4 (0.12%) | 0 | ||
| Diagnosisb | |||
| Healthy | 608 (17.9%) | 7 (9.7%) | NA |
| Intestinal parasites | 588 (17.3%) | 14 (19.4%) | |
| Malaria | 476 (14%) | 28 (38.8%) | |
| Eosinophilia | 283 (8.3%) | 0 | |
| Non-specific acute diarrhea | 270 (8%) | 0 | |
| Chronic Chagas | 157 (4.6%) | 1 (1.4%) | |
| Dengue | 103 (3%) | 0 | |
| Latent tuberculosis | 45 (1.3%) | 2 (2.8%) | |
| Syphilis | 28 (0.8%) | 1 (1.4%) | |
| Filariasis | 13 (0.4%) | 3 (4.2%) | |
| New HIV infection | 0 | 18 (25%) | |
| HIV acute infection | 2 (0.05%) | 0 | |
| AIDS | 0 | 5 (7%) | |
HIV–, non-HIV infected traveller; HIV+, HIV-infected traveller; VFR, patients visiting friends and relatives; MCP, malaria chemoprophylaxis; AIDS, acquired immunodeficiency syndrome.
HIV+ patients were older and more frequently VFRs, when compared with HIV− travelers. Duration of travel was similar in both groups, as well as time elapsed from arrival to consultation. Most patients, both HIV+ and HIV−, referred trips considered as of high risk for acquiring a travel-related disease. Despite this fact, few patients referred seeking pre-travel medical advice. In addition, malaria chemoprophylaxis (MCP) was indicated in one third of patients (both HIV+ and HIV−), but only 12% of the HIV+ and 33.6% of the HIV− took it correctly (Table 1).
Top five destinations identified among the HIV+ group were, in order of frequency, Sub-Saharan Africa (66.6%); Central and South America (15.3%); the Caribbean (7%), the Indian subcontinent and Northern Africa (4.2%, each) and Asia (2.8%). HIV− patients traveled mainly to Sub-Saharan Africa (40.7%); Central and South America (27.3%); the Indian Subcontinent (11.4%), Asia (8.5%) and the Caribbean (5.6%) (Table 1).
The most common reasons for seeking medical advice among HIV+ travelers were fever (41.6%), request for a health exam (20.8%), laboratory test abnormalities (13.1%; mainly eosinophilia and anemia), gastrointestinal syndromes (8.3%) or a skin disorder (5.5%). HIV− travelers mainly presented to a +REDIVI clinic in order to undergo a health exam (29.3%), due to fever (25.6%), a gastrointestinal syndrome (24.2%), abnormal laboratory findings (7.7%; mainly eosinophilia and anemia), and skin disorders (7.6%) (Table 1).
The most common diagnoses in the HIV+ group were: malaria in 38.8% cases, newly diagnosed HIV infection for 25% of cases, intestinal parasites occurred in 19.4%, 9.7% were considered to have no travel-related diseases, and filarial blood species were diagnosed in 4.2%. In contrast, the most common diagnoses in the HIV− group were: healthy (17.3%), intestinal parasites (17.3%), malaria (14%), eosinophilia (8.3%), acute unspecific diarrhea (8%), chronic Chagas disease (4.6%) and dengue (3%) (Table 1).
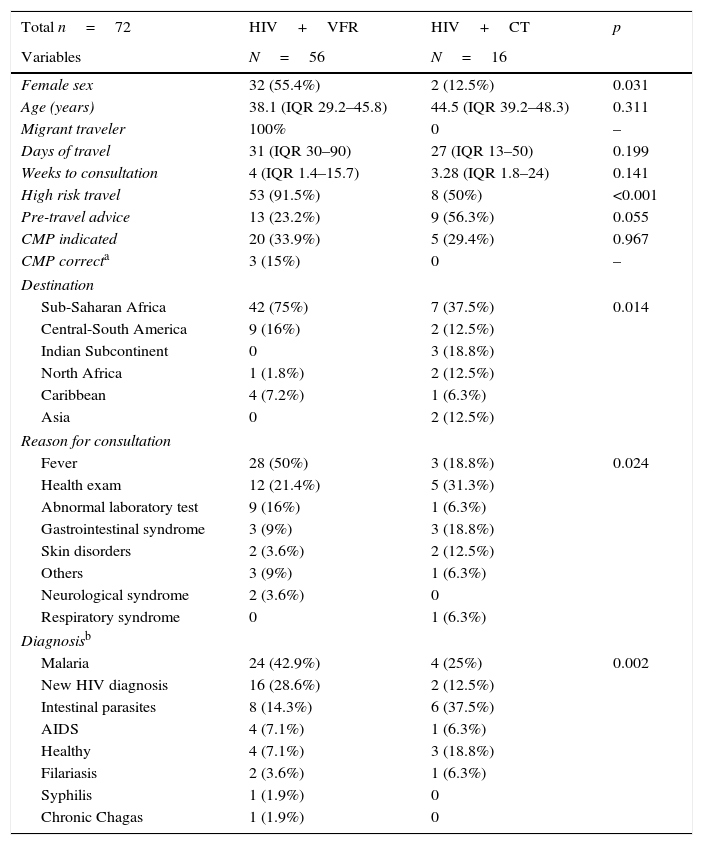
Characteristics of HIV+ travelers according to case-type: conventional tourists and VFRsAmong the 72 HIV+ travelers, 16 (22.2%) were HIV+ conventional tourists (HIV+CT) and 56 (77.8%) were HIV+VFRs. HIV+CT were more frequently male. Duration of travel and time elapsed from arrival to consultation were similar for both subgroups. HIV+CT sought pre-travel advice more frequently than HIV+VFR, and had gone on less high risk trips. Malaria prophylaxis was indicated in 25 HIV+ patients, 5 of whom were HIV+CT and 20 were HIV+VFR; but only 3 patients took it correctly, all in the HIV+VFR group (Table 2).
Characteristics of the HIV+ travelers according to type of case.
| Total n=72 | HIV+VFR | HIV+CT | p |
|---|---|---|---|
| Variables | N=56 | N=16 | |
| Female sex | 32 (55.4%) | 2 (12.5%) | 0.031 |
| Age (years) | 38.1 (IQR 29.2–45.8) | 44.5 (IQR 39.2–48.3) | 0.311 |
| Migrant traveler | 100% | 0 | – |
| Days of travel | 31 (IQR 30–90) | 27 (IQR 13–50) | 0.199 |
| Weeks to consultation | 4 (IQR 1.4–15.7) | 3.28 (IQR 1.8–24) | 0.141 |
| High risk travel | 53 (91.5%) | 8 (50%) | <0.001 |
| Pre-travel advice | 13 (23.2%) | 9 (56.3%) | 0.055 |
| CMP indicated | 20 (33.9%) | 5 (29.4%) | 0.967 |
| CMP correcta | 3 (15%) | 0 | – |
| Destination | |||
| Sub-Saharan Africa | 42 (75%) | 7 (37.5%) | 0.014 |
| Central-South America | 9 (16%) | 2 (12.5%) | |
| Indian Subcontinent | 0 | 3 (18.8%) | |
| North Africa | 1 (1.8%) | 2 (12.5%) | |
| Caribbean | 4 (7.2%) | 1 (6.3%) | |
| Asia | 0 | 2 (12.5%) | |
| Reason for consultation | |||
| Fever | 28 (50%) | 3 (18.8%) | 0.024 |
| Health exam | 12 (21.4%) | 5 (31.3%) | |
| Abnormal laboratory test | 9 (16%) | 1 (6.3%) | |
| Gastrointestinal syndrome | 3 (9%) | 3 (18.8%) | |
| Skin disorders | 2 (3.6%) | 2 (12.5%) | |
| Others | 3 (9%) | 1 (6.3%) | |
| Neurological syndrome | 2 (3.6%) | 0 | |
| Respiratory syndrome | 0 | 1 (6.3%) | |
| Diagnosisb | |||
| Malaria | 24 (42.9%) | 4 (25%) | 0.002 |
| New HIV diagnosis | 16 (28.6%) | 2 (12.5%) | |
| Intestinal parasites | 8 (14.3%) | 6 (37.5%) | |
| AIDS | 4 (7.1%) | 1 (6.3%) | |
| Healthy | 4 (7.1%) | 3 (18.8%) | |
| Filariasis | 2 (3.6%) | 1 (6.3%) | |
| Syphilis | 1 (1.9%) | 0 | |
| Chronic Chagas | 1 (1.9%) | 0 | |
HIV+CT, HIV-infected common traveler; HIV+VFR, HIV-infected traveler who travels to visit friends and relatives; MCP, malaria chemoprophylaxis; AIDS, acquired immunodeficiency syndrome.
Destinations among HIV+CT were more varied than for HIV+VFR, but namely: Sub-Saharan Africa (37.5%), Indian subcontinent (18.8%), Northern Africa and Central-South America (12.5% each) or the Caribbean (6.3%). While nearly all destinies among HIV+VFR were in: Sub-Saharan Africa (75%), Central and South America (16%) and the Caribbean (7.2%) (Table 2)
The main reasons for consultation in HIV+CT were: Health exam (29.4%), fever (23.5%), gastrointestinal symptoms (17.6%), skin disorders (11.7%), respiratory symptoms or abnormal laboratory findings (5.8% each). HIV+VFR consulted more frequently for fever (50%), for a health exam (21.4%) or due to an abnormal laboratory test (16%) and less frequently for gastrointestinal symptoms or others reasons (9% each) (Table 2).
The HIV+CT group had a wide variety of diagnoses: intestinal parasites (37.5%), malaria (25%), no travel-related disease (18.8%), newly diagnosed HIV infection (12.5%) and AIDS defining conditions or filarial disease (6.3%). While the main diagnoses among HIV+VFRs were malaria (42.9%), newly diagnosed HIV infection (28.6%), intestinal parasites (14.3%) and AIDS defining conditions or no travel-related disease (7.1% each) (Table 2). More than one third of both subgroups had more than one diagnosis.
DiscussionThe typical profile of an HIV+ traveler in +REDIVI is that of an infected migrant who travels to visit friends and relatives and does not seek previous travel advice, even if the trip is considered high-risk. As a result, he/she might find him/herself at an increased risk for acquiring a travel-related infection, for which HIV might have an additional deleterious effect. Although the sample size of the study is small, the HIV+ conventional tourist seems to attend for pre-travel advice more often and undergoes less high-risk travels, in accordance with the profile of a regular HIV− traveler in +REDIVI.14
HIV+ travelers were older and more frequently migrants who traveled to visit friends and relatives compared with HIV− travelers. Demographic characteristics such as age and sex were in accordance with national data on HIV infected persons where the proportion of men for the same period ranged from 82.1% to 85% and the median age was 36–37 years old.16,17 Similarly, the increased proportion of VFRs in our study is concordant with the increasing proportion of VFRs among international travellers.13,18,19 Additionally, HIV infection rates in the VFR subgroup were significantly higher than in the autochthonous traveler subgroup (3.6% vs. 0.9%; p<0.001). This probably reflects higher prevalence rates of HIV infection among certain migrant populations, such as Sub-Saharan Africans,20–22 who constitute an important proportion in +REDIVI.
Regarding travel characteristics, 90.3% of the HIV+ group traveled to Sub-Saharan Africa or Latin America, reflecting the large proportion of migrants traveling to their countries of origin, while HIV− travelers showed somewhat more variation in destinations. In contrast; comparison of pre-travel advice, travel duration and risk, time to consultation, or indication for malaria chemoprophylaxis or compliance, showed no major differences, suggesting HIV status is not related to these travel-related practices.
Reasons for consultation and final diagnosis differed between HIV+ and HIV− travelers, which may be attributable to a difference in risk exposure between both groups, as destinations and reasons for travel (proportion of people traveling to visit friends and relatives) differed between groups. HIV+ travelers consulted more frequently due to fever, and most were found to have malaria (2.8 times more frequent in HIV+ than HIV−), which occurred solely in those coming from Sub-Saharan Africa. The relative proportion of VFRs in the HIV+ population was probably responsible for this association.19 Other common diagnoses were normal health exam and intestinal parasites.
Of note, 25% of the HIV cases were newly diagnosed infections (20/74) and 2 (2/20, 10%) were acute infections. Despite this, only two of the 20 patients (10%) with newly diagnosed HIV presented with an AIDS defining condition at the time of the visit. This suggests the general screening protocol proposed in +REDIVI, which includes universal HIV screening, could be of use to detect new cases of HIV infection which may also be diagnosed earlier in the natural history of the disease. In addition, three patients known to be HIV positive presented with AIDS defining conditions following travel and five patients with previous AIDS-defining conditions traveled abroad. This highlights the importance of adequately assessing and monitoring these travelers.
HIV− patients came to a +REDIVI clinic mostly for a health exam, or due to gastrointestinal symptoms, fever, abnormal laboratory findings (eosinophilia) and skin disorders; and many were finally found healthy or were diagnosed with intestinal parasites, malaria, or acute non-specific diarrhea. These data are in accordance with the most relevant published series in travellers.18,19,23 Some chronic infections, such as Chagas disease and filarial infections were also detected following our tailored screening protocol for geographically related infections.
This is one of the few studies providing data from travelers infected with HIV that seek medical advice after travel. The main strength of our study is its external validity, as data were obtained from 21 different health centers, specialized in travel medicine or not, attending both HIV-infected and non-infected people. As a major limitation, no further information on HIV immune or clinical stage, or regarding HIV treatment was recorded. Additionally, these data were obtained from people attending a +REDIVI clinic and do not reflect the whole traveler population. Nevertheless this limitation may be counter-balanced by the fact that clinics in the Spanish National Health System attend people free of charge (and many patients were seen in order to perform a health exam).
When travelers in +REDIVI were compared according to their HIV status, some characteristics attributable to VFRs stand out, such as older age, gender balance, lack of pre-travel advice and high risk travels to Africa or Latin America. Clinicians should be aware that the latter two conditions imply a higher risk for acquiring travel-related infections, such as malaria, and HIV infection might have an additional deleterious effect. The HIV+CT appear to be similar to the HIV− travelers generally seen in +REDIVI, adopting more preventive measures and avoiding high-risk travels more often. As the most common profile of an HIV+ traveler attended at a +REDIVI clinic belongs to a migrant who travels to visit friends and relatives, this population might constitute a special target group for receiving health education and pre-travel tailored advice. Consultation after travel is a good opportunity to test for HIV infection.
Conflict of interestThe authors declare no conflicts of interest.
We would like to thank Ms. Liliana Moreno for her kind support in data registry and management. This work was funded by the VI PN de I+D+I 2008–2011, ISCIII – Subdirección General de Redes y Centros de Investigación Cooperativa, expediente RD12/0018/0019.
Members of the +REDIVI Collaborative Network (alphabetical order): Paloma Aguilera (Centro de Atención Primaria Guayaba, Madrid), José María Cuadrado (Hospital Universitario San Juan de Alicante), Juan Antonio Cuadros (Hospital Universitario Príncipe de Asturias, Alcalá de Henares, Madrid), Ángel Domínguez (Hospital Universitario Virgen de La Macarena de Sevilla), Rubén Gálvez (Hospital Universitario San Cecílio de Granada), Magdalena García (Consorcio Hospital General Universitario de Valencia), Jordi Gomez i Prat (Unitat de Salut Internacional Drassanes, Barcelona), Esteban Martín Echevarría (Hospital Unversitario de Guadalajara), María Martínez (Complejo Hospitalario Universitario de Albacete), Ana Mena Ribas (Hospital Universitario Son Espases, Palma de Mallorca), Israel Molina (Hospital Universitario Vall d’Hebró de Barcelona), Begoña Monge (Hospital Universitario Ramón y Cajal. Madrid), Adriá Sanchez Montalvá (Hospital Universitario Vall d’Hebró de Barcelona), Marta Mora-Rillo (Hospital Universitario La Paz-IdiPaz. Madrid), Liliana M. Moreno Velazquez (Hospital Universitario Ramón y Cajal. Madrid), Ana Pérez de Ayala (Hospital Universitario 12 de Octubre, Madrid), Diana Pou (Unitat de Salut Internacional Drassanes, Barcelona), Azucena Rodríguez Guardado (Hospital Universitario Central de Astúrias, Oviedo), Fernando Salvador (Hospital Universitario Vall d’Hebró de Barcelona), Antoni Soriano (Unitat de Salut Internacional Drassanes, Barcelona), Inés Suárez (Hospital Infanta Sofía), Philip Wikman (Hospital Universitario San Juan de Alicante), Miren Zuriñe Zuberu (Hospital Universitario Basurto de Bilbao, Bizkaia).