Osteoporosis is a leading cause of morbidity and mortality in the elderly and influences quality of life, as well as life expectancy. Currently, there is a growing interest among the medical scientists in search of specific nutrients and/or bioactive compounds of natural origin for the prevention of disease and maintenance of bone health. Although calcium and vitamin D have been the primary focus of nutritional prevention of osteoporosis, a recent research has clarified the importance of several additional nutrients and food constituents. Based on this review of the literature, supplementation with vitamins B, C, K, and silicon could be recommended for proper maintenance of bone health, although further clinical studies are needed. The results of studies on long-chain polyunsaturated fatty acids, potassium, magnesium, copper, selenium, and strontium are not conclusive, although studies in vitro and in animal models are interesting and promising.
La osteoporosis es una de las principales causas de morbimortalidad en ancianos y tiene repercusiones en la calidad y esperanza de vida. Actualmente existe un interés creciente por parte de los investigadores médicos en los nutrientes y compuestos bioactivos de origen natural que puede ser útiles para la prevención de la enfermedad y el mantenimiento de la salud ósea. Si bien el calcio y la vitamina D han sido los nutrientes más destacados en la prevención de la osteoporosis, investigaciones recientes han aportado información sobre la importancia de otros nutrientes y componentes alimentarios. En base a esta revisión de la literatura, se puede recomendar la suplementación con vitaminas B, C, K y silicio para el mantenimiento adecuado de la salud ósea, aunque se necesitan más estudios clínicos. Los resultados de estudios sobre la cadena larga de ácidos grasos poliinsaturados, potasio, magnesio, cobre, selenio, estroncio no son concluyentes, aunque los estudios in vitro y en modelos animales son interesantes y prometedores.
Osteoporosis is a leading cause of morbidity and mortality in the elderly.1 In the United States of America, an estimated 4–6 million women aged >50 years have osteoporosis, and another 13–17 million (37–50%) have osteopenia (or low bone density) based on femoral bone mineral density (BMD) tests using dual X-ray absorptiometry (DEXA) when osteoporosis is defined by a T-score of less than −2.5 while osteopenia is defined as a bone mineral density T-score between −1.0 and −2.5.1
Regarding the prevalence of osteoporosis in Europe, by the year 2050 the number of men and women estimated to be affected will be more than 30 million in the EU.2
In England and Wales, it is estimated that there are 0.95 million women suffering from osteoporosis3 and in Sweden approximately 6% of men and 21% of women aged 50–84 years are classified as having osteoporosis.4
Osteoporosis influences quality of life as well as life expectancy5 because the major consequence of osteoporosis is fractures, and especially hip fractures are associated with institutionalization and increased mortality. In 2000, approximately 9 million fractures occurred worldwide, leading to a loss of 5.8 million disability adjusted life-years (DALYs).6 Due to a rise in life expectancy, the economic burden of osteoporotic fractures in Europe is expected to increase substantially in the coming decades: from 36.3€ billion in 2000 to 76.8€ billion in 2050.7
There are numerous categories of drugs used to treat osteoporosis; these medical approaches have been associated with serious side effects such as osteonecrosis of the jaw in patients receiving oral bisphosphonates,8 and increased risks of breast cancer, stroke, and venous thromboembolism in women treated with postmenopausal hormone replacement therapy.9 With respect to osteopenia, this is not a disease, but a statistical risk class. Osteopenia does not have any particular diagnostic or therapeutic significance. It was meant to show a huge group who looked like they might be at risk, but intervention due to prevention of osteoporosis is a crucial key point in this group of subjects at risk.
Given this background, currently, among medical scientists there is a growing interest in the search for specific nutrients and/or bioactive compounds of natural origin for the prevention of disease and maintenance of health.10Although calcium and vitamin D have been the primary focus of nutritional prevention of osteoporosis,11 recent research has clarified the importance of several additional nutrients and food constituents. The process of bone formation requires an adequate and constant supply of nutrients, and a large amount of literature suggests that numerous nutrients may have an interesting preventive activity in the management of osteopenia and osteoporosis.12–14
However, dietary intervention studies in humans, investigating the effect of the numerous nutrients involved in bone health, have yielded mixed and contrasting results. The main problem is related to the heterogeneity of the populations studied. In fact, these studies have been carried out on very different population groups: men and/or pre-, peri- or early postmenopausal women (≤5 years after menopause) or late postmenopausal women (>5 years after menopause), with very different ages and very different values of bone mineral density, with different sites of detection.
Moreover, another significant problem concerns the effectiveness indicators used in different studies: some studies use blood markers of bone turnover, some use blood markers of bone resorption, and others blood markers of bone formation or different values of bone mineral density, measured with DEXA and, in this case, there is difference regarding the site of detection. Finally, there is a significant difference in the duration of the studies: from a few months to several years. Additionally, studies on nutrients related to the prevention of bone fractures as the primary outcome are scarce and conflicting.
Given this background, with regard to human intervention studies, only the following studies will then be taken into account in the review: (1) Randomized, placebo-controlled, double-blind studies carried out for longer than one year. (2) Only those studies assessing mineral bone density by DEXA or bone fracture prevention as effectiveness indicators. (3) Studies using the sample size calculation for the population considered.
The aforementioned duration of the intervention study has been established considering that the bone-remodeling cycle ranges from 30 to 80 weeks according to Heaney's simulation model.15
With respect to in vitro and animal models studies, the most significant studies that clearly explain the effects of specific nutrients on bone health will be taken into consideration.
Finally, in the review, in addition to randomized, placebo-controlled, double-blind studies, only the studies with the following features will be taken into account: the largest cross sectional study that investigates the association between the dietary intake of specific nutrients and bone mineral density, as well as the largest cross sectional study using retrospective diet and nutrients supplement data and the studies that evaluated associations of nutrient intake (total, dietary and supplemental) with incident hip fracture and nonvertebral osteoporotic fracture.
Vitamin CA significant association that remained significant after adjustment for many of the important confounding factors was found between intakes of vitamin C and BMD.16–19 Vitamin C (ascorbic acid) is a vital component in the biology of bone cells and resultant bone mass, because it is the required coenzyme in the hydroxylation of proline and lysine during collagen synthesis in osteoblasts (bone cells).20,21
There are two relevant cross-sectional studies in humans on the effect of vitamin C supplementation on BMD. Morton et al.22 studied 994 postmenopausal women, in which 277 of them were regularly taking vitamin C support. Daily intake of vitamin C was 100–5000mg (average 745mg) and the average of duration of intake was 12.4 years; 85% of them reported that they were taking vitamin C support for more than 3 years. The results of this study showed that vitamin C intake has beneficial effects in BMD, especially if they are combined with hormone therapy. In this study, optimal doses were not determined, but best results (high BMD level) were by obtained for those taking 1000mg/day or higher (Table 1).
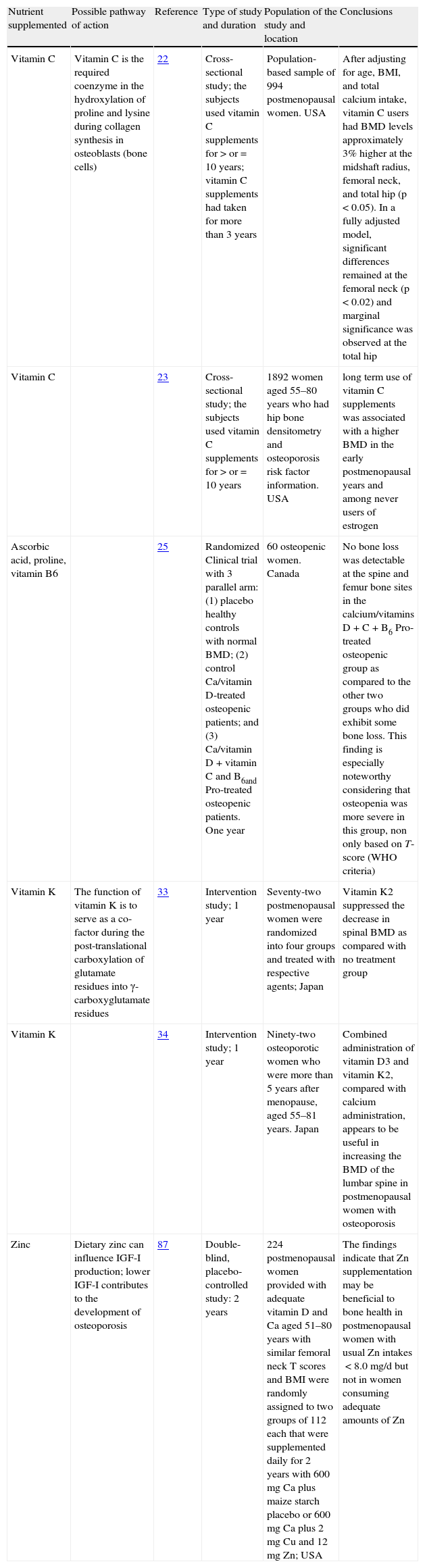
Intervention studies with dietary supplements in humans.
| Nutrient supplemented | Possible pathway of action | Reference | Type of study and duration | Population of the study and location | Conclusions |
| Vitamin C | Vitamin C is the required coenzyme in the hydroxylation of proline and lysine during collagen synthesis in osteoblasts (bone cells) | 22 | Cross-sectional study; the subjects used vitamin C supplements for>or=10 years; vitamin C supplements had taken for more than 3 years | Population-based sample of 994 postmenopausal women. USA | After adjusting for age, BMI, and total calcium intake, vitamin C users had BMD levels approximately 3% higher at the midshaft radius, femoral neck, and total hip (p<0.05). In a fully adjusted model, significant differences remained at the femoral neck (p<0.02) and marginal significance was observed at the total hip |
| Vitamin C | 23 | Cross-sectional study; the subjects used vitamin C supplements for>or=10 years | 1892 women aged 55–80 years who had hip bone densitometry and osteoporosis risk factor information. USA | long term use of vitamin C supplements was associated with a higher BMD in the early postmenopausal years and among never users of estrogen | |
| Ascorbic acid, proline, vitamin B6 | 25 | Randomized Clinical trial with 3 parallel arm: (1) placebo healthy controls with normal BMD; (2) control Ca/vitamin D-treated osteopenic patients; and (3) Ca/vitamin D+vitamin C and B6and Pro-treated osteopenic patients. One year | 60 osteopenic women. Canada | No bone loss was detectable at the spine and femur bone sites in the calcium/vitamins D+C+B6 Pro-treated osteopenic group as compared to the other two groups who did exhibit some bone loss. This finding is especially noteworthy considering that osteopenia was more severe in this group, non only based on T-score (WHO criteria) | |
| Vitamin K | The function of vitamin K is to serve as a co-factor during the post-translational carboxylation of glutamate residues into γ-carboxyglutamate residues | 33 | Intervention study; 1 year | Seventy-two postmenopausal women were randomized into four groups and treated with respective agents; Japan | Vitamin K2 suppressed the decrease in spinal BMD as compared with no treatment group |
| Vitamin K | 34 | Intervention study; 1 year | Ninety-two osteoporotic women who were more than 5 years after menopause, aged 55–81 years. Japan | Combined administration of vitamin D3 and vitamin K2, compared with calcium administration, appears to be useful in increasing the BMD of the lumbar spine in postmenopausal women with osteoporosis | |
| Zinc | Dietary zinc can influence IGF-I production; lower IGF-I contributes to the development of osteoporosis | 87 | Double-blind, placebo-controlled study: 2 years | 224 postmenopausal women provided with adequate vitamin D and Ca aged 51–80 years with similar femoral neck T scores and BMI were randomly assigned to two groups of 112 each that were supplemented daily for 2 years with 600mg Ca plus maize starch placebo or 600mg Ca plus 2mg Cu and 12mg Zn; USA | The findings indicate that Zn supplementation may be beneficial to bone health in postmenopausal women with usual Zn intakes<8.0mg/d but not in women consuming adequate amounts of Zn |
Abbreviations: BMI: body mass index; BMD: bone mineral density; Ca: calcium; Cu: copper; IGF-I: insulin-like growth factor – 1; United States of America (USA); zinc (Zn); World Health Organization (WHO).
The study of Leveille et al.23 demonstrated that long-term use of vitamin C supplements was associated with higher bone density in women who were 55–64 years old and in women who had never used estrogen (Table 1).
There is only one study that evaluated associations of vitamin C intake (total, dietary and supplemental) with incident hip fracture and nonvertebral osteoporotic fracture, over a 15–17-y follow-up.24 This is the Framingham Osteoporosis Study that demonstrated that subjects in the highest tertile of total vitamin C intake had significantly fewer hip fractures and non-vertebral fractures compared to subjects in the lowest tertile of intake. Subjects in the highest category of supplemental vitamin C intake had significantly fewer hip fractures and non-vertebral fractures compared to non-supplement users. Dietary vitamin C intake was not associated with fracture risk. These results suggest a possible protective effect of vitamin C supplementation on bone health in older adults.
There are only two intervention studies with vitamin C supplementation. However, in both studies, vitamin C was in association with other nutrients. In the first study, vitamin C was taken for 1 year, by osteopenic women in conjunction with calcium, vitamin D, proline and pyridoxine.25 In this study, middle-aged women not using estrogen were screened for osteopenia using the World Health Organization criteria and divided into three groups (n=20 each): (1) placebo healthy controls with normal bone mineral density (BMD); (2) control calcium/vitamin D-treated osteopenic patients; and (3) calcium/vitamin D+vitamin C and vitamin B6 and prolyne-treated osteopenic patients. No bone loss was detectable at the spine and femur bone sites in the calcium/vitamin D+vitamin C and vitamin B6 and prolyne-treated osteopenic group as compared to the other two groups who did exhibit some bone loss (Table 1). In the second study,26 Ruiz-Ramos et al. suggest that the administration of 1000mg of ascorbic acid together with 400IU of alpha-tocopherol could be useful in preventing or aiding in the treatment of age-related osteoporosis in a sample of 90 elderly subjects.
Studies in animal models confirm these data. Arsla et al. demonstrated that in ovariectomized rats (ovariectomy may produce osteoporosis), vitamin C supplementation may prevent worsening of BMD values.27
Finally, as regards in vitro studies, vitamin C is a known potent antioxidant that could reduce effects of free radicals,28 and antioxidants have been shown in laboratory studies to limit bone resorption.29
In conclusion, a cross-sectional study reported interesting results, showing a correlation between intake and supplementation of vitamin C and BMD. Moreover, recently, the Framingham Osteoporosis Study demonstrated a protective effect against fracture with supplemental vitamin C in a population of elderly Caucasian men and women. Finally, increased bone mineral density has been noted in postmenopausal women taking vitamin C supplements. More studies are needed to examine these associations in other populations and to further investigate this issue.
Vitamin KThe epidemiologic studies assessing different markers of vitamin K status (dietary vitamin K and/or blood levels of vitamin K) consistently support a role for vitamin K in the maintenance of bone health and reduction in fracture risk,30 although the data are not consistent for all ethnic groups.31
In the Framingham Offspring Study, a relevant cross-sectional study, Booth et al.32 reported a significant positive association between vitamin K intake and spine and hip BMD in women. As regards the intervention study in humans, Iwamoto et al. demonstrated that a vitamin K2 supplement suppressed the decrease in spinal BMD, as compared with no treatment group in postmenopausal women (Table 1).33
The effect of vitamin K and D supplementation on BMD was compared with the effect of calcium and vitamin D by Iwamoto et al.34 The results of this study indicate that combined administration of vitamin D3 and vitamin K2, compared with calcium administration, appears to be useful in increasing the BMD of the lumbar spine in postmenopausal women with osteoporosis (Table 1).
As for long-term intervention studies, the 4-year ECKO trial demonstrated that daily vitamin K1 supplementation does not protect against age-related decline in BMD, but may protect against fractures and cancers in postmenopausal women with osteopenia.35
The evidence summarized in a meta-analysis confirms the results of ECKO trial and suggests that phylloquinone is associated with a significant reduction in the risk of clinical fractures in postmenopausal women with osteopenia, but without osteoporosis.36
Remarkably, throughout the literature the association between vitamin K status and fracture incidence seems to be more evident than the effects on bone mineral density (BMD). Moreover, vitamin K intervention studies have shown contradictory results, with some studies showing a positive effect on bone health (as measured by BMD) and others with no measurable effect. A recent review on this topic argues that one explanation for these apparently contradictory results is that BMD is not an appropriate endpoint to monitor effects of vitamin K on bone health. Also, it should be realized that in epidemiological studies only poor vitamin K status is associated with increased fracture risk. It would be logical, therefore, to investigate the effect of vitamin K supplements on bone health in subjects pre-selected for poor dietary vitamin K status. However, no such studies have yet been published today.37
It is interesting to note that a recent state-transition probabilistic microsimulation model to quantify the cost-effectiveness of various interventions to prevent fractures in 50-year-old postmenopausal women without osteoporosis, demonstrates that adding vitamin K2 to vitamin D3 with calcium reduced the lifetime probability of at least one fracture by 25% and increased discounted survival by 0.7 QALYs.38
For the vitamin K–dependent proteins, conversion of glutamyl to γ-carboxyglutamyl conveys the ability to bind calcium ions and is essential for biological activity, according to in vitro studies.39 Since 3 vitamin K–dependent proteins (osteocalcin, matrix Gla-protein, and protein S) are present in bone40 and may play a role in bone metabolism,41,42 impaired function could potentially have adverse skeletal consequences. Specifically, subclinical vitamin K insufficiency might contribute to the development of osteoporosis.43
In conclusion, doses of 45mg/day have decreased fracture rates 37% which is similar to fracture decreases following treatment with bisphosphonates. However, lower fracture rates from vitamin K supplementation are not accompanied by increased bone mineral density.44 This suggests that vitamin K improves bone properties that increase bone strength without increasing mineral content. Vitamin K has no toxicity except for those using warfarin; thus, supplementation with 100 microgram/day would achieve slightly more than the recommended daily allowance and may have beneficial effects on bone structure.
B vitaminsVitamin B6 (pyridoxine)The Rottherdam study showed that increased dietary pyridoxine intake was associated with higher BMD. Furthermore, the same study found a reduction in the risk of fracture in relation to dietary pyridoxine intake independent of BMD.45 Moreover, low serum vitamin B6 concentrations are associated with an altered morphology of human bone.46
Vitamin B6 is involved as a coenzyme in the assembly process of collagen (aldehyde cross-link formation) in the extracellular matrix. Masse et al.’s biomechanical study demonstrated the importance of this extracellular process for the strength of bone using a vitamin B6-deficient animal model.47 As regards clinical studies, the study of Masse et al.25 demonstrated that in osteopenic women who were given a supplement of pyridoxine, vitamin C, vitamin D and prolyne no bone loss was detectable at the spine and femur bone sites as compared to the untreated groups that did exhibit some bone loss (Table 1). Another clinical study on this vitamin in relation to bone was reported by Reynolds et al.48 showed that half of their hip fracture patients were vitamin B6-deficient. In vitro studies have shown that low B vitamin concentrations stimulate osteoclasts.49
Moreover, in this contest it is important to remember the relationship between these vitamins and hyperhomocysteinemia (tHcy) that is considered a novel and potentially modifiable risk factor for age-related osteoporotic fractures.50 In fact folate, vitamin B2 (riboflavin), and vitamin B12 may affect bone directly or through an effect on plasma homocysteine levels. On multiple linear regression analysis, adjusting for age, body mass index, folates, vitamin B12, creatinine clearance, smoking habit and alcohol intake, tHcy was negatively related to BMD of the total femur in postmenopausal women.51 Another study confirmed this negative correlation.52
Homocysteine is a metabolite of the essential amino acid methionine. Folate, vitamin B6, and vitamin B12 are important coenzymes of the homocysteine-degrading remethylation and transsulfuration pathways.53 Accordingly, deficiencies of folate, vitamin B6, and vitamin B12 lead to an elevated serum concentration of homocysteine (hyperhomocysteinemia). In addition, B vitamins play a crucial role in the reduction of oxidative stress and in the methylation of different proteins.54
The hypothesis that tHcy may be a risk factor for fracture was suggested by studies of patients with homocystinuria, characterized by very high plasma levels of homocysteine. Among several clinical manifestations, these patients also have high incidence of premature osteoporosis and fractures.55 Investigations have been further motivated by studies showing that homocysteine inhibits the collagen cross-linking56 and impairs bone mineralization.57
Possible relation between levels of tHcy and BMD and fractures has large health implications because hyperhomocysteinemia responds to intake of B vitamins.58 However, a direct effect of folate status on bone tissue has been hypothesized,59 and a positive association between folate levels and lumbar spine BMD has previously been reported in postmenopausal women.59,60 Actually, there are no studies in the literature that have evaluated the effect of administration of adequate amounts of B vitamins on BMD, although, given the interest in this topic, a study to assess the efficacy of oral supplementation with B vitamins in the prevention of fractures in Dutch elderly people with elevated homocysteine concentrations is being conducted.61
In conclusion, the mechanistic in vitro and animal model studies support the hypothesis of a beneficial effect of homocysteine reduction by B-vitamins supplementation on fracture incidence and related outcome measures. However, evidence from randomized controlled trials (RCTs) is still limited, although, given the interest in this topic, a study aimed at assessing the efficacy of oral supplementation with B vitamins in the prevention of fractures in subjects with elevated homocysteine concentrations is under way.
MagnesiumA significant association that remained significant after adjustment for many of the important confounding factors was found between intakes of magnesium and BMD.16,62,63 It has been shown that magnesium (Mg) is essential for the normal function of the parathyroid glands, vitamin D metabolism, and adequate sensitivity of target tissues to parathormone (PTH) and active vitamin D metabolites.64 Therefore, Mg deprivation is regularly associated with hypoparathyroidism, low production of 1,25-dihydroxyvitamin D3 [1,25-(OH)2D3] and end-organ resistance to PTH and vitamin D. The combined effects of Mg deficiency on PTH and 1,25-(OH)2D3 synthesis and secretion could lead to hypocalcemia without the compensatory increase in PTH secretion.65 These Mg deficiency-associated adverse effects together could impair bone growth and mineralization66–68 and thereby could reduce bone quality, strength and density.69–71 Accordingly, Mg deficiency has been suggested to be a potential risk factor for osteoporosis.72,73 In this regard, postmenopausal osteoporosis in women is frequently associated with low dietary Mg intake74 and reduced serum and bone Mg levels.75,76
Two earlier reports, which indicated that Mg repletion in postmenopausal osteoporotic women significantly increased bone mass and reduced fracture rate,72,73 support the contention that Mg deficiency may be associated with osteoporosis. In particular, the study by Stendig-Lindberg et al. of women with osteoporosis in Israel reported significantly increased bone mineral density with 250mg/day of magnesium supplement when compared to a control group who did not take magnesium supplements.72
After this interesting study that had the drawback of not being a placebo-controlled trial, conducted in 1993, in 2012 Genuis et al. conducted another study to evaluate the effectiveness of magnesium supplementation on bone health. In this one year study the nutritional supplement included vitamin D3, vitamin K2, strontium, magnesium and docosahexaenoic acid (DHA).77
This combined micronutrient supplementation regimen appears to be at least as effective as bisphosphonates or strontium ranelate in raising BMD levels in hip, spine and femoral neck sites. No fractures occurred in the group taking the micronutrient protocol. This micronutrient regimen also appears to show efficacy in individuals where bisphosphonate therapy was previously unsuccessful in maintaining or raising BMD.
In conclusion, there are published studies linking Mg deficiency to osteoporosis. Also, modest supplementation with magnesium is reasonable to support bone health and for other aspects of general health.78
PotassiumFarrell et al. recently demonstrated that dietary potassium intakes were positively associated with BMD,79 confirming previous cross-sectional studies.16 Actually, there are no studies in the literature that consider the effectiveness of potassium supplementation on bone mineral density, except for a study on a specific group of subjects, i.e. idiopathic calcium stone formers.80
In the literature, there are only studies suggesting that treatment with potassium citrate can reduce bone resorption, thereby contrasting the potential adverse effects caused by chronic acidemia of protein-rich diets.81
In conclusion, cross-sectional studies demonstrated that dietary potassium intakes were positively associated with BMD, but to date, there are no RCTs in the literature that consider the effectiveness of potassium supplementation on bone mineral density.
ZincZinc (Zn) is essential for the growth, development, and maintenance of healthy bones.82 Zinc deficiency is associated with delayed skeletal growth and decreased bone mass in a variety of animal models,83 and zinc supplementation in children has been shown to stimulate both skeletal growth and maturation.82 In addition, zinc supplementation has been reported to reduce tissue lead deposition in animal models.84–86 A significant association that remained significant after adjustment for many of the important confounding factors was found between intakes of zinc and BMD.16,19,63 As regards clinical studies on zinc efficacy on BMD, the study of Nielsen et al. indicates that Zn supplementation may be beneficial to bone health in postmenopausal women with usual Zn intakes <80mg/d but not in women consuming adequate amounts of Zn (Table 1).87
In conclusion, cross-sectional studies demonstrated a significant association between intakes of zinc and BMD. To date, the studies have been shown that Zn supplementation may be beneficial to bone health in postmenopausal women with usual Zn intakes is deficient, but not in women consuming adequate amounts of Zn.
BoronRecently, Kaats et al. designed a study to compare the safety and efficacy of three bone health plans (containing different amounts of boron) using three independent sequentially enrolled groups of healthy women aged 40 years and older.88 The results of this study demonstrated an increase in BMD in all three treatment groups, but the group following the most nutritionally comprehensive plan outperformed the other two groups. As regards studies in animal models, the study by Amstrong et al. indicates that boron supplementation to pigs can increase growth and bone strength without greatly affecting calcium and phosphorus metabolism.89 There is, therefore, considerable evidence that dietary boron alleviates perturbations in mineral metabolism that are characteristic of vitamin D3 deficiency. The findings described in the review by Hunt90 lend support to the hypothesis that boron alleviates the symptoms of vitamin D3 deficiency by enhancing utilization or sparing minimal supplies of the active vitamin D3 metabolite. Also, boron and vitamin D3 have the same overall effect on the local utilization of energy substrates. A corollary of the hypothesis is that some of the effects of dietary boron will be overshadowed by the effects of adequate amounts of dietary vitamin D3.90
In conclusion, boron stabilizes and extends the half-life of vitamin D; therefore, future cross-sectional studies and RCTs are needed to better understand the potential of this interesting micronutrient on bone health.
SiliconIn 1970, Carlisle suggested that silicon is a possible factor in bone calcification,91 due to animal studies that reported that dietary silicon deficiency resulted in reduced bone tensile strength.92,93 More recently, a study by Kim et al. demonstrated that silicon supplementation produced positive effects on bone mineral density in calcium-deficient OVX rats by reducing bone resorption;94 in this study, silicon was shown to modulate the ratio of expression of two cytokines involved in bone formation-RANKL and osteoprotegerin. A more recent in vitro study, demonstrated that silica nanoparticles promote a significant enhancement of BMD in mice in vivo.95 In the Framingham offspring cohort, increased dietary silicon intake was associated with increased bone mass.96 As for studies in humans, silicon was shown to be more effective than etidronate and sodium fluoride over a 14 to 22 month period.97 In a recent double blind placebo-controlled 12-month trial in osteopenic and osteoporotic subjects, Spector et al.98 reported that oral choline-stabilized orthosilicic acid had potential beneficial effects on bone collagen and a trend for a dose-related decrease in the bone resorption marker, collagen type 1 C-terminal telopeptide at 6 and 12 months. Another interesting study99 demonstrated that, in postmenopausal women with low bone mass, but without osteopenia or osteoporosis, bottled water from artesian aquifers is a safe and effective way of providing easily absorbed dietary silicon to the body, although the research has been conducted for a short time (3 months). However, there are no RCTs that evaluate the effectiveness of silicon supplementation on bone mineral density in humans.
Some types of mineral water also contain silicon in the form of orthosilicic acid.100 Beer is a rich source of silicon because of the processing of barley and hops.101 Men consume more silicon than women and this is primarily due to differences in beer consumption.102 Post-menopausal women rarely achieve 40mg of silicon per day and average approximately 18mg per day.96,103 Also, post-menopausal women, as well as younger women, may not absorb silicon. Thus, silicon supplementation with approximately 20–30mg/day may benefit bone health for the majority of subjects who do not consume beer on a regular basis.
In conclusion, cross-sectional studies demonstrated that increased dietary silicon intake was associated with increased bone mass. To date there are no randomized trials on this issue; RCTs are warranted, given also the interesting in vitro, animal model and clinical studies.
Protein and specific amino acidsLong-term effects of high dietary protein intake on bone structure are not clear.104 A 5-year cohort study of the effects of high protein intake on lean mass and BMC in elderly postmenopausal women showed that there were positive correlations between baseline protein intake and whole body and appendicular bone-free lean mass and BMC. Compared with those in the lowest tertile of protein intake (<66g/d), women in the top tertile (>87g/d) had 5.4–6.0% higher whole body and appendicular lean mass and 5.3–6.0% higher whole body and appendicular BMC. These effects remained after adjusting for potential confounders. However, the effect on BMC disappeared after further adjustment for lean mass. This study shows that high protein intake is associated with long-term beneficial effects on muscle mass and size and bone mass in elderly women. The protein effect on bone may be partly mediated by its effects on muscle.105
On average, for every 50g increase in dietary protein, there is approximately a 1.6mmol increase in 24-h urinary calcium excretion.106 Indeed, some investigators have concluded that dietary protein is a more important regulator of urinary calcium than dietary calcium intake.107,108One mechanism by which high dietary protein could induce bone loss may be related to the metabolic acid load engendered by such a diet. Meat and fish, which are high in sulfur-containing amino acids, generate significant fixed metabolic acid loads, whereas fruits and vegetables generate little acid and, in fact, may under certain circumstances generate more base than acid. While renal metabolism represents the principal mechanism by which fixed metabolic acid loads are handled by the body, renal buffering may be incomplete, particularly with aging. Under those circumstances, the skeleton may be called on to act as a buffer to neutralize acid generated from high-protein diets. Liberation of buffer from bone comes at the expense of mineral dissolution and ultimately bone loss.109–111 Consistent with this hypothesis is the finding that the magnitude of urinary calcium excretion during a high-protein diet is dependent, to a large extent, on the sulfur amino acid content of the diet.112–114
However, additional balance studies have shown that higher protein intake leads to increased intestinal absorption of calcium.115 Thus, higher urinary calcium produced by high protein diets may reflect this enhanced calcium absorption and not bone resorption. In fact, previous studies have observed that subjects with greater protein intake had higher BMD and less bone loss, perhaps mediated through local production of insulin-like growth factor-1 (IGF-1) by amino acids arginine116 and lysine.117,118 Yakar et al. showed low levels of IGF-1 in mice was associated with decreased bone strength.119On the other hand, the long-term consequences of low-protein diet-induced changes in mineral metabolism are not known, but the diet could be detrimental to skeletal health. Of concern are several epidemiologic studies that demonstrate reduced bone density and increased rates of bone loss in individuals habitually consuming low-protein diets.120,121
With regard to individual amino acids, there are numerous studies on animal models, but very few human intervention studies. As for supplementation with arginine, it has been hypothesized that supplementation of l-arginine may be a novel strategy in the prevention and treatment of osteoporosis, because l-arginine can be converted to produce nitric oxide (NO), that slows bone remodeling and bone loss in animal and human studies.122 This hypothesis has been confirmed by many studies in animal models,123–125 while there is still no confirmation in human studies because the studies conducted to date do not have an adequate sample size and were conducted without comparison to placebo.126,127 In addition, Hurson et al. showed that supplementation with l-arginine leads to a significant increase in serum IGF-1 concentration.128 Several studies have shown that serum levels of IGF-1 are significantly correlated with BMD, cross-sectional area of the femur, and risk of hip fractures. Arginine is a semi-essential amino acid involved in multiple areas of human physiology and metabolism. Arginine is the biologic precursor of NO, an endogenous messenger molecule involved in a variety of endothelium dependent physiological effects. Several co-factors are required for NO biosynthesis. Flavin adenine dinucleotide, flavin mononucleotide, and (6R)5,6,7,8-tetrahydrobiopterin (BH(4)) are essential cofactors required for the activity of NO synthase (NOS). Nitric oxide synthases are a family of enzymes that catalyze the production of nitric oxide from l-arginine. Recent reports suggest that vitamin C may prevent endothelial dysfunction by scavenging free radicals and increasing the bioavailability of nitric oxide.129,130 Studies in cultured vascular endothelial cells demonstrated that vitamin C increases NOS activity by increasing availability of BH4.129,131,132 A more recent study showed that the beneficial effect of vitamin C on vascular endothelial function appears to be mediated in part by protection of tetrahydrobiopterin and restoration of NOS enzymatic activity.133 Vitamin B2 (riboflavin) is a precursor of certain essential coenzymes such as flavin mononucleotide and flavin adenine dinucleotide. In these coenzyme forms riboflavin functions as a catalyst for oxidation and reduction reactions and electron transport.134
Concerning the activity of glutamate on bone health, a recent review highlighted that glutamate could play a pivotal role in mechanisms underlying the maintenance of cellular homeostasis as an extracellular signal mediator in bone.135 In fact, an in vitro study shows that l-glutamate promotes the stimulation of osteoblast differentiation by N-methyl-d-aspartate receptor activation.136 No studies have been conducted in humans.
In conclusion, rather than having a negative effect on bone, protein intake appears to benefit bone status, particularly in older adults. A moderate intake of proteins (1g/kg/day) is associated with normal calcium metabolism and presumably does not alter bone turnover. With regard to individual amino acids, it has been hypothesized that supplementation of l-arginine may be a novel strategy in the prevention and treatment of osteoporosis, because l-arginine can be converted to produce NO, that slows bone remodeling and bone loss in animal and human studies and leads to a significant increase in serum IGF-1 concentration.
Long-chain polyunsaturated fatty acidsDietary long-chain polyunsaturated fatty acids (LCPUFAs) are incorporated into cell membranes within the body. The composition of LCPUFAs in the diet is reflected in the fatty acid composition of a variety of body tissues and fluids, including bone marrow, the periosteum and bone.137 There is evidence from animal models that omega-3 fatty acids inhibit osteoclast activity and promote osteoblast activity, thus favoring bone formation over bone resorption. Animal studies also suggest that LCPUFAs potentiate the effects of estrogen on bone, reduce bone loss during estrogen deficiency, and moderate peripheral peroxisome activated receptor gamma (PPAR-γ), which influences the marrow adiposity that accompanies osteoporosis.138 It appears that the omega-6/omega-3 ratio may be important, in addition to the absolute quantities of omega-3 fatty acids ingested.139 Lipid metabolism differs between animals and humans, so data cannot always be easily extrapolated from these animals to humans.140 To date, human studies concerning omega-3 and omega-6 fatty acids and bone health are limited, no RCTs included fracture as an outcome with some suggesting an effect on calcium absorption, bone turnover, peak bone mass and postmenopausal bone loss.141–145 A recent interesting metanalysis146 showed strong conclusions regarding n-3 FAs and bone disease are limited, due to the small number and modest sample sizes of RCTs; however, it appears that any potential benefit of omega 3 fatty acids on skeletal health may be enhanced by concurrent administration of calcium.
In conclusion, some epidemiological evidence suggests that diets high in LCPUFAs may be beneficial for skeletal health, but to date no RCTs support a positive effect of n–omega 3 fatty acids on osteoporosis.
Other minerals: Selenium, strontium and copperSeleniumSelenium deficiency is detrimental to bone microarchitecture by increasing bone resorption, possibly through decreasing antioxidative potential.147
An inverse dose-response association between intakes of selenium and the risk of hip fracture was observed among ever smokers in an elderly Utah population. Ever smokers in the highest quintile of intakes of selenium had 73% lower risks of hip fracture than those in the lowest quintile.148
However, Melhus et al. and Wolf et al. did not find an association between low compared with high intakes of dietary selenium and risk of hip fracture. Those findings are not surprising, given that there is probably too little selenium in our bodies to act as a direct antioxidant without the use of supplements.149,150
In the evaluation of antioxidant supplement safety, it is important to acknowledge that the process of oxidative stress is not just equated with adverse consequences and that the generation of byproducts of oxidative stress are natural and can be beneficial, such as, signal transduction via modulation of kinases or phosphatases and transcription factor activation leading to cell growth, proliferation, and apoptosis.
StrontiumStrontium is increasingly being recognized as a trace mineral which may be essential to the normal biology of bone and teeth and it is yet undetermined if strontium deficiency, like iodine deficiency, results in physiological malfunction. Thus, the restoration of adequate strontium levels to individuals may simply represent the normal homeostatic requirement for strontium, and normal healthy bone may require some level of strontium to prevent calcium loss.151
At low supplemental doses of strontium, in fact, there is evidence of an increase in both bone formation rate and the trabecular bone density related to a strontium-induced stimulation of osteoblastic activity.152 Furthermore, at low doses, strontium is not associated with any mineralization defect or any increase in the number of active bone-resorbing cells.153,154 In addition, it has recently been found that the mechanism of strontium benefit may also involve a calcium preservation effect as the rate of calcium release was almost halved after strontium treatment was assessed in recent research on teeth.151 Finally, strontium supplementation, unlike use of calcium supplementation, shows the ability to recalcify osteopenic areas in pathological bone conditions characterized by accelerated bone loss and extensive demineralization.152,155
CopperCopper is essential for normal development of the skeleton in humans and animals.156–158 There is no cross sectional or RCTs in literature on copper intake or supplementation and BMD.
In conclusion, to date, randomized controlled trials on effect of supplementation with selenium, strontium, copper and BMD are scarce and so the results not conclusive, although studies in vitro and in animal models are interesting and promising.
General concluding remarksPharmacological interventions may prevent 30–60% of fractures in patients with osteoporosis.159 However, due to the high prevalence of osteoporosis and osteoporotic fractures, attention has been shifted toward preventive lifestyle interventions, such as vitamin D and calcium supplementation and promoting physical activity. Supplementation of vitamin D and calcium was shown to decrease the incidence of hip fractures and other non-vertebral fractures by 23–26%.11 Increased physical activity is related to higher BMD, bone structure and elasticity160,161 and is suggested to reduce the risk of hip fracture.162
Despite the fact that several recent reviews stress the importance of certain nutrients in the protection of the bone, the literature on the clinical intervention studies in humans is low, debated and often dated.
A crucial point concerns the difficulty of identifying the specific effect of single individual elements of diets. Biochemicals in their natural physiological state as produced in foods or gut microbiota do not work in isolation. Combinations of nutrients are known to be required for normal biochemical function. In addition, emerging evidence suggests that other nutrients including some phytochemicals may contribute to the constellation of factors involved in healthy bone biochemistry.
In addition to identifying the role of individual components, there is a great need to understand the interactions of these factors within diets and, increasingly, in the presence of nutrient supplements. Furthermore, genetic factors are likely to interact with these dietary exposures, increasing the complexity of these effects. With advances in both genetics and nutrition, improved understanding of all these interactions will contribute to effective recommendations for prevention of bone loss and osteoporosis in the aging population.
The intake, through diet or supplements, of adequate amounts of certain vitamins and minerals is certainly a key point for the prevention of BMD loss and is a crucial support to the drugs in the treatment of osteoporosis. Adequate dietary intake is essential and supplementation should be considered in subjects with documented malabsorption syndromes or deficiencies.
It is important to note that the effects of interventions in healthy subjects cannot be extrapolated to subjects with osteoporosis.
The effectiveness of the use of supplemental nutrients for osteoporosis therapy remains controversial, because studies in double-blind comparison with drugs are scarce. As regards osteopenia, certainly today there is evidence of how the intake of dietary supplements of vitamin K can slow the loss of bone mineral density.
Based on this review of the literature, supplementation with vitamins B, C, K, and silicon can be recommended for proper maintenance of bone health, although further clinical studies are needed. The results of studies on long-chain polyunsaturated fatty acids, potassium, magnesium, copper, selenium and strontium are not conclusive, although studies in vitro and in animal models are interesting and promising.
As regards macronutrients, rather than having a negative effect on bone, protein intake appears to benefit bone status, particularly in older adults. A moderate intake of proteins (1g/kg/day), is associated with normal calcium metabolism and presumably does not alter bone turnover.
Programs to increase awareness of osteoporosis and its outcomes are necessary for healthcare specialists and the general public. Earlier diagnosis and intervention prior to the first fracture are highly desirable and the use of specific dietary supplement may be useful. Further RCTs should be carried out on this topic.
Conflict of interestThe authors declare no conflict of interest.